Evaluation value of systemic immune inflammation index for left ventricular hypertrophy in non-dialysis patients with chronic kidney disease
-
摘要:目的 探讨非透析的慢性肾脏病(CKD)患者左心室肥厚(LVH)的发生情况及相关危险因素, 分析全身免疫炎症指数(SII)对LVH的评估价值。方法 选取CKD患者196例为研究对象(CKD组),根据性别分为CKD男性组117例和CKD女性组79例,并选取同期40例健康者为对照组。收集并分析3组实验室指标及心脏超声资料。分析左心室质量指数(LVMI)与其他指标的相关性。采用Logistic回归分析LVH的危险因素,以及分析SII与LVH的关系。结果 男性、女性LVH患病率分别为31.62%、50.63%。收缩压(SBP)升高、血红蛋白(Hb)降低、SII升高是男性患者LVH发生的独立危险因素,而高龄、Hb降低、尿酸(UA)上升是女性患者LVH发生的独立危险因素(P<0.05)。结论 LVH在非透析的CKD患者中普遍存在,且女性患者较多。贫血是所有CKD患者LVH的危险因素, SII升高是男性患者LVH的危险因素。Abstract:Objective To investigate the incidence and risk factors of left ventricular hypertrophy (LVH) in non-dialysis patients with chronic kidney disease (CKD), and to analyze the value of systemic immune inflammation index (SII) in evaluating LVH.Methods A total of 196 non-dialysis patients with CKD were selected as study subjects (CKD group). According to gender, 196 cases were divided into male CKD group (n=117) and female CKD group (n=79), and 40 healthy subjects in the same period were selected as control group. The laboratory indexes and cardiac ultrasound data of three groups were collected and analyzed. The correlation between left ventricular mass index (LVMI) and other indexes was analyzed. Logistic regression was used to analyze the risk factors of LVH and the relationship between SII and LVH(P<0.05).Results The prevalence of LVH in male and female was 31.62% and 50.63%, respectively. Increased systolic blood pressure (SBP), decreased hemoglobin (Hb) and increased SII were independent risk factors for LVH in male patients, while older age, decreased Hb and increased uric acid (UA) were independent risk factors for LVH in female patients.Conclusion LVH is common in non-dialysis patients with CKD, and there are more female patients. Anemia is a risk factor for LVH in all CKD patients while SII is a risk factor for LVH in men.
-
慢性肾脏病(CKD)在全球的发病率为8%~16%[1], 心血管疾病(CVD)与CKD密切相关,是CKD患者主要死亡原因。左心室肥厚(LVH)是CKD患者常见的心血管并发症[2], 与患者死亡及其他心血管事件的发生密切相关[3-4], 因此需要早期识别并干预。炎症是LVH常见的危险因素[5], 研究[6-8]发现由血常规衍生的新型炎症指标如中性粒细胞与淋巴细胞比值(NLR)、血小板与淋巴细胞比值(PLR)、红细胞分布宽度与心血管事件密切相关,并证实了其在LVH中的意义。
