A Nomogram model establishment for noscomial infection in elderly patients with hypertension and diabetes mellitus
-
摘要:目的 分析老年高血压合并糖尿病患者发生医院感染(HAI)的危险因素,并建立预测HAI的Nomogram模型。方法 回顾性分析148例老年高血压合并糖尿病患者的临床资料,根据是否发生HAI将患者分为HAI组和非HAI组。通过单因素、多因素Logistic回归分析筛选出HAI发生的独立危险因素,同时应用Nomogram法对各个因素进行评分,构建预测模型。应用受试者工作特征(ROC)曲线评估模型的预测价值,并对模型进行内部验证,计算一致性指数(C-index),绘制校准图。结果 148例患者平均年龄为(64.21±12.84)岁,其中32例(21.62%)患者发生HAI。单因素分析显示,年龄、吸烟、共患病程、血压控制情况、血糖控制情况、合并其他基础疾病、急性生理学与慢性健康状况评分系统Ⅱ(APACHEⅡ)评分、意识障碍、白蛋白水平均是HAI发生的影响因素(P < 0.10)。多因素Logistic回归分析显示,共患病程≥10年(OR=3.589,95% CI为1.056~12.193,P=0.041),血糖控制不达标(OR=4.538,95% CI为1.287~16.002,P=0.019),合并其他基础疾病(OR=8.893,95% CI为2.624~30.132,P < 0.001),APACHEⅡ评分≥20分(OR=6.259,95% CI为1.934~20.256,P=0.002),存在意识障碍(OR=9.365,95% CI为2.744~34.477,P=0.001)均是HAI发生的独立危险因素。基于上述预测因子建立Nomogram预测模型,经验证,该模型贴合度、C-index、ROC曲线下面积均良好,提示该模型具有良好的预测效能和区分度。结论 共患病程≥10年、血糖控制不达标、合并其他基础疾病、APACHE Ⅱ评分≥20分、存在意识障碍均是老年高血压合并糖尿病患者发生HAI的独立危险因素,基于上述危险因素建立的Nomogram模型具有良好的预测效能,可为HAI防控工作提供参考依据。Abstract:Objective To investigate the risk factors of hospital-associated infection (HAI) in elderly patients with hypertension and diabetes mellitus, and to establish a nomogram model for HAI.Methods A retrospective study was performed to analyze the clinical data of 148 elderly patients with hypertension complicated with diabetes mellitus. The patients were divided into the HAI group and non-HAI group according to occurrence of HAI. Univariate analysis and multivariate Logistic regression analysis were used to screen out the independent risk factors of HAI occurrence. Then, each factor was scored by Nomogram method to construct the prediction model. Receiver operating characteristic (ROC) curve was drawn to assess the predictive value of the established Nomogram. Furthermore, the predictive ability of the Nomogram model was internally validated by calculating the C-index and the calibration plot was drawn.Results The mean age of 148 patients was (64.21±12.84) years, and 32 patients (21.62%) developed HAI. Univariate analysis showed that the occurrence of HAI was correlated with age, smoking, disease duration of comorbidities, blood pressure and blood glucose control state, other underlying diseases, APAHEⅡ scores, consciousness state and albumin levels (P < 0.05). The multivariate Logistic regression analysis showed that disease duration of comorbidities ≥10 years (OR=3.589, 95%CI, 1.056~12.193, P=0.041), blood glucose control substandard (OR=4.538, 95%CI, 1.287~16.002, P=0.019), other underlaying diseases (OR=8.893, 95%CI, 2.624~30.132, P < 0.001), APACHEⅡ score ≥20 (OR=6.259, 95%CI, 1.934~20.256, P=0.002), consciousness disorder (OR=9.365, 95%CI, 2.744~34.477, P=0.001) were independent risk factors for HAI occurrence. Based on above risk factors in Nomogram model, statistical analysis showed that this model had a good discrimination, C-index value and the area under the ROC curve, indicating that the nomogram model had better predictive performance and differentiation.Conclusion The disease duration of comorbidities ≥10 years, substandard blood glucose control, other underlying diseases, APACHEⅡscore ≥20, consciousness disorder are independent risk factors for HAI occurrence in in elderly patients with hypertension and diabetes mellitus. Nomogram model based on these risk factors has good predictive efficacy and important clinical value, and can provide reference for prevention and control of HAI.
