Value of plasma neutrophil to lymphocyte ratio in predicting prognosis after half a year in acute ischemic stroke patients with mechanical thrombectomy
-
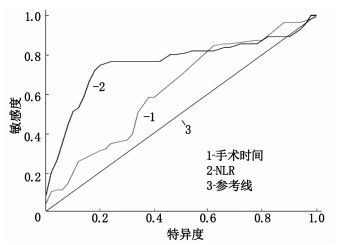
摘要:目的 探讨血浆中性粒细胞与淋巴细胞比值(NLR)预测急性缺血性脑卒中(AIS)机械取栓患者半年预后的价值。方法 将105例AIS机械取栓患者根据半年后改良Rankin量表(mRS)评分结果分为预后良好组48例和预后不良组57例,比较2组患者的临床资料。将有统计学差异的相关指标采用二元Logistic回归分析,采用受试者工作特征(ROC)曲线评估预测价值。结果 预后良好组与预后不良组手术时间、中性粒细胞百分比、淋巴细胞百分比及NLR比较,差异有统计学意义(P < 0.05)。前循环梗死组与后循环梗死组手术时间、入院美国国立卫生研究院卒中量表(NIHSS)比较,差异有统计学意义(P < 0.05)。颈内动脉闭塞组与大脑中动脉闭塞组相关临床资料比较,差异无统计学意义(P>0.05)。二元Logistic回归分析结果显示,手术时间、NLR是预测急性脑梗死机械取栓患者半年预后的独立危险因子。NLR判断急性脑梗死取栓半年预后的ROC曲线下面积(AUC)为0.759, 当最佳临界值为4.685时,其约登指数为0.565, 敏感度为74.50%, 特异度为82.00%, 95%CI为0.662~0.855。手术时间判断急性脑梗死取栓半年预后的AUC为0.623, 当最佳临界值为81.500 min时,其约登指数为0.245, 敏感度为74.50%, 特异度为50.00%, 95%CI为0.516~0.731。结论 血浆NLR的升高对AIS机械取栓半年不良预后有较好的预测价值。
-
关键词:
- 急性缺血性脑卒中 /
- 机械取栓 /
- 中性粒细胞与淋巴细胞比值 /
- 预后
Abstract:Objective To explore the value of plasma neutrophil to lymphocyte ratio (NLR) in predicting prognosis after half a year in acute ischemic stroke (AIS) patients with mechanical thrombectomy.Methods Totally 105 AIS patients with mechanical thrombectomy were divided into good prognosis group (n=48) and poor prognosis group (n=57) according to the score of modified Rankin Scale (mRS) after half a year, and the clinical materials were compared between the two groups. Binary Logistic regression analysis was used to analyze the related indicators with statistical differences, and the receiver operating characteristic (ROC) curve was used to evaluate the predictive value.Results There were significant differences in operation time, neutrophil percentage, lymphocyte percentage and NLR between the two groups (P < 0.05). There were significant differences in operation time and National Institute of Health Stroke Scale (NIHSS) between anterior circulation infarction group and posterior circulation infarction group (P < 0.05). There was no significant difference in clinical materials between internal carotid artery occlusion group and middle cerebral artery occlusion group (P>0.05). Binary Logistic regression analysis showed that operation time and NLR were independent risk factors for predicting prognosis after half a year in acute cerebral infarction patients with mechanical thrombectomy. The area under the ROC curve (AUC) of NLR in predicting prognosis after half a year in acute cerebral infarction patients