全身免疫炎症指数(SII)是基于中性粒细胞、血小板和淋巴细胞的综合指标,能反映机体内炎症和免疫平衡状态,是一种新型的炎症标志物,对肿瘤、肝硬化有预后预测价值[9-10], 但对LVH的评估价值研究较少。本研究探讨慢性肾脏病(CKD) 非透析患者LVH发生情况及危险因素,分析SII对CKD患者LVH的评估价值。
1. 资料与方法
1.1 一般资料
选取2019—2020年在苏州大学附属第一医院肾内科住院并根据KDIGO指南诊断为CKD的非透析患者196例(CKD组),其中男117例(CKD男性组),女79例(CKD女性组)。纳入标准: 18~89岁者; 数据完整的CKD患者。排除标准: 已进入透析(包括血液透析和腹膜透析) 者; 合并急性感染性疾病者; 合并肝硬化、急性心力衰竭、恶性肿瘤、血液系统疾病者。随机选取40例同期健康体检者为对照组。
1.2 方法
收集所有入组患者的性别、年龄、体质量指数(BMI)、收缩压(SBP)、舒张压(DBP)、平均动脉压(MBP)、脉压(PP)。采集CKD患者空腹静脉血2 mL送至苏州大学附属第一医院检验科进行检测。
1.3 观察指标
检测血常规、生化全套、超敏C反应蛋白(hs-CRP)等指标,并进行如下计算: NLR=中性粒细胞计数/淋巴细胞计数; PLR=血小板计数/淋巴细胞计数; 淋巴细胞与单核细胞比值(LMR)=淋巴细胞计数/与单核细胞计数; 全身免疫炎症指数(SII)=血小板计数×(中性粒细胞计数/淋巴细胞计数)。
心脏彩色多普勒超声检查由心脏超声专职医生操作。根据美国超声心动图协会推荐的测量方法,取胸骨旁长轴切面,测量左房内径(LAD)、左心室舒张末内径(LVEDD)、左室舒张期后壁厚度(LVPWT)、室间隔厚度(IVST)、相对室壁厚度(RWT)、左室射血分数(EF)等。各参数均测量3个心动周期,取平均值。LVH诊断标准: 参照Devereux公式计算。左心室质量指数(LVMI)(g/m2)=心室质量(LVM)/体表面积。LVM(g)=0.8×1.04×[(LVEDD+IVST+LVPWT)3-(LVEDd)3]+0.6; 体表面积=0.006 1×身高(cm)+0.012 8×体质量(kg)-0.152 9; 诊断标准: 男性LVMI>115 g/m2, 女性LVMI>95 g/m2。估算肾小球滤过率(eGFR): 将血清肌酐(SCr)代入CKD-EPI公式计算得出。
1.4 统计学分析
应用SPSS 23.0软件进行统计分析。连续变量用(x±s)表示,分类变量用[n(%)]表示。正态分布资料组间比较采用t检验,非正态分布资料组间比较采用非参数检验。分类数据组间比较采用卡方检验。LVMI与各指标间的相关性采用Pearson相关分析或Spearsman相关性分析。采用单因素和多因素Logistic回归分析LVH的独立危险因素。定义检验水准为0.05, P<0.05为差异有统计学意义。
2. 结果
2.1 临床特征
CKD男性组和CKD女性组的中位LVMI分别是104.83、99.72 g/m2。与健康对照组相比, CKD患者无论男女, SBP、PP、NLR、SII、LVM、LVMI均较高,而LMR、Hb、ALB较低,差异有统计学意义(P<0.05)。见表 1、表 2。
表 1 CKD组与对照组临床指标比较(x±s)[M(P25, P75)]指标 CKD男性组(n=117) CKD女性组(n=79) 对照组(n=40) 年龄/岁 57.50(46.00, 66.00) 55.50(43.00, 67.50) 54.00(47.25, 63.00) 体质量指数/(kg/m2) 24.03(22.15, 27.16)# 22.68(20.79, 26.13) 22.98(21.22, 26.37) 收缩压/mmHg 139.50(129.75, 153.00)* 138.00(124.00, 153.50)* 124.50(115.00, 135.00) 舒张压/mmHg 81.93±10.42 78.70±11.67 79.30±12.78 平均动脉压/mmHg 101.72±10.10* 98.23±12.14 95.41±15.12 脉压/mmHg 57.75(47.00, 68.00)* 58.25(46.50, 68.75)* 45.50(40.00, 54.50) 中性粒细胞与淋巴细胞比值 2.83(1.95, 4.23)* 2.95(2.02, 4.56)* 1.71(1.37, 2.04) 淋巴细胞与单核细胞比值 2.87(2.26, 4.00)* 2.95(1.98, 4.27)* 4.77(3.85, 5.74) 血小板与淋巴细胞比值 113.23(89.84, 147.02) 116.35(93.69, 155.52) 111.05(85.49, 136.19) 全身免疫炎症指数/(×1012/L) 472.92(303.26, 663.45)* 430.50(309.39, 577.46)* 310.06(263.65, 