Relationships between ketogenic diet and metabolism-related fatty liver disease
-
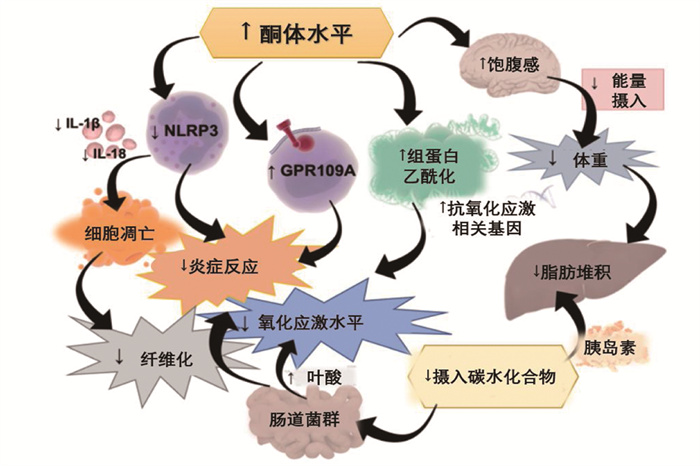
摘要: 代谢相关脂肪性肝病(MAFLD)是患病率高、危害较大的肝脏疾病,与代谢综合征、肥胖、糖尿病密切相关。生酮饮食是一种高脂肪、低碳水化合物与适量蛋白质的治疗性饮食方式,可有效降低体质量,改善胰岛素抵抗水平。生酮饮食中脂肪占比较高,与MAFLD的关系目前尚不明确。本研究对生酮饮食预防和治疗代谢相关脂肪性肝病的机制如改善胰岛素水平、降低体质量、改变肝线粒体代谢、改变肠道微生物组成、与有氧运动的协同作用等进行综述。Abstract: Metabolic-associated fatty liver disease (MAFLD) is a liver disease with high prevalence and great harm, which is closely related to metabolic syndrome, obesity and diabetes. Ketogenic diet is a therapeutic diet with high fat, low carbohydrate and appropriate protein, which can effectively reduce body mass and improve the level of insulin resistance. The proportion of fat in ketogenic diet is relatively high, and the relationship between ketogenic diet and MAFLD is not clear. This study aims to review the mechanism of ketogenic diet in the prevention and treatment of metabolic related fatty liver disease, such as improving insulin level, reducing body mass, changing liver mitochondrial metabolism, changing intestinal microbial composition and playing a synergetic effect with aerobic exercise.
-
-
表 1 生酮饮食分类及其具体要求
分类 每日能量 每日碳水 每日脂肪 附加 生酮饮食 ≈基础代谢量 < 50 g 有一定限制 无特殊 高脂生酮饮食 通常不受限制 < 50 g 无限制 无特殊 低热量生酮饮食 < 800 kal < 50 g 低 无特殊 中链甘油三酯生酮饮食 ≈基础代谢量 < 50 g 有一定限制 中短链不饱和脂肪酸为主 长链甘油三酯生酮饮食 ≈基础代谢量 < 50 g 有一定限制 长链不饱和脂肪酸为主 低碳水饮食 ≈基础代谢量 50~130 g 低 不属于严格意义上的生酮饮食 -
[1] ESLAM M, SANYAL A J, GEORGE J, et al. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease[J]. Gastroenterology, 2020, 158(7): 1999-2014. doi: 10.1053/j.gastro.2019.11.312
[2] ESLAM M, NEWSOME P N, SARIN, S K, et al. A new definition for metabolic associated fatty liver disease: an international expert consensus statement[J]. Hepatol, 2020, 73(1): 202-209. doi: 10.1016/j.jhep.2020.03.039
[3] YOUNOSSI Z, ANSTEE Q M, MARIETTI M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention[J]. Nat Rev Gastroenterol Hepatol, 2018, 15(1): 11-20. doi: 10.1038/nrgastro.2017.109
[4] RAHMAN K, DESAI C, IYER S S, et al. Loss of junctional adhesion molecule A promotes severe steatohepatitis in mice on a diet high in saturated fat, fructose, and cholesterol[J]. Gastroenterology, 2016, 151(4): 733-746. doi: 10.1053/j.gastro.2016.06.022