with mechanical thrombectomy was 0.759. When the optimal critical value was 4.685, the Youden index was 0.565, the sensitivity was 74.50%, the specificity was 82.00%, and the 95% CI was from 0.662 to 0.855. The AUC of operation time in predicting prognosis after half a year in acute cerebral infarction patients with mechanical thrombectomy was 0.623. When the optimal cut-off value was 81.500 min, the Youden index was 0.245, the sensitivity was 74.50%, the specificity was 50.00%, and the 95% CI was from 0.516 to 0.731.Conclusion The increase of plasma NLR has a good predictive value for the poor prognosis after half a year in AIS patients with mechanical thrombectomy. -
自然灾害是一种极端事件,一般由突然气候变化和其他环境因素造成[1]。根据国际紧急灾难数据库(EMDAT)数据,从1900年到2017年,世界遭受重大自然灾害的死亡人数为22 989 400人[2]。这些自然灾害中洪涝灾害发生最频繁,导致的死亡人数最高[3]。洪涝灾害会给受灾群众带来严重精神心理伤害[4-5], 尤其是经历自然灾害的青少年,特殊的经历对其心理健康的影响至关重要[6], 易出现一定的创伤后应激障碍(PTSD)[7-8]。2021年7—8月中国河南郑州和新乡等地发生重大洪涝灾情,是有记录以来最严重的一次洪涝灾害[9]。本研究采用定性研究方法对经历此次洪涝灾情的青少年进行访谈,获得青少年真实心理体验,以期为探讨和建立重大洪涝自然灾害对青少年心理行为影响的预测和干预研究提供依据。
1. 资料与方法
1.1 一般资料
采用目的抽样法选取河南省新乡市卫辉市2021年7—8月经历洪涝灾害的12~18岁在校读书青少年为研究对象。纳入标准: ①河南新乡卫辉籍者; ②在校初中或高中学生,年龄12~18岁者; ③经历2021年7—8月洪涝灾害者。纳入研究的青少年均知情同意,自愿参与本研究。排除不在校的青少年或有沟通障碍的在校学生。样本量以达到资料饱和为标准[10]。本研究最终共纳入12名青少年,一般资料见表 1。
表 1 12例受访者一般资料情况编号 年级 出生日期 性别 民族 是否是独生子女 学习成绩班级排名 家庭月收入/元人民币 是否去过安置点 母亲文化程度 父亲文化程度 S1 八年级 2008.03.20 女 回族 是 中等偏下 3 000~5 000 否 中专 高中 S2 七年级 2007.10.17 男 汉族 否 中等偏下 8 000以上 是 高中 中专 S3 高一 2005.08.10 女 汉族 否 一般 3 000~4 000 是 高中 初中 S4 高二 2004.10.09 女 汉族 否 前10名 5 000~6 000 是 初中 高中 S5 高三 2003.08.20 男 汉族 否 前10名 8 000以上 否 大学及以上 大学及以上 S6 九年级 2006.03.28 女 汉族 否 一般 5 000~6 000 否 初中 小学 S7 高二 2005.04.26 女 汉族 否 中等偏上 2 000~3 000 否 高中 初中 S8 高三 2004.03.22 女 汉族 否 中等偏上 8 000以上 否 大学及以上 大学及以上 S9 高一 2005.08.24 男 汉族 否 一般 3 000~4 000 否 小学 高中 S10 八年级 2008.05.28 男 汉族 否 中等偏下 2 000~3 000 是 初中 初中 S11 七年级 2008.04.01 男 汉族 否 中等偏下 2 000~3 000 是 初中 初中 S12 九年级 2006.09.19 男 汉族 否 中等偏上 6 000~7 000 是 初中 初中 1.2 研究方法
采用质性研究的现象学方法进行研究。基于研究目的,在查阅文献的基础上,经课题组成员讨论并咨询儿童青少年卫生领域专家后形成访谈提纲,以半结构式访谈法进行问题的设计。设计包括2个部分: 以封闭式问卷设计了解受访者基本情况特征,如年龄、性别、家庭月收入、是否去过安置点、财产损失、父母学历等; 半开放性问题以青少年对洪涝灾害的认知和心理行为体验为主,包括5个方面问题: ①你经历洪水当时,你主要的心情是什么?②你现在想起洪水的心情是什么?③你现在是否经常想起当时洪水的情形?④经历这次洪水后,你主要的感想是什么?⑤洪水期间你在干什么?访谈过程中鼓励青少年表达自己的观点、体验和感受,根据访谈情况和受访者的情绪适当调整谈话内容及方式。
1.3 伦理学问题
接受调查前先告知受访者调查目的,并征得其同意,由访谈者首先登记其一般人口学资料。访谈过程中,受访者有权因任何原因拒绝谈论某个问题或中途退出,但在整个研究过程中未出现这种情况。如果个别受访者参加讨论之后出现情绪问题,访谈者会为其提供针对性心理支持服务。
1.4 资料收集及分析