404.09) 血红蛋白/(g/L) 121.50(96.00, 138.00)*# 108.00(87.00, 122.00)* 138.50(129.25, 153.25) 红细胞分布宽度/% 12.80(12.10, 13.40) 12.95(12.40, 13.60) 12.50(12.03, 13.20) 血小板/(×1012/L) 195.25±61.87 206.62±70.29 199.56±63.49 碱性磷酸酶/(U/L) 64.70(54.30, 82.30) 59.95(45.75, 85.10) 61.35(50.30, 71.68) 白蛋白/(g/L) 38.45(34.10, 41.70)* 38.45(34.5, 42.00)* 43.75(42.75, 46.48) 尿素氮/(mmol/L) 11.20(7.70, 22.80)* 12.30(5.90, 21.45)* 5.45(4.60, 6.18) 血清肌酐/(μmol/L) 201.00(129.30, 393.30)* 201.05(83.05, 383.00)* 62.00(52.98, 71.40) 尿酸/(μmol/L) 438.90(373.20, 519.50)*# 399.65(326.40, 491.15)* 337.70(275.73, 389.25) 血糖/(mmol/L) 4.88(4.39, 5.39) 4.84(4.41, 5.74) 4.89(4.49, 5.39) 总胆固醇/(mmol/L) 4.42(3.83, 5.15)# 4.94(4.275, 5.85) 4.80(4.29, 5.54) 甘油三酯/(mmol/L) 1.47(1.08, 2.24)* 1.51(1.15, 2.36)* 1.20(0.82, 1.44) 高密度脂蛋白胆固醇/(mmol/L) 0.97(0.79, 1.14)* 1.22(0.97, 1.45)* 1.26(1.06, 1.56) 低密度脂蛋白胆固醇/(mmol/L) 2.53(1.79, 3.33) 2.66(2.00, 3.31) 3.01(2.39, 3.38) 钙/(mmol/L) 2.21(2.11, 2.32) 2.21(2.13, 2.33) - 磷/(mmol/L) 1.25(1.06, 1.53) 1.35(1.20, 1.54) - 超敏C反应蛋白/(mg/L) 1.35(0.47, 2.95)* 0.98(0.35, 3.29)* 1.72(1.44, 2.84) eGFR/[mL/(min·1.73 m2)] 29.08(12.60, 52.05)* 23.65(11.14, 72.50)* 105.03(98.91, 118.54) eGFR: 估算肾小球滤过率。与对照组比较, *P<0.05; 与CKD女性组比较, #P<0.05。 表 2 CKD组与对照组心脏超声指标比较[M(P25, P75)][n(%)]指标 CKD男性组(n=117) CKD女性组(n=79) 对照组(n=40) 左房内径/mm 38.00(35.00, 42.00)* 38.00(33.50, 41.50)* 34.00(32.00, 38.00) 室间隔厚度/mm 10.00(9.00, 11.00)*# 9.00(9.00, 10.00)* 9.00(8.00, 9.00) 左心室舒张末内径/mm 51.00(47.00, 54.00)*# 47.50(44.00, 51.00) 46.00(43.25, 49.00) 左室舒张期后壁厚度/mm 10.00(9.00, 10.00)* 9.00(8.50, 10.00)* 9.00(8.00, 9.75) 左心室质量/g 181.98(153.42, 213.18)*# 153.09(127.73, 175.61)* 135.79(109.44, 164.13) 左心室质量指数/(g/m2) 104.90(83.20, 120.84)* 95.87(84.23, 114.70)* 79.61(69.89, 95.13) 相对室壁厚度/mm 0.39(0.36, 0.42) 0.38(0.36, 0.41) 0.37(0.35, 0.40) EF值/% 65.00(61.00, 69.00)* 67.00(63.00, 69.00) 67.00(65.00, 69.00) 左心室肥厚 37(31.62) 40(50.63) - EF: 射血分数。与对照组比较, *P<0.05; 与CKD女性组比较, #P<0.05。 2.2 CKD患者LVH发生情况
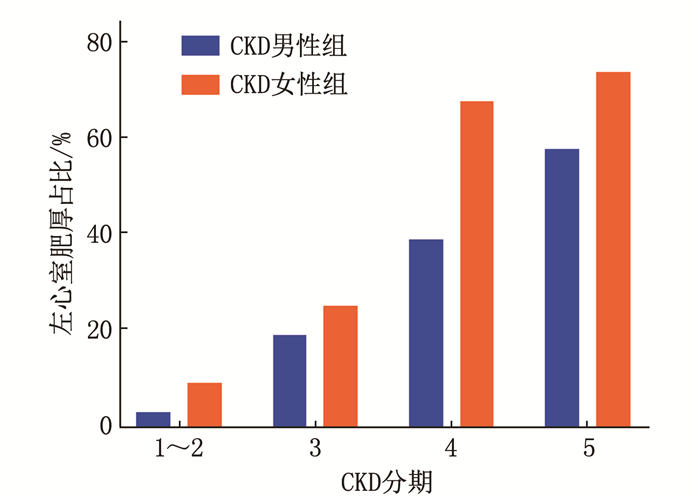
196例患者中有77例诊断为LVH, LVH发生率为39.29%。CKD男性组和CKD女性组中LVH的占比分别为31.62%(37/117)、50.63%(40/79), 2组差异有统计学意义(P<0.05)。随着eGFR的降低,无论是男性还是女性, LVH的占比逐渐升高,见图 1。