-
Keywords:
- elderly patients /
- hypertension /
- diabetes mellitus /
- hospital-associated infection /
- risk factors /
- Nomogram model
-
医院感染(HAI)是指住院患者在医院内获得的感染, HAI的发生将显著影响原发病预后,导致更高的病死率、更长的住院时间和更高的医疗费用,是医院防控工作的重点和难点。老年住院患者因器官功能衰退,免疫、防御功能低下,且常处于多病共存、带病生存状态,是HAI的高危易感群体[1-2]。目前,高血压、糖尿病均是老年人群常见的基础疾病, LI X Y等[3]研究发现,高血压经常与糖尿病共同存在,超过50%的老年高血压患者同时患有糖尿病。高血压合并糖尿病患者若发生HAI, 将导致更高的致死率、致残率。本研究回顾性分析148例老年高血压合并糖尿病患者的临床资料,探讨HAI发生的相关危险因素,并建立简便可靠的Nomogram预测模型,旨在实现HAI早期预警,从而改善患者预后。
1. 资料与方法
1.1 一般资料
采用回顾性队列研究方法,选取2016年1月—2018年12月本院老年医学科收治的148例老年高血压合并糖尿病患者作为研究对象,其中男64例,女84例,年龄60~87岁,平均(64.21±12.84)岁。以国家卫生部颁布的《医院感染诊断标准(试行)》[4]为诊断参照,根据是否发生HAI将患者分为HAI组和非HAI组。本研究得到本院伦理委员会审核批准。纳入标准: ①年龄≥60岁者; ②符合《中国老年高血压管理指南2019》[5]和《中国2型糖尿病防治指南(2017年版)》[6]相关诊断标准者; ③入院前无全身感染或局部感染者; ④相关临床资料完整者。排除标准: ①入院时间不足72 h, 入院后死亡或转院者; ②合并严重心、肺、肝、肾功能不全者; ③患有精神类疾病者。
1.2 方法
收集患者年龄、性别、文化程度、是否吸烟(近1年平均每天吸烟≥1支为是)、是否饮酒(平均每日饮酒≥1次为是)、高血压病程、糖尿病病程,血压控制达标情况、血糖控制达标情况[5-7], 其他基础病(包括冠心病、心功能不全、心肌病、脑梗死、慢性阻塞性肺疾病、慢性肾病、肝病等)[8], 体质量指数(BMI)[9], 入院时急性生理学与慢性健康状况评分系统Ⅱ(APACHEⅡ)评分[10], 是否意识障碍及白蛋白水平[11]等资料。同时,记录HAI患者的感染发生部位和病原菌培养结果,检测仪器为VITEK2 Compact全自动微生物分析系统(法国生物梅里埃公司)。
1.3 判断标准
① 血压控制达标标准: 《中国老年高血压管理指南2019》[5]推荐, ≥65岁高血压合并2型糖尿病患者宜将血压控制在收缩压 < 140 mmHg且舒张压 < 90 mmHg, 若能耐受,可进一步降低为收缩压 < 130 mmHg且舒张压 < 80 mmHg, ≥80岁的患者首先降至收缩压 < 150 mmHg且舒张压 < 90 mmHg, 若耐受性良好,则进一步降至收缩压 < 140 mmHg且舒张压 < 90 mmHg。本研究将60~64岁患者收缩压 < 130 mmHg且舒张压 < 80 mmHg评定为血压控制达标,将65~79岁患者收缩压 < 140 mmHg且舒张压 < 90 mmHg评定为血压控制达标,将≥80岁患者收缩压 < 150 mmHg且舒张压 < 90 mmHg评定为血压控制达标。②血糖控制达标标准: 按照美国糖尿病学会(ADA)[7]和《中国2型糖尿病防治指南(2017年版)》[6]中的标准,以糖化血红蛋白(HbAlc)≤7.0%为血糖控制达标目标值。③ BMI分类: 依据世界卫生组织(WHO)对BMI的划分标准[9], 分为体质量过轻(BMI < 18.5 kg/m2)、正常(BMI 18.5~ < 25.0 kg/m2)、超重(BMI 25.0~ < 30.0 kg/m2)和肥胖(BMI≥30.0 kg/m2)。
1.4 统计学分析
采用SPSS 23.0统计学软件进行数据分析。计数资料以[n(%)]表示,比较采用χ2检验或Fisher确切概率法。将单因素分析中P < 0.10的变量纳入多因素Logistic回归分析,确定HAI发生的独立危险因素。基于多因素分析结果,应用R 3.4.0软件中的rms安装包建立Nomogram预测模型。绘制受试者工作特征(ROC)曲线,评估预测模型对HAI发生的预测价值。采用Bootstrap法进行内部验证,计算区分度评价指标一致性指数(C-index), 绘制校准图。以双侧P < 0.05为差异有统计学意义。