访谈前,首先向受访者介绍采访目的,并征得其同意。受疫情的影响,以网络腾讯会议的方式进行访谈,并全程录屏。录屏时向受访者解释清楚,尽量避免因录屏造成受访者紧张。了解受访者基本情况后,以半开放性问题与受访者进行交流。访谈中不设特定的封闭式问题,并适当施加引导,以获取更多受访者的真实感受和体验,同时观察受访者细微表情变化并做好记录。每例访谈约20 min。访谈结束后,收集所有受访者的资料并仔细阅读,将资料输入计算机,根据提纲设计的问题对资料进行总结和分析。资料的分析采取Colaizzi现象学资料分析步骤进行阅读记录,回放并分析其含义,选取有重要意义的陈述,阐述观点[11]。访谈结束24 h内,由2名研究者将音频文件逐字转为文字,分析所有资料,保证资料分析的准确性。最后应用Nvivo11.0软件进行分类编码,提取主题。
2. 结果
2.1 主题1: 经历洪涝灾害的青少年的主要负性心理体验
河南新乡地处华北平原,远离沿海,经历洪涝灾害千年不遇, 12~18岁的青少年生活在中国城镇化高速发展时期,生活物质及自然环境条件比较优越,经历这次突发事件以负性心理体验为主。
① 恐惧和悲伤。访谈中,经历洪涝灾害的青少年主要心理体验为“恐惧”和“悲伤”。受灾青少年S12: “昨天我们街道水不多,突然水多了起来,深度齐腰,若不是救援人员,我们都会被淹死,太可怕了。”S8: “我家地势比较低,是最先被淹的地方,水都到了屋顶,我不在家,我妈妈去了安置点,她一直情绪不好,家里的猪也都淹死了,我很害怕妈妈会一直难过。”受灾青少年S9: “家里新买的院子,刚装修完,凝结了父母一辈子的心血,一天都没有住,所有的家具、家电全部坏了,太难过了。”受灾青少年S4: “我家的地都被淹了,今年庄稼肯定没有收成了,还搭进去了种子和人力,我很难过,也不知道怎么安慰爸爸妈妈。”
② 无奈。访谈中出现频率较高的是“无奈”和“复杂”。受灾青少年S1: “看到受灾后街上充斥大量的损坏的家具、家电和恶臭的垃圾,心情非常复杂和无奈,很难用一个词来形容自己的感受。”受灾青少年S5: “以前只是了解过历史上灾难后的逃难,如今,经历了现实版逃难,我们借住到亲戚家,心里五味杂陈,一言难尽。”
2.2 主题2: 灾后1个月,经历这次洪涝灾害的青少年的PTSD
在灾后1个多月的访谈中,“恍如昨日”和“偶尔想起”仍是受灾青少年常见的心理影响,有明显的PTSD表现。
① 恍如昨日。受灾青少年S6访谈提起洪水时,脸上表现出悲伤表情,哭泣不止。S6: “感觉往日受灾情景历历在目,仿佛就在昨天。”S8: “漆黑的夜里,我和妈妈紧急撤离,撤离时间太紧急一件衣服也没带,淌着很深的水,我怕掉到水沟,太可怕了!现在我总是梦到我掉水里了。”
② 偶尔想起。受灾青少年S3访谈提起洪水时回忆到: “我现在偶尔还是会想起当时的情况,没水、没电的日子真是没法过呀。家里也没有菜,我们只能吃发的方便面和家里过去囤积的土豆,还好家里还有天燃气。接些雨水当冲厕水,也不能洗澡,没水、没电真不好受!”S10: “现在我一下雨就害怕再次被淹,害怕再次来到安置点,学习被中断。”
2.3 主题3: 经历这次洪涝灾害的青少年的创伤后成长方面
① 感恩国家强大。青少年S10: “看着一排排救援车辆到达灾区,不禁泪流满面,真是一方有难八方支援。非常感恩我们生活在一个祖国强大的时代。”S7: “救援车送来的水、方便面和奶堆积在安置点,在这么短的时间内,五湖四海的人送来这么多吃的,真是非常感动,感谢我们的国家。”S10: “我们在安置点居住,有很多志愿者为大家服务,有的免费给大家看病,有的组织大家的生活日常,还有一些教我们唱歌,非常感谢国家的救助。”
② 帮助他人。经历这次洪涝灾害对青少年的人生规划有些变化。S7: “想去当兵,报答国家,报答那些帮助过我们的人。”S1: “想当一名现场记者,为家乡做贡献,为家乡出力。” S12: “想做市长,帮助更多的人,做一个有理想、有抱负的人,向帮助我们的人学习,确保大家的健康平安。”S4: “为被洪水造成破坏的家园感到惋惜,被救援人员的行为所感动,长大了也要多帮助他人。”
③ 生命无常。S9: “过去我想当科学家,经历这次灾害变化,现在我想当医生,去帮助那些受灾群众,同时也觉得健康地和一家人在一起最重要,真是不知道未来会发生什么。”S5: “这次洪水真是太突然了,真是不知道我们会经历这样的事情,想想真是生命无常,也许雨水再大一些,我们都成为了鬼魂了,所以我以后要珍惜生命,好好活着。”
2.4 主题4: 正常生活节奏被打乱后,青少年的应对方式
① 学习。访谈中S6: “大雨后,我还是按照老师和父母的要求按时预习新课,在家学习。” S10: “大雨后,哪里都是水,小区外边的积水到腰了,家里也没电,就到手机上看看学习的相关内容,然后看新闻,好在有发电车,可以给手机充电。”
② 玩手机和电脑。S11和S2: “我们在安置点没有带课本,只能玩父母的手机和电脑,打打游戏,瞎逛逛,要不在安置点的日子太难熬了。”S8: “没有电,爸爸妈妈去单位加班了,也没有上辅导班,也不知道做些什么,只能打游戏,看看新闻,没有心情学习。”
③ 帮助大人做事。S5: “父母去抗洪了,我就负责照顾2岁的弟弟,照顾小朋友非常心累,感觉到父母养育我们真不容易。”S6: “家里没有电了,电梯停了,爷爷、奶奶上下步梯不方便,我就负责帮爷爷、奶奶买菜、买水、手机充电,偶尔也做做作业。”
④ 做志愿者。S9: “看到来自四面八方的救援车我非常感动,我就到各个安置点去当志愿者,搬运物资。”S7: “看大家都在抗洪,我也做些力所能及的小事情,帮助一下老人和小朋友。”
3. 讨论