2.3 LVMI与临床指标的相关性分析
CKD男性组患者LVMI与SBP、PP、PLR、SII、RDW、尿素氮(UN)、SCr、磷(P)呈正相关(P<0.05), 与Hb、ALB、TC、高密度脂蛋白胆固醇(HDL-C)、低密度脂蛋白胆固醇(LDL-C)、钙(Ca)、eGFR呈负相关(P<0.05)。CKD女性组患者LVMI与年龄、SBP、PP、红细胞分布宽度(RDW)、UN、SCr、UA呈正相关(P<0.05), 与Hb、PLT、TC、HDL-C、LDL-C、Ca、eGFR呈负相关(P<0.05)。见表 3。
表 3 LVMI与临床指标的相关性分析自变量 CKD男性组(n=117) CKD女性组(n=79) r P r P 年龄/岁 0.109 0.242 0.482 < 0.001 体质量指数/(kg/m2) 0.053 0.570 -0.074 0.516 收缩压/mmHg 0.411 < 0.001 0.366 0.001 舒张压/mmHg -0.130 0.163 -0.139 0.221 平均动脉压/mmHg 0.131 0.158 0.101 0.377 脉压/mmHg 0.477 < 0.001 0.509 < 0.001 中性粒细胞与淋巴细胞比值 -0.003 0.978 -0.093 0.415 淋巴细胞与单核细胞比值 0.086 0.357 0.129 0.258 血小板与淋巴细胞比值 0.277 0.002 0.024 0.834 全身免疫炎症指数/(×1012/L) 0.284 0.002 -0.050 0.659 血红蛋白/(g/L) -0.635 < 0.001 -0.625 < 0.001 红细胞分布宽度/% 0.373 < 0.001 0.318 0.004 血小板/(×1012/L) -0.106 0.255 -0.394 < 0.001 碱性磷酸酶/(U/L) 0.046 0.619 0.177 0.119 白蛋白/(g/L) -0.204 0.027 -0.083 0.469 尿素氮/(mmol/L) 0.537 < 0.001 0.576 < 0.001 血清肌酐/(μmol/L) 0.615 < 0.001 0.585 < 0.001 尿酸/(μmol/L) 0.007 0.944 0.413 < 0.001 血糖/(mmol/L) 0.030 0.748 -0.085 0.457 总胆固醇/(mmol/L) -0.264 0.004 -0.246 0.029 甘油三酯/(mmol/L) -0.097 0.299 0.108 0.342 高密度脂蛋白胆固醇/(mmol/L) -0.260 0.005 -0.336 0.002 低密度脂蛋白胆固醇/(mmol/L) -0.226 0.014 -0.330 0.003 钙/(mmol/L) -0.377 < 0.001 -0.257 0.022 磷/(mmol/L) 0.415 < 0.001 0.213 0.059 超敏C反应蛋白/(mg/L) -0.064 0.496 0.021 0.853 eGFR/[mL/(min·1.73 m2)] -0.398 < 0.001 -0.487 < 0.001 eGFR: 估算肾小球滤过率。 2.4 LVH影响因素分析
在CKD男性组患者中, SBP、PP、PLR、SII、RDW、UN、SCr、P是其发生LVH的危险因素,而Hb、TC、HDL-C、Ca、eGFR是其保护因素。将单因素分析有意义的变量纳入多因素回归分析,结果显示SBP及SII值越高, Hb越低,患者发生LVH的风险越高。在CKD女性组患者中,年龄、SBP、PP、RDW、UN、SCr、UA是患者发生LVH的危险因素,而Hb、PLT、TC、HDL-C、LDL-C、eGFR则是其保护因素。将单因素分析有意义的变量纳入多因素回归分析,结果显示年龄及UA值越高, Hb越低,患者发生LVH的风险越高。见表 4、表 5。
表 4 影响CKD男性组患者LVH的Logistic回归分析自变量 单因素Logistic回归分析 多因素Logistic回归分析 OR(95%CI) P OR(95%CI) P 年龄/岁 1.010(0.984~1.036) 0.461 - - 体质量指数/(kg/m2) 1.063(0.946~1.194) 0.306 - - 收缩压/mmHg 1.056(1.025~1.087) < 0.001 1.033(1.001~1.066) 0.043 舒张压/mmHg 0.992(0.955~1.030) 0.662 - - 平均动脉压/mmHg 1.037(0.996~1.080) 0.079 - - 脉压/mmHg 1.057(1.028~1.087) < 0.001 - - 中性粒细胞与淋巴细胞比值 1.142(0.888~1.467) 0.300 - - 淋巴细胞与单核细胞比值 1.169(0.867~1.574) 0.305 - - 血小板与淋巴细胞比值 1.013(1.005~1.022) 