2. 结果
2.1 一般资料
148例老年高血压合并糖尿病患者中, 32例患者发生HAI(共36例次), HAI发病率为21.62%(32/148)。36例次HAI的感染部位分别为呼吸道16例次(44.44%)、泌尿生殖道10例次(27.78%)、血液系统5例次(13.89%)、中枢神经系统3例次(8.33%)、皮肤软组织2例次(5.56%)。
32例HAI患者共分离出40株病原菌,其中革兰阴性菌25株(肺炎克雷伯菌8株、铜绿假单胞菌6株、鲍氏不动杆菌5株、大肠埃希菌4株、其他2株)占62.50%, 革兰阳性菌13株(金黄色葡萄球菌5株、表皮葡萄球菌3株、粪肠球菌3株、其他2株)占32.50%, 真菌2株(白色念珠菌1株、光滑念珠菌1株)占5.00%。
2.2 老年高血压合并糖尿病患者发生HAI的单因素分析
单因素分析结果显示,年龄、吸烟、共患病程、血压控制情况、血糖控制情况、合并其他基础疾病、APACHE Ⅱ评分、意识障碍、白蛋白水平均是老年高血压合并糖尿病患者发生HAI的影响因素(P < 0.10), 见表 1。
表 1 老年高血压合并糖尿病患者发生HAI的单因素分析[n(%)]因素 HAI组(n=32) 非HAI组(n=116) χ2 P 年龄 ≥75岁 12(37.50) 25(21.55) 3.402 0.065 < 75岁 20(62.50) 91(78.45) 性别 男 14(43.75) 50(43.10) 0.004 0.948 女 18(56.25) 66(56.90) 文化程度 小学及以下 6(18.75) 21(18.10) 0.972 0.808 初中 16(50.00) 57(49.14) 中专或高中 7(21.88) 20(17.24) 大专及以上 3(9.38) 18(15.52) 吸烟 是 14(43.75) 24(20.69) 6.989 0.008 否 18(56.25) 92(79.31) 饮酒 是 9(28.13) 31(26.72) 0.025 0.874 否 23(71.88) 85(73.28) 高血压病程 ≥10年 17(53.12) 54(46.55) 0.434 0.510 < 10年 15(46.88) 62(53.45) 糖尿病病程 ≥10年 16(50.00) 48(41.38) 0.759 0.384 < 10年 16(50.00) 68(58.62) 共患病程 ≥10年 14(43.75) 19(16.38) 10.845 0.001 < 10年 18(56.25) 97(83.62) 血压控制情况 未达标 16(50.00) 32(27.59) 5.750 0.016 达标 16(50.00) 84(72.41) 血糖控制情况 未达标 15(46.88) 25(21.55) 8.155 0.004 达标 17(53.12) 91(78.45) 合并其他基础疾病 是 22(68.75) 25(21.55) 25.781 < 0.001 否 10(31.25) 91(78.45) BMI分类 低体质量 7(21.88) 20(17.24) 1.268 0.737 正常 17(53.12) 63(54.31) 超重 5(15.62) 26(22.41) 肥胖 3(9.38) 7(6.03) APACHE Ⅱ评分 ≥20分 20(62.50) 21(18.10) 24.683 < 0.001 < 20分 12(37.50) 95(81.90) 意识障碍 是 15(46.88) 16(13.79) 16.577 < 0.001 否 17(53.12) 100(86.21) 白蛋白水平 ≥30 g/L 18(56.25) 94(81.03) 8.370 0.004 < 30 g/L 14(43.75) 22(18.97) BMI: 体质量指数; APACHEⅡ: 急性生理学与慢性健康状况评分系统Ⅱ。 2.3 老年高血压合并糖尿病患者发生HAI的多因素Logistic回归分析
以是否发生HAI作为因变量(0=无HAI, 1=有HAI), 以单因素分析筛选出具有统计学意义的相关因素作为自变量,进行多因素Logistic回归分析,结果显示共患病程≥10年(OR=3.589, 95%CI为1.056~12.193, P=0.041), 血糖控制不达标(OR=4.538, 95%CI为1.287~16.002, P=0.019), 合并其他基础疾病(OR=8.893, 95%CI为2.624~30.132, P < 0.001), APACHEⅡ评分≥20分(OR=6.259, 95%CI为1.934~20.256, P=0.002), 存在意识障碍(OR=9.365, 95%CI为2.744~34.477, P=0.001)均是老年高血压合并糖尿病患者发生HAI的独立危险因素,见表 2。