经历洪涝灾害后青少年以负性心理体验为主,需要专业心理支持,但创伤后成长良好。本研究中大部分青少年均承受不同程度的恐惧和悲伤,可见灾后对青少年进行心理帮助十分必要。政府方面: 在加强物资救援的同时,可以积极调配本地心理健康服务资源,提供情绪疏导与心理支持,提供必要的危机干预筛查并做出必要转接,如转接热线或其他社会心理健康服务资源。社会层面: 要增加对自然灾害相关知识的科普宣传,同时也要重视心理咨询对促进心理健康的重大意义,确保青少年经历突发事件后的身心健康。在提供专业服务的同时,还应当严格保护受助者的个人隐私,重视避免助人者和受助者可能存在再次创伤。学校层面: 为了减少负性体验,可在重大灾害来临前,开展灾害教育课程和心理技能辅导,让该地区青少年人群了解重大灾害的详细信息,并具有与之相对应的心理技能或重大突发事件的心理危机干预能力,从而减少对重大灾害的负性心理体验。学校应注重提高对青少年情绪状态的识别能力,注意相关处理方法[12]。家庭方面: 需要关注青少年心理健康状况,及时发现青少年心理变化,给予相应的心理支持与帮助。
浦娟等[13]研究指出,经历一定负性事件后的青少年会有一定创伤后成长。本研究证实,大部分青少年经历洪水灾害后会更加珍惜生命,好好学习,报答帮助他们的人。本研究认为,学校及家庭应密切关注经历灾害后青少年的创伤后成长,引导其正确看待逆境的人生境遇,真正做到“把灾难当教材,与祖国共成长”; 政府应当加强青少年思想政治引领,通过发生的案例和社会上的鲜活素材,积极开展灾后思想政治引领和人生困境的逆商教育; 社会应给予青少年一个良好的成长环境,营造积极和谐的社会氛围,从而引领青少年健康成长。同时,社会、学校、家庭及政府应齐心协力,对创伤后成长不良的青少年进行适度的感恩或生命意义教育,最终引导青少年具有积极向上的人生价值观和生命意义感。
青少年自我控制能力需要加强,尤其是手机和网络成瘾急需关注。正常生活节奏被打乱后,大部分青少年应对良好,但本研究访谈到,有部分同学在父母抗洪期间,因父母没有时间管教,而且正值暑假,一直沉迷手机或网络游戏。研究[14]表明,网络成瘾已成为青少年不可忽视的行为问题并已受到研究者的普遍关注。青少年网络成瘾的影响因素错综复杂,在父母无精力监管的情况下,自我控制能力是非常重要的。自我控制是指个体为了实现长远目标,有意识地克服冲动、习惯或自动反应,调整自身行为的过程[15]。自我控制的能力是通往成功和幸福的关键,自我控制水平较高的个体有更高的自尊水平,更稳定的情绪状况和更好的学业成绩、健康状况和社会适应能力[16]。研究[17]表明,行为训练、体育锻炼、正念和情绪觉察均可提高青少年的自我控制水平。此外,在信息时代背景下,青少年自主学习的动机也需要加强,学习动机较强的学生通过学习不仅能收获知识,而且能满足求知欲、体验到较强的学习成就感和愉悦感[18]。本研究认为,家庭应加强对青少年的约束,进行适当家庭教育,言传身教,提高家长自我控制能力,从而影响孩子,预防手机成瘾; 政府应出台相关条例,对青少年手机成瘾进行界定,维护良好社会环境,预防手机成瘾; 社会应与政府共同维护良好网络环境,减少青少年网络成瘾的诱发因素; 学校层面应重视培养青少年的自我控制理念,倡导学生自律,帮助学生制订学习计划,逐渐提高自我控制能力。
中国关于自然灾害心理行为的研究处于初级阶段,对经历重大自然灾害受灾群众的心理影响研究尚少,尤其对于青少年人群。本研究通过质性研究分析了经历河南省新乡市2021年7—8月特大洪水的青少年的心理体验,建议社会及学校等相关机构对青少年人群给予支持和帮助,预防PTSD, 以期为探讨和建立重大洪涝自然灾害对青少年心理行为影响的预测指标提供依据,为健全中国心理服务机制提供证据。
-
表 1 不同预后急性脑梗死机械取栓患者的临床资料比较(x±s)[n(%)]M(P25, P75)
临床资料 预后良好组
(n=48)预后不良组
(n=57)年龄/岁 66.38±12.75 67.07±11.12 男 35(72.92) 33(57.89) 高血压病 34(70.83) 41(71.93) 糖尿病 16(33.33) 16(28.07) 房颤 18(37.50) 17(29.82) 冠心病 8(16.67) 10(17.54) 入院收缩压/mmHg 148.86±18.74 150.85±24.56 入院舒张压/mmHg 81.56±12.88 85.42±17.78 入院NIHSS/分 18.00(12.00, 27.25) 22.00(13.00, 35.00) 手术时间/min 85.50(70.00, 112.50) 100.00(80.00, 150.00)* 尿比重/(g/cm3) 1.04±0.01 1.03±0.01 空腹血糖/(mmol/L) 6.18(5.42, 7.44) 6.30(5.34, 7.83) 糖化血红蛋白/% 5.75(5.50, 5.90) 5.90(5.30, 6.40) 红细胞计数/(×109/L) 4.67±0.68 4.64±0.57 红细胞压积/% 42.36±5.41 41.97±4.81 血小板计数/(×109/L) 179.18±49.96 186.82±60.33 中性细胞百分比/% 70.00(60.40, 76.23) 81.60(75.20, 85.80)* 淋巴细胞百分比/% 21.45(17.53, 28.48) 11.50(9.00, 17.10)* NLR 3.30(2.15, 4.35) 7.13(4.40, 9.53)* NLR: 中性粒细胞与淋巴细胞比值。与预后良好组比较, *P < 0.05。 表 2 前循环梗死组与后循环梗死组相关临床资料比较(x±s)M(P25, P75)
临床资料 前循环梗死组
(n=74)后循环梗死组