0.003 - - 全身免疫炎症指数/(×1012/L) 1.002(1.001~1.004) 0.001 1.002(1.001~1.004) 0.009 血红蛋白/(g/L) 0.959(0.942~0.976) < 0.001 0.962(0.943~0.981) < 0.001 红细胞分布宽度/% 1.822(1.235~2.687) 0.003 - - 血小板/(×1012/L) 0.999(0.993~1.005) 0.744 - - 碱性磷酸酶/(U/L) 1.017(0.999~1.034) 0.066 - - 白蛋白/(g/L) 0.955(0.897~1.017) 0.151 - - 尿素氮/(mmol/L) 1.073(1.032~1.115) < 0.001 - - 血清肌酐/(μmol/L) 1.004(1.002~1.006) < 0.001 - - 尿酸/(μmol/L) 1.002(0.999~1.006) 0.223 - - 血糖/(mmol/L) 1.141(0.879~1.481) 0.320 - - 总胆固醇/(mmol/L) 0.669(0.461~0.970) 0.034 - - 甘油三酯/(mmol/L) 0.746(0.500~1.114) 0.152 - - 高密度脂蛋白胆固醇/(mmol/L) 0.179(0.039~0.821) 0.027 - - 低密度脂蛋白胆固醇/(mmol/L) 0.724(0.491~1.067) 0.103 - - 钙/(mmol/L) 0.005(0~0.100) 0.001 - - 磷/(mmol/L) 4.238(1.609~11.166) 0.003 - - 超敏C反应蛋白/(mg/L) 1.019(0.898~1.157) 0.769 - - eGFR/[mL/(min·1.73 m2)] 0.973(0.956~0.990) 0.002 - - eGFR: 估算肾小球滤过率。 表 5 影响CKD女性组患者LVH的Logistic回归分析自变量 单因素Logistic回归分析 多因素Logistic回归分析 OR(95%CI) P OR(95%CI) P 年龄/岁 1.068(1.031~1.107) < 0.001 1.064(1.019~1.111) 0.005 体质量指数/(kg/m2) 1.005(0.909~1.111) 0.919 - - 收缩压/mmHg 1.032(1.006~1.059) 0.017 - - 舒张压/mmHg 0.970(0.932~1.009) 0.133 - - 平均动脉压/mmHg 1.006(0.970~1.043) 0.761 - - 脉压/mmHg 1.068(1.029~1.108) 0.001 - - 中性粒细胞与淋巴细胞比值 0.929(0.731~1.181) 0.548 - - 淋巴细胞与单核细胞比值 1.044(0.795~1.371) 0.756 - - 血小板与淋巴细胞比值 0.998(0.990~1.005) 0.543 - - 全身免疫炎症指数/(×1012/L) 1.000(0.999~1.001) 0.923 - - 血红蛋白/(g/L) 0.942(0.916~0.969) < 0.001 0.953(0.926~0.982) 0.002 红细胞分布宽度/% 1.593(1.041~2.439) 0.032 - - 血小板/(×1012/L) 0.986(0.977~0.994) 0.001 - - 碱性磷酸酶/(U/L) 1.013(0.995~1.032) 0.150 - - 白蛋白/(g/L) 0.999(0.938~1.064) 0.974 - - 尿素氮/(mmol/L) 1.095(1.036~1.157) 0.001 - - 血清肌酐/(μmol/L) 1.004(1.002~1.007) 0.001 - - 尿酸/(μmol/L) 1.006(1.002~1.011) 0.004 1.006(1.001~1.012) 0.031 血糖/(mmol/L) 0.735(0.507~1.064) 0.102 - - 总胆固醇/(mmol/L) 0.578(0.372~0.898) 0.015 - - 甘油三酯/(mmol/L) 0.957(0.664~1.380) 0.814 - - 高密度脂蛋白胆固醇/(mmol/L) 0.148(0.035~0.618) 0.009 - - 低密度脂蛋白胆固醇/(mmol/L) 0.457(0.262~0.795) 0.006 - - 钙/(mmol/L) 0.056(0.002~1.288) 0.072 - - 磷/(mmol/L) 4.108(0.965~7.482) 0.056 - - 超敏C反应蛋白/(mg/L) 1.027(0.916~1.152) 0.650 - - eGFR/(mL/min/1.73 m2) 0.970(0.954~0.986) < 0.001 - - eGFR: 估算肾小球滤过率。 3. 讨论