表 2 老年高血压合并糖尿病患者发生HAI的多因素Logistic回归分析预测因子 β S. E. Wald 自由度 P OR 95%CI 年龄 -0.850 0.643 1.751 1.000 0.186 0.427 0.121~1.505 吸烟 0.746 0.632 1.390 1.000 0.238 2.108 0.610~7.280 共患病程 1.278 0.624 4.193 1.000 0.041 3.589 1.056~12.193 血压控制情况 1.159 0.608 3.628 1.000 0.057 3.186 0.967~10.494 血糖控制情况 1.513 0.643 5.534 1.000 0.019 4.538 1.287~16.002 合并其他基础疾病 2.185 0.623 12.318 1.000 < 0.001 8.893 2.624~30.132 APACHEⅡ评分 1.834 0.599 9.368 1.000 0.002 6.259 1.934~20.256 意识障碍 2.237 0.665 11.316 1.000 0.001 9.365 2.744~34.477 白蛋白水平 -0.123 0.654 0.036 1.000 0.850 0.884 0.245~3.186 常量 -4.506 0.953 22.369 1.000 < 0.001 0.011 — 2.4 老年高血压合并糖尿病患者发生HAI的Nomogram预测模型建立及评价
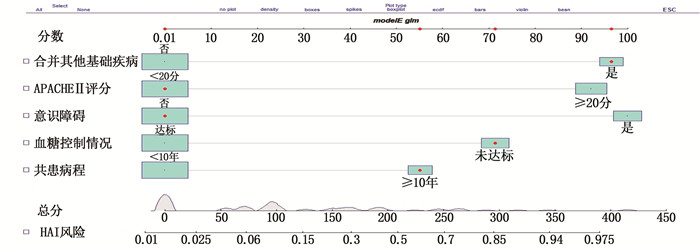
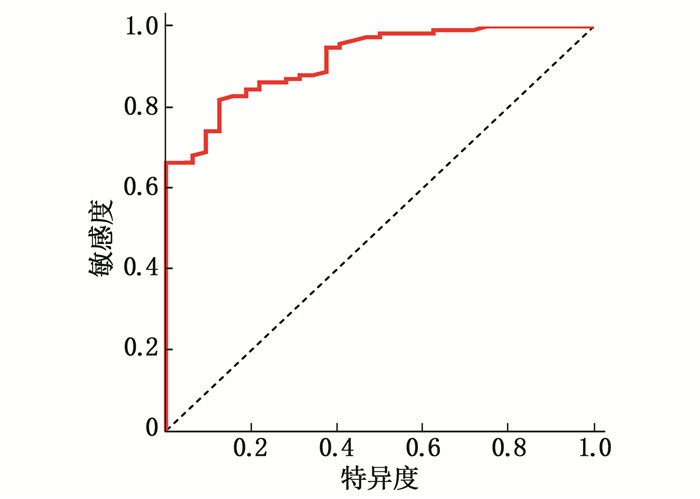
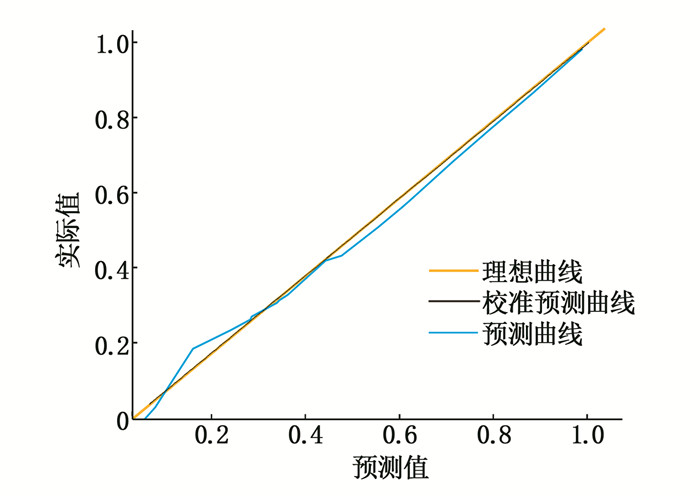
根据多因素logistic回归模型中的β系数,应用R软件Nomogram分析对各危险因素进行评分,构建个体化Nomogram预测模型,见图 1。在此模型中,意识障碍是HAI发生的最强预测因子(对应分值为100分),然后依次是合并其他基础疾病(97分)、APACHEⅡ评分≥20分(92分)、血糖控制未达标(71分)以及共患病程≥10年(55分),总分为415分。ROC曲线分析显示,该模型ROC曲线下面积(AUC)为0.918(95%CI为0.872~0.963, P < 0.001),提示该预测模型具有良好的预测能力,见图 2。对该Nomogram预测模型采用Bootstrap法进行内部验证,自抽样200次,其区分度评价指标C-index为0.746(95%CI为0.682~0.815, P < 0.001)。校准图显示,校准预测曲线与理想曲线贴合良好,说明该模型预测精确度及区分度均为良好,见图 3。
3. 讨论
血压异常、糖代谢紊乱严重威胁心脑血管系统的正常运转,并可导致器官功能性或器质性改变。老年高血压合并糖尿病患者常因不良并发症或靶器官损害需住院治疗,加之老年人自身免疫功能低下,抵抗力较弱,是HAI的高发人群。本研究进行回顾性队列分析发现,老年高血压合并糖尿病患者的HAI发生率高达21.62%, 远高于高血压患者、糖尿病患者和无病(无高血压与糖尿病)患者[2, 12]。因此,临床需加强对该类HAI高危患者的关注,以便及早采取防控措施,减少HAI的发生,进而改善患者预后。
本研究32例HAI患者中,呼吸道感染最多, 32例患者共分离出病原菌40株,主要致病菌为革兰阴性菌(占62.50%), 与相关研究[13-14]结果相似。医务人员可依据病原菌情况适时施以经验性治疗,为临床经验性用药提供一定指导和参考。本研究单因素及多因素Logistic回归分析结果显示,共患病程≥10年、血糖不达标、合并其他基础疾病、APACHE Ⅱ评分≥20分、存在意识障碍均是老年高血压合并糖尿病患者发生HAI的独立危险因素。高血压合并糖尿病患者的两病共患时间越长,对心血管及其他靶器官损害的协同效应越强[15], 故而发生HAI的概率较大。病程中,患者血糖水平与HAI感染率呈正相关,这可能是因为机体高血糖环境利于病原菌生长,且高血糖状态会导致肺部微血管病变和代谢酶结构与功能破坏,引起肺微循环障碍,增高患者感染概率[16-17]。对于同时合并其他基础疾病的患者而言,其免疫能力更差,且可能伴有日常生活能力不足或需长期氧疗、透析等情况而更多地暴露在医院风险环境内,病原菌感染可能性则更大[8, 18]。此外,入院时APACHEⅡ评分高和存在意识障碍也是老年患者发生HAI的重要因素。APACHEⅡ评分高和存在意识障碍均提示患者病情严重,有更高的误吸、痰液蓄积及菌群失衡风险,从而更加容易发生HAI[10, 19]。