[5] BRUNT E M, WONG V W, NOBILI V, et al. Nonalcoholic fatty liver disease[J]. Nat Rev Dis Primers, 2015, 1: 15080. doi: 10.1038/nrdp.2015.80
[6] FAN J G, CAO H X. Role of diet and nutritional management in non-alcoholic fatty liver disease[J]. J Gastroenterol Hepatol, 2013, 28(Suppl 4): 81-87. http://www.vivamb.com/wp-content/uploads/2013/12/role-of-nutrition-on-fattyliverdieseaseonlinelibrary.wiley_.com_store_10.1111_jgh.12244_asset_jgh12244.pdf
[7] SALES R C, MEDEIROS P C, SPREAFICO F, et al. Olive oil, palm oil, and hybrid palm oil distinctly modulate liver transcriptome and induce NAFLD in mice fed a high-fat diet[J]. Int J Mol Sci, 2018, 20(1): 8. doi: 10.3390/ijms20010008
[8] DHAMIJA R, ECKERT S, WIRRELL E. Ketogenic diet[J]. Can J Neurol Sci, 2013, 40(2): 158-167. doi: 10.1017/S0317167100013676
[9] 江波, 邹大进, 马向华, 等. 生酮饮食干预2型糖尿病中国专家共识(2019年版)[J]. 实用临床医药杂志, 2019, 23(3): 1-6. doi: 10.7619/jcmp.201903001 [10] 江波, 白文佩, 郁琦, 等. 生酮饮食干预多囊卵巢综合征中国专家共识(2018年版)[J]. 实用临床医药杂志, 2019, 23(1): 1-4. doi: 10.7619/jcmp.201901001 [11] VAN BERKEL A A, IJFF D M, VERKUYL J M. Cognitive benefits of the ketogenic diet in patients with epilepsy: a systematic overview[J]. Epilepsy Behav, 2018, 87: 69-77. doi: 10.1016/j.yebeh.2018.06.004
[12] WHELESS J W. History of the ketogenic diet[J]. Epilepsia, 2008, 49(8): 3-5. http://anabolics24.com/art-The-History-Of-The-Ketogenic-Diet.html
[13] HIRONORI K, GUANLIANG C, YINHUA N, et al. Nonalcoholic fatty liver disease and insulin resistance: new insights and potential new treatments[J]. Nutrients, 2017, 9(4): 387. doi: 10.3390/nu9040387
[14] FRIEDMAN S L, NEUSCHWANDER-TETRI B A, RINELLA M, et al. Mechanisms of NAFLD development and therapeutic strategies[J]. Nat Med, 2018, 24(7): 908-922. doi: 10.1038/s41591-018-0104-9
[15] COBBINA E, AKHLAGHI F. Non-alcoholic fatty liver disease (NAFLD)-pathogenesis, classification, and effect on drug metabolizing enzymes and transporters[J]. Drug Metab Rev, 2017, 49(2): 197-211. doi: 10.1080/03602532.2017.1293683
[16] MARTINEZ K E, TUCKER L A, BAILEY B W, et al. Expanded normal weight obesity and insulin resistance in US adults of the national health and nutrition examination survey[J]. J Diabetes Res, 2017, 2017: 9502643.