心血管事件的发生随着肾功能减退逐渐增加[11], 合并CVD的CKD患者病死率远高于普通CKD患者。心血管事件包括冠心病、心力衰竭、心室肥厚等。LVH作为CKD患者心脏病变的重要特征,在CKD患者中普遍存在[12], 且与上述心血管事件及全因死亡密切相关[3-4]。CKD患者较高LVH患病率的原因除了高血压、糖尿病等因素外,炎症可能在LVH的发展过程中具有重要作用。研究[6-8]发现NLR、PLR、RDW等新型炎症指标与LVH密切相关,但是反映机体炎症和免疫平衡状态的指标SII是否与LVH有更密切关联的研究较少。
本研究中, CKD患者LVH患病率为39.29%, 与男性相比,女性患病率更高,与侯凡凡等[13]调查结果一致。造成这种现象的原因可能为绝经后女性体内激素水平变化相关。既往研究[14-15]表明,雌激素可通过改善脂质代谢、抗氧化等多种途径对心血管发生具有保护作用。本研究中,女性中位年龄为55.50岁,考虑其高LVH患病率可能与该类女性雌激素水平较低有关。此外,本研究发现,随着eGFR的降低,无论男性还是女性, LVH的患病率逐渐升高,与既往研究[2]结果相符。高血压患者同时存在压力、容量负荷, 2种负荷均可增加心肌细胞容积、改变胶原蛋白基质的成分,最终引起肥厚[16-17]。CKD患者由于肾素-血管紧张素-醛固酮系统(RAAS)及交感神经系统激活等因素,往往合并有难以控制的高血压。本研究发现, SBP是男性CKD患者的危险因素,但未观察到血压独立于其他因素与女性患者LVH之间的关系,可能与本研究中女性患者样本量相对较少、血压控制程度相对较好有关。
炎症因子不仅可影响血管内皮功能,诱导趋化因子表达,引起炎性细胞的聚集和浸润,导致炎性损伤; 还可直接导致细胞增殖、凋亡,调节细胞外间质的合成和降解,从而参与心脏重构[5]。此外,氧化应激也是参与LVH发生发展的重要原因之一[18], 炎症与氧化应激过程相互影响,共同促进LVH的发生。CKD患者体内处于微炎症状态,本研究中,与对照组相比, CKD组患者NLR、SII等反映炎症状态的指标水平较高。行LVH危险因素分析提示, SII是男性患者LVH的独立危险因素。众多炎症指标中,仅SII与LVH发生独立相关,而与由血常规检测获得的其他炎症指标,如NLR、LMR、PLR、RDW则未发现与LVH发生的独立相关性,显示SII更能够全面地反映机体内炎症和免疫平衡状态,对LVH的发生影响更大。女性CKD患者多因素分析未发现炎症指标与LVH的关系密切,可能与女性患者样本较少有关; 此外,有研究[19]显示,血管紧张素受体阻滞剂(ARB)类药物可减少炎症因子产生,本研究中因未记录患者用药种类,也有可能影响研究结果。
Hb降低是LVMI增加主要的危险因素[20]。贫血不仅会加重心肌缺血,还会降低血液的粘滞度,导致静脉回心血量增多,使机体处于慢性容量超载的状态,而心脏容量负荷增加也是导致心室肥厚的重要因素之一。此外,低Hb浓度可能导致内皮来源的舒张因子(一氧化氮)的可用性提高,从而导致血管扩张和心输出量增加[21]。本研究中,无论女性还是男性, Hb降低均是CKD患者LVH发生的危险因素。机体处于炎症状态时,肝脏合成铁调素增加,影响机体铁释放,从而加重了患者贫血的程度,因此炎症在贫血对LVH的影响上也具有重要的作用。研究[22]显示,在使用促红细胞生成素纠正贫血后,患者LVH有所逆转,且心功能也得到改善,因而纠正CKD患者的贫血对防治LVH有重要意义。
综上所述, LVH在CKD患者中普遍存在,且女性患者较高。贫血是所有CKD患者LVH的危险因素。新型炎症指标SII是男性患者LVH的危险因素,而在女性患者中未发现SII与LVH具有相关性。由血常规衍生出的SII,在临床中获取简单,经济适用,有望成为早期干预并延缓LVH发生的指标。本研究为单中心横断面研究,样本量相对较少、未记录患者用药情况,因此SII对于LVH的评估价值还需进一步验证。此外, SII对于CKD患者远期预后也有待进一步研究。
-
表 1 CKD组与对照组临床指标比较(x±s)[M(P25, P75)]
指标 CKD男性组(n=117) CKD女性组(n=79) 对照组(n=40) 年龄/岁 57.50(46.00, 66.00) 55.50(43.00, 67.50) 54.00(47.25, 63.00) 体质量指数/(kg/m2) 24.03(22.15, 27.16)# 22.68(20.79, 26.13) 22.98(21.22, 26.37) 收缩压/mmHg 139.50(129.75, 153.00)* 138.00(124.00, 153.50)* 124.50(115.00, 135.00) 舒张压/mmHg 81.93±10.42 78.70±11.67 79.30±12.78 平均动脉压/mmHg 101.72±10.10* 98.23±12.14 95.41±15.12 脉压/mmHg 57.75(47.00, 68.00)* 58.25(46.50, 68.75)* 