为了建立量化的HAI风险预测模型,对患者感染风险进行评估,识别HAI高危人群,尽早干预,推动感控措施前移,本研究基于HAI的独立危险因素建立了HAI发生的Nomogram预测模型。Nomogram图是回归方程的一种可视化表现形式,可提供更加直观、个体化的患者发病风险概率[20-22]。经统计学验证,该模型贴合度、C-index、ROC曲线下面积均良好,提示模型具有可靠的预测效能和一致性,可应用于临床诊疗活动中。本研究中, 1例老年高血压合并糖尿病患者既往高血压病与糖尿病共患病程12年余,平素血糖控制未达标,且合并慢性肾功能不全,本次入院时意识尚清, APACHEⅡ评分14分,经Nomogram模型评分,该患者总评分为223分(55+71+97+0+0=223分),对应的风险预测值为0.57, 即该患者有57.00%的概率并发HAI。
本研究尚存不足之处: ①本研究为单中心回顾性病例研究,样本量偏小,且模型仅在内部人群中进行交叉验证; ② HAI涉及多个环节,影响因素众多,本研究纳入的指标仅为HAI管理的日常监测指标,未纳入更多的影响因素来构建预测模型; ③本研究应用的是Nomogram模型,而目前用于疾病预测的模型还有很多,包括时间序列模型(ARIMA模型)[23]、人工神经网络模型[24]以及不同方法相组合的模型(ARIMA-NARNN模型、AR1MAGRNN模型)[25]等。因此,本课题组未来还将扩大样本量开展多中心研究,对模型进一步修正和完善,以期构建更加准确、适用范围更广的预警模型。
综上所述,老年高血压合并糖尿病患者发生HAI的危险因素较多,主要包括共患病程≥10年、血糖不达标、合并其他基础疾病、APACHE Ⅱ评分≥20分、存在意识障碍等。基于上述危险因素建立的Nomogram模型能够有效预测HAI的发生概率,可为HAI防控工作提供参考依据。
-
表 1 老年高血压合并糖尿病患者发生HAI的单因素分析[n(%)]
因素 HAI组(n=32) 非HAI组(n=116) χ2 P 年龄 ≥75岁 12(37.50) 25(21.55) 3.402 0.065 < 75岁 20(62.50) 91(78.45) 性别 男 14(43.75) 50(43.10) 0.004 0.948 女 18(56.25) 66(56.90) 文化程度 小学及以下 6(18.75) 21(18.10) 0.972 0.808 初中 16(50.00) 57(49.14) 中专或高中 7(21.88) 20(17.24) 大专及以上 3(9.38) 18(15.52) 吸烟 是 14(43.75) 24(20.69) 6.989 0.008 否 18(56.25) 92(79.31) 饮酒 是 9(28.13) 31(26.72) 0.025 0.874 否 23(71.88) 85(73.28) 高血压病程 ≥10年 17(53.12) 54(46.55) 0.434 0.510 < 10年 15(46.88) 62(53.45) 糖尿病病程 ≥10年 16(50.00) 48(41.38) 0.759 0.384 < 10年 16(50.00) 68(58.62) 共患病程 ≥10年 14(43.75) 19(16.38) 10.845 0.001 < 10年 18(56.25) 97(83.62) 血压控制情况 未达标 16(50.00) 32(27.59) 5.750 0.016 达标 16(50.00) 84(72.41) 血糖控制情况 未达标 15(46.88) 25(21.55) 8.155 0.004 达标 17(53.12) 91(78.45) 合并其他基础疾病 是 22(68.75) 25(21.55) 25.781 < 0.001 否 10(31.25) 91(78.45) BMI分类 低体质量 7(21.88) 20(17.24) 1.268 0.737 正常 17(53.12) 63(54.31) 超重 5(15.62) 26(22.41) 肥胖 3(9.38) 7(6.03) APACHE Ⅱ评分 ≥20分 20(62.50) 21(18.10) 24.683 < 0.001 < 20分 12(37.50) 95(81.90) 意识障碍 是 15(46.88) 16(13.79) 16.577 < 0.001 否 17(53.12) 100(86.21) 白蛋白水平 ≥30 g/L 18(56.25) 94(81.03) 8.370 0.004 < 30 g/L 14(43.75) 22(18.97) BMI: 体质量指数; APACHEⅡ: 急性生理学与慢性健康状况评分系统Ⅱ。 