(n=31)入院收缩压/mmHg 150.70±21.28 148.00±23.56 入院舒张压/mmHg 81.86±14.92 87.68±16.92 红细胞计数/(×109/L) 4.59±0.61 4.80±0.63 红细胞压积/% 41.54±5.03 43.62±4.99 血小板计数/(×109/L) 179.19±55.51 192.71±55.22 尿比重/(g/cm3) 1.04±0.01 1.03±0.02 手术时间/min 90.00(70.00, 110.00) 108.00(81.00, 160.00)* 入院NIHSS/分 18.00(12.75, 27.00) 30.00(10.00, 35.00)* 空腹血糖/(mmol/L) 6.20(5.39, 7.44) 6.30(5.30, 8.06) 糖化血红蛋白/% 5.80(5.40, 6.13) 5.90(5.50, 6.50) 中性粒细胞百分/% 74.00(62.23, 82.33) 80.60(69.10, 84.00) 淋巴细胞百分比/% 18.25(10.28, 27.68) 13.30(10.01, 21.20) NLR 4.03(2.22, 8.08) 6.17(3.26, 8.34) NLR: 中性粒细胞与淋巴细胞比值。与前循环梗死组比较, *P < 0.05。 表 3 颈内动脉闭塞组与大脑中动脉闭塞组相关临床资料比较(x±s)M(P25, P75)
临床资料 颈内动脉组
(n=34)大脑中动脉组
(n=37)入院收缩压/mmHg 155.26±25.40 145.24±15.60 入院舒张压/mmHg 80.56±15.21 83.68±14.97 红细胞计数/(×109/L) 4.58±0.69 4.61±0.57 红细胞压积/% 41.33±5.47 41.76±4.76 血小板计数/(×109/L) 177.82±56.01 182.32±55.99 尿比重/(g/cm3) 1.04±0.01 1.04±0.01 手术时间/min 97.50(78.75, 120.50) 85.00(60.00, 96.50) 入院NIHSS/分 18.00(12.00, 24.75) 18.00(12.50, 27.00) 空腹血糖/(mmol/L) 6.32(5.49, 8.19) 5.80(5.20, 6.97) 糖化血红蛋白/% 5.80(5.50, 6.10) 5.70(5.30, 6.25) 中性粒细胞百分/% 72.35(56.50, 82.18) 75.00(69.70, 83.75) 淋巴细胞百分比/% 20.45(10.53, 34.80) 18.20(10.05, 22.85) NLR 3.36(1.62, 8.06) 4.19(3.14, 8.41) NLR: 中性粒细胞与淋巴细胞比值。 表 4 影响急性脑梗死机械取栓患者预后的危险因素分析
变量 回归系数 标准误 Wald(χ2)值 P值 OR值 95%CI 手术时间 0.012 0.006 4.026 0.045 1.012 1.000~1.023 中性粒细胞百分比 0.127 0.102 1.542 0.214 1.135 0.929~1.386 淋巴细胞百分比 0.200 0.115 3.031 0.082 1.221 0.975~1.529 NLR 0.434 0.171 6.437 0.011 1.543 1.104~2.157 NLR: 中性粒细胞与淋巴细胞比值。 -
[1] SACKS D, BAXTER B, CAMPBELL B C V, et al. Multisociety consensus quality improvement revised consensus statement for endovascular therapy of acute ischemic stroke: from the American association of neurological surgeons (AANS), American society of neuroradiology (ASNR), cardiovascular and interventional radiology society of Europe (CIRSE), Canadian interventional radiology association (CIRA), congress of neurological surgeons (CNS), European society of minimally invasive neurological therapy (ESMINT), European society of neuroradiology (ESNR), European stroke organization (ESO), society for cardiovascular angiography and interventions (SCAI), society of interventional radiology (SIR), society of NeuroInterventional surgery (SNIS), and world stroke organization (WSO)[J]. J Vasc Interv Radiol, 2018, 29(4): 441-453. doi: 10.1016/j.jvir.2017.11.026
[2] POWERS W J, RABINSTEIN A A, ACKERSON T, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American heart association/American stroke association[J]. Stroke, 2018, 49(3): e46-e110.