45.50(40.00, 54.50) 中性粒细胞与淋巴细胞比值 2.83(1.95, 4.23)* 2.95(2.02, 4.56)* 1.71(1.37, 2.04) 淋巴细胞与单核细胞比值 2.87(2.26, 4.00)* 2.95(1.98, 4.27)* 4.77(3.85, 5.74) 血小板与淋巴细胞比值 113.23(89.84, 147.02) 116.35(93.69, 155.52) 111.05(85.49, 136.19) 全身免疫炎症指数/(×1012/L) 472.92(303.26, 663.45)* 430.50(309.39, 577.46)* 310.06(263.65, 404.09) 血红蛋白/(g/L) 121.50(96.00, 138.00)*# 108.00(87.00, 122.00)* 138.50(129.25, 153.25) 红细胞分布宽度/% 12.80(12.10, 13.40) 12.95(12.40, 13.60) 12.50(12.03, 13.20) 血小板/(×1012/L) 195.25±61.87 206.62±70.29 199.56±63.49 碱性磷酸酶/(U/L) 64.70(54.30, 82.30) 59.95(45.75, 85.10) 61.35(50.30, 71.68) 白蛋白/(g/L) 38.45(34.10, 41.70)* 38.45(34.5, 42.00)* 43.75(42.75, 46.48) 尿素氮/(mmol/L) 11.20(7.70, 22.80)* 12.30(5.90, 21.45)* 5.45(4.60, 6.18) 血清肌酐/(μmol/L) 201.00(129.30, 393.30)* 201.05(83.05, 383.00)* 62.00(52.98, 71.40) 尿酸/(μmol/L) 438.90(373.20, 519.50)*# 399.65(326.40, 491.15)* 337.70(275.73, 389.25) 血糖/(mmol/L) 4.88(4.39, 5.39) 4.84(4.41, 5.74) 4.89(4.49, 5.39) 总胆固醇/(mmol/L) 4.42(3.83, 5.15)# 4.94(4.275, 5.85) 4.80(4.29, 5.54) 甘油三酯/(mmol/L) 1.47(1.08, 2.24)* 1.51(1.15, 2.36)* 1.20(0.82, 1.44) 高密度脂蛋白胆固醇/(mmol/L) 0.97(0.79, 1.14)* 1.22(0.97, 1.45)* 1.26(1.06, 1.56) 低密度脂蛋白胆固醇/(mmol/L) 2.53(1.79, 3.33) 2.66(2.00, 3.31) 3.01(2.39, 3.38) 钙/(mmol/L) 2.21(2.11, 2.32) 2.21(2.13, 2.33) - 磷/(mmol/L) 1.25(1.06, 1.53) 1.35(1.20, 1.54) - 超敏C反应蛋白/(mg/L) 1.35(0.47, 2.95)* 0.98(0.35, 3.29)* 1.72(1.44, 2.84) eGFR/[mL/(min·1.73 m2)] 29.08(12.60, 52.05)* 23.65(11.14, 72.50)* 105.03(98.91, 118.54) eGFR: 估算肾小球滤过率。与对照组比较, *P<0.05; 与CKD女性组比较, #P<0.05。 表 2 CKD组与对照组心脏超声指标比较[M(P25, P75)][n(%)]
指标 CKD男性组(n=117) CKD女性组(n=79) 对照组(n=40) 左房内径/mm 38.00(35.00, 42.00)* 38.00(33.50, 41.50)* 34.00(32.00, 38.00) 室间隔厚度/mm 10.00(9.00, 11.00)*# 9.00(9.00, 10.00)* 9.00(8.00, 9.00) 左心室舒张末内径/mm 51.00(47.00, 54.00)*# 47.50(44.00, 51.00) 46.00(43.25, 49.00) 左室舒张期后壁厚度/mm 10.00(9.00, 10.00)* 9.00(8.50, 10.00)* 9.00(8.00, 9.75) 左心室质量/g 181.98(153.42, 213.18)*# 153.09(127.73, 175.61)* 135.79(109.44, 164.13) 左心室质量指数/(g/m2) 104.90(83.20, 120.84)* 95.87(84.23, 114.70)* 79.61(69.89, 95.13) 相对室壁厚度/mm 0.39(0.36, 0.42) 0.38(0.36, 0.41) 0.37(0.35, 0.40) EF值/% 65.00(61.00, 69.00)* 67.00(63.00, 69.00) 67.00(65.00, 69.00) 左心室肥厚 37(31.62) 40(50.63) - EF: 射血分数。与对照组比较, *P<0.05; 与CKD女性组比较, #P<0.05。 表 3 LVMI与临床指标的相关性分析