表 2 老年高血压合并糖尿病患者发生HAI的多因素Logistic回归分析
预测因子 β S. E. Wald 自由度 P OR 95%CI 年龄 -0.850 0.643 1.751 1.000 0.186 0.427 0.121~1.505 吸烟 0.746 0.632 1.390 1.000 0.238 2.108 0.610~7.280 共患病程 1.278 0.624 4.193 1.000 0.041 3.589 1.056~12.193 血压控制情况 1.159 0.608 3.628 1.000 0.057 3.186 0.967~10.494 血糖控制情况 1.513 0.643 5.534 1.000 0.019 4.538 1.287~16.002 合并其他基础疾病 2.185 0.623 12.318 1.000 < 0.001 8.893 2.624~30.132 APACHEⅡ评分 1.834 0.599 9.368 1.000 0.002 6.259 1.934~20.256 意识障碍 2.237 0.665 11.316 1.000 0.001 9.365 2.744~34.477 白蛋白水平 -0.123 0.654 0.036 1.000 0.850 0.884 0.245~3.186 常量 -4.506 0.953 22.369 1.000 < 0.001 0.011 — -
[1] LLOPIS F, FERRÉC, GARCÍA-LAMBERECHTS E J, et al. Are short-stay units an appropriate resource for hospitalising elderly patients with infection[J]. Rev Calid Asist, 2016, 31(6): 322-328. doi: 10.1016/j.cali.2016.02.007
[2] 王力红, 赵霞, 郝晋, 等. 高龄老年患者医院感染特点[J]. 中国感染控制杂志, 2017, 16(1): 6-9. doi: 10.3969/j.issn.1671-9638.2017.01.002 [3] LI X Y, QI X, YUAN G H, et al. Microbiological profile and clinical characteristics of diabetic foot infection in Northern China: a retrospective multicentre survey in the Beijing area[J]. J Med Microbiol, 2018, 67(2): 160-168. doi: 10.1099/jmm.0.000658
[4] 中华人民共和国卫生部. 医院感染诊断标准(试行)[J]. 中华医学杂志, 2001, 81(5): 314-320. doi: 10.3760/j:issn:0376-2491.2001.05.027 [5] 中国老年医学学会高血压分会, 国家老年疾病临床医学研究中心中国老年心血管病防治联盟. 中国老年高血压管理指南2019[J]. 中国心血管杂志, 2019, 24(1): 1-23. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLQG201902001.htm [6] 中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2017年版)[J]. 中国实用内科杂志, 2018, 38(4): 292-344. https://www.cnki.com.cn/Article/CJFDTOTAL-SYNK201804009.htm [7] NATHAN D M, BUSE J B, DAVIDSON M B, et al. Management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes[J]. Diabetes Care, 2006, 29(8): 1963-1972. doi: 10.2337/dc06-9912