[17] WATT M J, MIOTTO P M, DE NARDO W, et al. The liver as an endocrine organ-linking NAFLD and insulin resistance[J]. Endocr Rev, 2019, 40(5): 1367-1393. http://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsRW5nTmV3UzIwMjEwMzAyEiA0MDg0ZmViM2FiMmQ1MTljN2I4NjRkMzI4YmRmZTYwZhoId2xpY2t0OGY%3D
[18] ROMERO-GÓMEZ M, ZELBER-SAGI S, TRENELL M. Treatment of NAFLD with diet, physical activity and exercise[J]. J Hepatol, 2017, 67(4): 829-846. doi: 10.1016/j.jhep.2017.05.016
[19] SUMITHRAN P, PRENDERGAST L A, DELBRIDGE E, et al. Ketosis and appetite-mediating nutrients and hormones after weight loss[J]. Eur J Clin Nutr, 2013, 67(7): 759-764. doi: 10.1038/ejcn.2013.90
[20] BODEN G, SARGRAD K, HOMKO C, et al. Effect of a low-carbohydrate diet on appetite, blood glucose levels, and insulin resistance in obese patients with type 2 diabetes[J]. Ann Intern Med, 2005, 142(6): 403-411. doi: 10.7326/0003-4819-142-6-200503150-00006
[21] FREEDLAND S J, MAVROPOULOS J, WANG A, et al. Carbohydrate restriction, prostate cancer growth, and the insulin-like growth factor axis[J]. Prostate, 2008, 68(1): 11-19. doi: 10.1002/pros.20683
[22] MYETTE-CÔTÉ É, DURRER C, NEUDORF H, et al. The effect of a short-term low-carbohydrate, high-fat diet with or without postmeal walks on glycemic control and inflammation in type 2 diabetes: a randomized trial[J]. Am J Physiol Regul Integr Comp Physiol, 2018, 315(6): R1210-R1219. doi: 10.1152/ajpregu.00240.2018
[23] GODAY A, BELLIDO D, SAJOUX I, et al. Short-term safety, tolerability and efficacy of a very low-calorie-ketogenic diet interventional weight loss program versus hypocaloric diet in patients with type 2 diabetes mellitus[J]. Nutr Diabetes, 2016, 6(9): e230. doi: 10.1038/nutd.2016.36
[24] SASLOW L R, MASON A E, KIM S, et al. An online intervention comparing a very low-carbohydrate ketogenic diet and lifestyle recommendations versus a plate method diet in overweight individuals with type 2 diabetes: a randomized controlled trial[J]. J Med Internet Res, 2017, 19(2): e36. doi: 10.2196/jmir.5806
[25] PARTSALAKI I, KARVELA A, SPILIOTIS B E. Metabolic impact of a ketogenic diet compared to a hypocaloric diet in obese children and adolescents[J]. J Pediatr Endocrinol Metab, 2012, 25(7/8): 697-704. http://www.degruyter.com/dg/viewarticle.fullcontentlink:pdfeventlink/$002fj$002fjpem.2012.25.issue-7-8$002fjpem-2012-0131$002fjpem-2012-0131.pdf?format=INT&t:ac=j$002fjpem.2012.25.issue-7-8$002fjpem-2012-0131$002fjpem-2012-0131.xml
[26] SASLOW L R, DAUBENMIER J J, MOSKOWITZ J T, et al. Twelve-month outcomes of a randomized trial of a moderate-carbohydrate versus very low-carbohydrate diet in overweight adults with type 2 diabetes mellitus or prediabetes[J]. Nutr Diabetes, 2017, 7(12): 304. doi: 10.1038/s41387-017-0006-9
[27] 中华医学会妇产科学分会内分泌学组及指南专家组. 多囊卵巢综合征中国诊疗指南[J]. 中华妇产科杂志, 2018, 53(1): 2-6. https://www.cnki.com.cn/Article/CJFDTOTAL-SFCZ201810010.htm [28] MAVROPOULOS J C, YANCY W S, HEPBURN J, et al. The effects of a low-carbohydrate, ketogenic diet on the polycystic ovary syndrome: a pilot study[J]. Nutr Metab: Lond, 2005, 2: 35. doi: 10.1186/1743-7075-2-35