[3] GIEDE-JEPPE A, MADŽAR D, SEMBILL J A, et al. Increased neutrophil-to-lymphocyte ratio is associated with unfavorable functional outcome in acute ischemic stroke[J]. Neurocrit Care, 2020, 33(1): 97-104. doi: 10.1007/s12028-019-00859-5
[4] SHI J, PENG H, YOU S, et al. Increase in neutrophils after recombinant tissue plasminogen activator thrombolysis predicts poor functional outcome of ischaemic stroke: a longitudinal study[J]. Eur J Neurol, 2018, 25(4): 687-696. doi: 10.1111/ene.13575
[5] BROOKS S D, SPEARS C, CUMMINGS C, et al. Admission neutrophil-lymphocyte ratio predicts 90 day outcome after endovascular stroke therapy[J]. J Neurointerv Surg, 2014, 6(8): 578-583. doi: 10.1136/neurintsurg-2013-010780
[6] KURAMATSU J B, BIFFI A, GERNER S T, et al. Association of surgical hematoma evacuation vs conservative treatment with functional outcome in patients with cerebellar intracerebral hemorrhage[J]. JAMA, 2019, 322(14): 1392-1403. doi: 10.1001/jama.2019.13014
[7] QUN S, TANG Y, SUN J, et al. Neutrophil-to-lymphocyte ratio predicts 3-month outcome of acute ischemic stroke[J]. Neurotox Res, 2017, 31(3): 444-452. doi: 10.1007/s12640-017-9707-z
[8] XUE J, HUANG W, CHEN X, et al. Neutrophil-to-lymphocyte ratio is a prognostic marker in acute ischemic stroke[J]. J Stroke Cerebrovasc Dis, 2017, 26(3): 650-657. doi: 10.1016/j.jstrokecerebrovasdis.2016.11.010
[9] HYUN S, KWON S, CHO S, et al. Can the neutrophil-to-lymphocyte ratio appropriately predict carotid artery Stenosis in patients with ischemic stroke-A retrospective study[J]. J Stroke Cerebrovasc Dis, 2015, 24(11): 2646-2651. doi: 10.1016/j.jstrokecerebrovasdis.2015.07.024
[10] SUN Y, YOU S, ZHONG C, et al. Neutrophil to lymphocyte ratio and the hematoma volume and stroke severity in acute intracerebral hemorrhage patients[J]. Am J Emerg Med, 2017, 35(3): 429-433. doi: 10.1016/j.ajem.2016.11.037
[11] GIEDE-JEPPE A, BOBINGER T, GERNER S T, et al. Neutrophil-to-lymphocyte ratio is an independent predictor for in-hospital mortality in spontaneous intracerebral hemorrhage[J]. Cerebrovasc Dis, 2017, 44(1/2): 26-34. http://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsRW5nTmV3UzIwMjEwMzAyEiBjZTA1OTE3OGM3N2NkZDhiN2YwNDI0ODI2MTJiYTZmNhoIZHVqajFicmc%3D
[12] LATTANZI S, CAGNETTI C, PROVINCIALI L, et al. Neutrophil-to-lymphocyte ratio and neurological deterioration following acute cerebral hemorrhage[J]. Oncotarget, 2017, 8(34): 57489-57494. doi: 10.18632/oncotarget.15423