[8] 潘桂群, 章建龙, 龚少波, 等. 老年高血压合并糖尿病患者医院感染的临床特点及影响因素分析[J]. 中华医院感染学杂志, 2019, 29(7): 1035-1037, 1041. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY201907019.htm [9] MA Y, AJNAKINA O, STEPTOE A, et al. Higher risk of dementia in English older individuals who are overweight or obese[J]. Int J Epidemiol, 2020, 49(4): 1353-1365. doi: 10.1093/ije/dyaa099
[10] 粟毅. RICU医院获得性鲍曼不动杆菌肺炎49例临床分析[J]. 重庆医科大学学报, 2009, 34(11): 1584-1587. https://www.cnki.com.cn/Article/CJFDTOTAL-ZQYK200911037.htm [11] 刘海燕, 刘勃, 王捷, 等. 肾脏内科住院患者医院感染的危险因素分析[J]. 中华医院感染学杂志, 2017, 27(9): 1994-1996, 2004. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY201709020.htm [12] 吴晓霞, 左阿芳, 吴建义, 等. 老年糖尿病患者医院感染的临床特点及影响因素分析[J]. 中华医院感染学杂志, 2017, 27(22): 5122-5125. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY201722023.htm [13] 刘卫平, 海云婷, 郭天慧, 等. 老年患者医院感染现状调查及病原菌耐药分析[J]. 中华医院感染学杂志, 2018, 28(11): 1645-1649. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY201811011.htm [14] SCHERBAUM M, KÖSTERS K, MÜRBETH R E, et al. Incidence, pathogens and resistance patterns of nosocomial infections at a rural hospital in Gabon[J]. BMC Infect Dis, 2014, 14: 124. doi: 10.1186/1471-2334-14-124
[15] KIM K, LEE S H, LEE S W, et al. Current findings of kidney biopsy including nephropathy associated with hypertension and diabetes mellitus in Korea[J]. Korean J Intern Med, 2020, 35(5): 1173-1187. doi: 10.3904/kjim.2020.195
[16] 王雁, 阿迪力·阿不都热合曼, 王烁, 等. 精准血糖控制对脑卒中相关感染免疫功能的影响[J]. 中华急诊医学杂志, 2017, 26(4): 381-385. doi: 10.3760/cma.j.issn.1671-0282.2017.04.005 [17] 陈亮, 韩秀迪, 朱晓莉, 等. 社区获得性肺炎患者入院血糖水平与预后的相关性: 一项多中心、回顾性研究[J]. 解放军医学杂志, 2020, 45(1): 84-91. https://www.cnki.com.cn/Article/CJFDTOTAL-JFJY202001011.htm [18] 肖素红. 重症监护病房医院感染与年龄和基础疾病关系的临床研究[J]. 中国煤炭工业医学杂志, 2013, 16(8): 1334-1335. https://www.cnki.com.cn/Article/CJFDTOTAL-ZMGY201308048.htm [19] Öncül O, Öksüz S, Acar A, et al. Nosocomial infection characteristics in a burn intensive care unit: analysis of an eleven-year active surveillance[J]. Burns, 2014, 40(5): 835-841. doi: 10.1016/j.burns.2013.11.003