[29] PHY J L, POHLMEIER A M, COOPER J A, et al. Low starch/low dairy diet results in successful treatment of obesity and co-morbidities linked to polycystic ovary syndrome (PCOS)[J]. J Obes Weight Loss Ther, 2015, 5(2): 259. http://www.scienceopen.com/document_file/bbe09a9e-c53d-4dcf-ac89-ca33309a265a/PubMedCentral/bbe09a9e-c53d-4dcf-ac89-ca33309a265a.pdf
[30] TENDLER D, LIN S, YANCY W S, et al. The effect of a low-carbohydrate, ketogenic diet on nonalcoholic fatty liver disease: a pilot study[J]. Dig Dis Sci, 2007, 52(2): 589-593. doi: 10.1007/s10620-006-9433-5
[31] PÉREZ-GUISADO J, MUÑOZ-SERRANO A. The effect of the Spanish Ketogenic Mediterranean Diet on nonalcoholic fatty liver disease: a pilot study[J]. J Med Food, 2011, 14(7/8): 677-680. http://publicationslist.org/data/pv1peguj/ref-29/SKMD%20and%20NFLD.pdf
[32] LI J, BAI W P, JIANG B, et al. Ketogenic diet in women with polycystic ovary syndrome and liver dysfunction who are obese: a randomized, open-label, parallel-group, controlled pilot trial[J]. J Obstet Gynaecol Res, 2021, 47(3): 1145-1152. doi: 10.1111/jog.14650
[33] WATANABE M, TOZZI R, RISI R, et al. Beneficial effects of the ketogenic diet on nonalcoholic fatty liver disease: A comprehensive review of the literature[J]. Obesity Reviews, 2020, 21(8): e13024. doi: 10.1111/obr.13024
[34] LUUKKONEN P K, DUFOUR S, LYU K, et al. Effect of a ketogenic diet on hepatic steatosis and hepatic mitochondrial metabolism in nonalcoholic fatty liver disease[J]. PNAS, 2020, 117(13): 7347-7354. doi: 10.1073/pnas.1922344117
[35] MINISTRINI S, CALZINI L, MIGLIOLA E N, et al. Lysosomal acid lipase as a molecular target of the very low carbohydrate ketogenic diet in morbidly obese patients: the potential effects on liver steatosis and cardiovascular risk factors[J]. Journal of Clinical Medicine, 2019, 8(5): 621. doi: 10.3390/jcm8050621
[36] MARDINOGLU A, WU H, BJORNSON E, et al. An integrated understanding of the rapid metabolic benefits of a carbohydrate-restricted diet on hepatic steatosis in humans[J]. Cell Metab, 2018, 27(3): 559-571.
[37] ANEKWE CV, CHANDRASEKARAN P, STANFORD F C. Ketogenic diet-induced elevated cholesterol, elevated liver enzymes and potential non-alcoholic fatty liver disease[J]. Cureus, 2020, 12(1): e6605. http://www.researchgate.net/publication/338484953_Ketogenic_Diet-induced_Elevated_Cholesterol_Elevated_Liver_Enzymes_and_Potential_Non-alcoholic_Fatty_Liver_Disease/download
[38] ZHANG Q, XU L, XIA J, et al. Treatment of diabetic mice with a combination of ketogenic diet and aerobic exercise via modulations of PPARs gene programs[J]. PPAR Res, 2018, 2018: 4827643. http://www.onacademic.com/detail/journal_1000040474765510_a3ec.html
-
期刊类型引用(7)
1. 张考珍,严燕艺,商明,关换琼,张爱珍. 高龄孕妇再生育出生缺陷情况及其影响因素分析. 中外医学研究. 2022(10): 139-142 .  百度学术
百度学术
2. 孟远霞. 责任亲情交互护理模式干预在新生儿出生缺陷产妇中的应用效果及对产妇产后生活质量的影响. 临床医学研究与实践. 2021(04): 174-176+182 .  百度学术
百度学术
3. 罗丽兰,吴岸晓,王丽婷. 胎儿先天性畸形的调查结果统计及危险因素分析. 中国优生与遗传杂志. 2021(01): 107-110 .  百度学术
百度学术
4. 李淑妮,许晨耘,伍芳芳,蔡容燕,李春蕾,韩丽珍. 海口市2016—2019年新生儿出生缺陷情况及相关影响因素分析. 实用预防医学. 2021(07): 881-884 .  百度学术
百度学术
5. 章历红,赵灵. 高龄孕产妇孕前及孕期检查现状及影响因素分析. 中国计划生育学杂志. 2021(08): 1563-1567 .  百度学术
百度学术
6. 俞鹏,邓晓龙,袁军. 2017—2020年泰州市新生儿出生缺陷发生率调查及特征观察. 中国妇幼健康研究. 2021(09): 1245-1249 .  百度学术
百度学术
7. 刘清玲,刘长娣,杨舒. 胎儿发生先天性畸形的数据比例及影响因素的Logistic回归分析. 中国优生与遗传杂志. 2020(08): 1017-1019 .  百度学术
百度学术
其他类型引用(3)




 下载:
下载:
 苏公网安备 32100302010246号
苏公网安备 32100302010246号