[13] GONG P, XIE Y, JIANG T, et al. Neutrophil-lymphocyte ratio predicts post-thrombolysis early neurological deterioration in acute ischemic stroke patients[J]. Brain Behav, 2019, 9(10): e01426. http://www.researchgate.net/publication/330807063_Abstract_TP229_High_Neutrophil-to-Lymphocyte_Ratio_Predicts_Early_Neurological_Deterioration_in_Ischemic_Stroke_Patients
[14] LUX D, ALAKBARZADE V, BRIDGE L, et al. The association of neutrophil-lymphocyte ratio and lymphocyte-monocyte ratio with 3-month clinical outcome after mechanical thrombectomy following stroke[J]. J Neuroinflammation, 2020, 17(1): 60-68. doi: 10.1186/s12974-020-01739-y
[15] KIM J Y, PARK J, CHANG J Y, et al. Inflammation after ischemic stroke: the role of leukocytes and glial cells[J]. Exp Neurobiol, 2016, 25(5): 241-251. doi: 10.5607/en.2016.25.5.241
[16] DUAN Z, WANG H, WANG Z, et al. Neutrophil-lymphocyte ratio predicts functional and safety outcomes after endovascular treatment for acute ischemic stroke[J]. Cerebrovasc Dis, 2018, 45(5/6): 221-227. http://www.karger.com/Article/FullText/489401
[17] ROSELL A, CUADRADO E, ORTEGA-AZNAR A, et al. MMP-9-positive neutrophil infiltration is associated to blood-brain barrier breakdown and basal Lamina type Ⅳ collagen degradation during hemorrhagic transformation after human ischemic stroke[J]. Stroke, 2008, 39(4): 1121-1126. doi: 10.1161/STROKEAHA.107.500868
[18] GAUTIER S, OUK T, TAGZIRT M, et al. Impact of the neutrophil response to granulocyte colony-stimulating factor on the risk of hemorrhage when used in combination with tissue plasminogen activator during the acute phase of experimental stroke[J]. J Neuroinflammation, 2014, 11: 96. doi: 10.1186/1742-2094-11-96
[19] GUO Z, YU S, CHEN X, et al. Suppression of NLRP3 attenuates hemorrhagic transformation after delayed rtPA treatment in thromboembolic stroke rats: Involvement of neutrophil recruitment[J]. Brain Res Bull, 2018, 137: 229-240. doi: 10.1016/j.brainresbull.2017.12.009
[20] HERMANN D M, KLEINSCHNITZ C, GUNZER M. Implications of polymorphonuclear neutrophils for ischemic stroke and intracerebral hemorrhage: Predictive value, pathophysiological consequences and utility as therapeutic target[J]. J Neuroimmunol, 2018, 321: 138-143. doi: 10.1016/j.jneuroim.2018.04.015