[20] 张鹏, 李育平, 王晓东, 等. 结合炎症反应指数的Nomogram模型对aSAH患者预后预测的价值[J]. 临床神经外科杂志, 2020, 17(2): 216-220. https://www.cnki.com.cn/Article/CJFDTOTAL-LCSW202002022.htm [21] IASONOS A, SCHRAG D, RAJ G V, et al. How to build and interpret a nomogram for cancer prognosis[J]. J Clin Oncol, 2008, 26(8): 1364-1370. http://europepmc.org/abstract/MED/18323559
[22] ZHANG P, LI Y, ZHANG J, et al. Risk factors analysis and a nomogram model establishment for late postoperative seizures in patients with meningioma[J]. J Clin Neurosci, 2020, 80: 310-317. http://www.sciencedirect.com/science/article/pii/S0967586820313138
[23] 刘峰, 朱妮, 邱琳, 等. ARIMA乘积季节模型在陕西省手足口病预测中的应用[J]. 中华流行病学杂志, 2016, 37(8): 1117-1120. http://qikan.cqvip.com/Qikan/Article/Detail?id=669725809 [24] TANG J, YANG B, ADAMS M P, et al. Artificial neural network-based prediction of outcome in Parkinson's disease patients using DaTscan SPECT imaging features[J]. Mol Imaging Biol, 2019, 21(6): 1165-1173. doi: 10.1007/s11307-019-01334-5
[25] WEI W, JIANG J, LIANG H, et al. Application of a combined model with Autoregressive Integrated Moving Average (ARIMA) and Generalized Regression Neural Network (GRNN) in forecasting hepatitis incidence in Heng County, China[J]. PLoS One, 2016, 11(6): eO156768.
-
期刊类型引用(4)
1. 陈婷婷,许东平,孙晋华,曾志伟,黄景泰,陈亮,李天林,黄馨莹,李远鹏,刘俊安,苏阿丽. 老年糖尿病者并发高血压对医院感染的影响分析. 心血管病防治知识. 2023(01): 16-18+22 .  百度学术
百度学术
2. 解彦格,魏宁,刘红艳. 急诊重症患者医院感染相关因素研究进展. 临床误诊误治. 2023(04): 149-152 .  百度学术
百度学术
3. 曹起云. 负压引流配合碘伏持续冲洗用于糖尿病足感染创面治疗中的效果. 糖尿病新世界. 2022(02): 183-186 .  百度学术
百度学术
4. 陈金妙,朱灵颖,廖米荣,卢柯妤. 糖尿病慢性伤口感染患者的临床特点及伤口愈合的危险因素分析. 中国现代医生. 2022(27): 50-54 .  百度学术
百度学术
其他类型引用(3)




 下载:
下载:
 苏公网安备 32100302010246号
苏公网安备 32100302010246号