[21] LIESZ A, HU X, KLEINSCHNITZ C, et al. Functional role of regulatory lymphocytes in stroke: facts and controversies[J]. Stroke, 2015, 46(5): 1422-1430. doi: 10.1161/STROKEAHA.114.008608
[22] LIESZ A, ZHOU W, NA S Y, et al. Boosting regulatory T cells limits neuroinflammation in permanent cortical stroke[J]. J Neurosci, 2013, 33(44): 17350-17362. doi: 10.1523/JNEUROSCI.4901-12.2013
[23] HASSAN A E, SHARIFF U, SAVER J L, et al. Impact of procedural time on clinical and angiographic outcomes in patients with acute ischemic stroke receiving endovascular treatment[J]. J Neurointerv Surg, 2019, 11(10): 984-988. doi: 10.1136/neurintsurg-2018-014576
[24] SPIOTTA A M, VARGAS J, TURNER R, et al. The golden hour of stroke intervention: effect of thrombectomy procedural time in acute ischemic stroke on outcome[J]. J Neurointerv Surg, 2014, 6(7): 511-516. doi: 10.1136/neurintsurg-2013-010726
-
期刊类型引用(16)
1. 苍姗,张帆,陶佳. 血清MMP-9、sTREM-1对输尿管结石患者术后泌尿系统感染的预测价值. 国际检验医学杂志. 2024(03): 257-260+265 .  百度学术
百度学术
2. 崔伟强,孙枫林,张小启. 血清CRP、ALT、CK-MB水平及APACHEⅡ评分评估有机磷中毒病情程度和预后的研究. 临床医学. 2024(02): 5-8 .  百度学术
百度学术
3. 王冠超,张永涛. APACHEⅡ评分结合血清PCT、hs-CRP对重症肺炎合并呼吸衰竭的预测价值研究. 现代医药卫生. 2024(08): 1307-1311+1316 .  百度学术
百度学术
4. 张育源,王晓聪,陈少芬. 经鼻高流量氧疗联合氨溴索治疗老年重症肺炎并呼吸衰竭的效果. 临床合理用药. 2024(18): 168-171 .  百度学术
百度学术
5. 田静,袁浩. 成年重症肺炎合并呼吸衰竭患者血清中sTREM-1、TLR4、VCAM-1的表达及对预后的评估价值. 中国医师杂志. 2024(05): 707-711 .  百度学术
百度学术
6. 丁阳琛,金洋,韦周兵. 罂粟碱联合生长抑素治疗重症急性胰腺炎的临床效果观察. 医学理论与实践. 2024(17): 2943-2945 .  百度学术
百度学术
7. 凌洁,陈娟红,张帅. 莫西沙星联合比阿培南治疗老年重症肺炎患者疗效及对炎性因子肿瘤坏死因子相关激活蛋白和血管细胞黏附分子-1的影响. 中国药物与临床. 2024(16): 1058-1062 .  百度学术
百度学术
8. 袁媛,丁晓彤,司艳,李冉冉,刘燕,吴金群,郑晓轩,苑茂静,王欣. 综合康复干预对重症肺炎患者病情控制、血气指标及肺功能的影响. 河北医药. 2024(23): 3630-3632+3636 .  百度学术
百度学术
9. 李甲,郑立慧,李霞. 血清sTREM-1、8-OHdG、HBP与肺炎严重程度的关系及其在重症肺炎患者中的预后价值. 转化医学杂志. 2024(06): 889-894 .  百度学术
百度学术
10. 李宁宁,翟展艺,李春苗,李海明. 血清降钙素原、磷评估老年慢性阻塞性肺疾病合并呼吸衰竭患者预后的价值. 福建医科大学学报. 2024(06): 402-406 .  百度学术
百度学术
11. 焦亚芳,陈庭萱,杜文艳. 气道分级管理模式下的护理对NCPAP肺透明膜病新生儿的影响. 国际医药卫生导报. 2023(03): 390-394 .  百度学术
百度学术
12. 刘锦茂,张小林,胡敏. 血清C反应蛋白、前白蛋白和红细胞体积分布宽度对重症肺炎合并呼吸衰竭患者预后的预测价值. 临床与病理杂志. 2023(01): 22-28 .  百度学术
百度学术
13. 赵茜. 老年吸入性肺炎患者预后的影响因素. 中国民康医学. 2023(18): 15-17 .  百度学术
百度学术
14. 黄正玲,张蕖,贾贤芬,崔陈陈,张彬. 针对性护理配合气道分级管理在早产儿呼吸窘迫综合征中的应用. 临床与病理杂志. 2023(09): 1670-1676 .  百度学术
百度学术
15. 林珍花,林冰冰. 风险防范模式下气道维护流程再造在ICU机械通气患者中的应用. 医疗装备. 2023(22): 133-135 .  百度学术
百度学术
16. 万盼盼,周闪闪. 重症创伤性SAH术后气管切开患者UEX的影响因素及护理干预策略. 疾病监测与控制. 2022(05): 405-408 .  百度学术
百度学术
其他类型引用(0)




 下载:
下载:
 苏公网安备 32100302010246号
苏公网安备 32100302010246号