自变量 CKD男性组(n=117) CKD女性组(n=79) r P r P 年龄/岁 0.109 0.242 0.482 < 0.001 体质量指数/(kg/m2) 0.053 0.570 -0.074 0.516 收缩压/mmHg 0.411 < 0.001 0.366 0.001 舒张压/mmHg -0.130 0.163 -0.139 0.221 平均动脉压/mmHg 0.131 0.158 0.101 0.377 脉压/mmHg 0.477 < 0.001 0.509 < 0.001 中性粒细胞与淋巴细胞比值 -0.003 0.978 -0.093 0.415 淋巴细胞与单核细胞比值 0.086 0.357 0.129 0.258 血小板与淋巴细胞比值 0.277 0.002 0.024 0.834 全身免疫炎症指数/(×1012/L) 0.284 0.002 -0.050 0.659 血红蛋白/(g/L) -0.635 < 0.001 -0.625 < 0.001 红细胞分布宽度/% 0.373 < 0.001 0.318 0.004 血小板/(×1012/L) -0.106 0.255 -0.394 < 0.001 碱性磷酸酶/(U/L) 0.046 0.619 0.177 0.119 白蛋白/(g/L) -0.204 0.027 -0.083 0.469 尿素氮/(mmol/L) 0.537 < 0.001 0.576 < 0.001 血清肌酐/(μmol/L) 0.615 < 0.001 0.585 < 0.001 尿酸/(μmol/L) 0.007 0.944 0.413 < 0.001 血糖/(mmol/L) 0.030 0.748 -0.085 0.457 总胆固醇/(mmol/L) -0.264 0.004 -0.246 0.029 甘油三酯/(mmol/L) -0.097 0.299 0.108 0.342 高密度脂蛋白胆固醇/(mmol/L) -0.260 0.005 -0.336 0.002 低密度脂蛋白胆固醇/(mmol/L) -0.226 0.014 -0.330 0.003 钙/(mmol/L) -0.377 < 0.001 -0.257 0.022 磷/(mmol/L) 0.415 < 0.001 0.213 0.059 超敏C反应蛋白/(mg/L) -0.064 0.496 0.021 0.853 eGFR/[mL/(min·1.73 m2)] -0.398 < 0.001 -0.487 < 0.001 eGFR: 估算肾小球滤过率。 表 4 影响CKD男性组患者LVH的Logistic回归分析
自变量 单因素Logistic回归分析 多因素Logistic回归分析 OR(95%CI) P OR(95%CI) P 年龄/岁 1.010(0.984~1.036) 0.461 - - 体质量指数/(kg/m2) 1.063(0.946~1.194) 0.306 - - 收缩压/mmHg 1.056(1.025~1.087) < 0.001 1.033(1.001~1.066) 0.043 舒张压/mmHg 0.992(0.955~1.030) 0.662 - - 平均动脉压/mmHg 1.037(0.996~1.080) 0.079 - - 脉压/mmHg 1.057(1.028~1.087) < 0.001 - - 中性粒细胞与淋巴细胞比值 1.142(0.888~1.467) 0.300 - - 淋巴细胞与单核细胞比值 1.169(0.867~1.574) 0.305 - - 血小板与淋巴细胞比值 1.013(1.005~1.022) 0.003 - - 全身免疫炎症指数/(×1012/L) 1.002(1.001~1.004) 0.001 1.002(1.001~1.004) 0.009 血红蛋白/(g/L) 0.959(0.942~0.976) < 0.001 0.962(0.943~0.981) < 0.001 红细胞分布宽度/% 1.822(1.235~2.687) 0.003 - - 血小板/(×1012/L) 0.999(0.993~1.005) 0.744 - - 碱性磷酸酶/(U/L) 1.017(0.999~1.034) 0.066 - - 白蛋白/(g/L) 0.955(0.897~1.017) 0.151 - - 尿素氮/(mmol/L) 1.073(1.032~1.115) < 0.001 - - 血清肌酐/(μmol/L) 1.004(1.002~1.006) < 0.001 - - 尿酸/(μmol/L) 1.002(0.999~1.006) 0.223 - - 血糖/(mmol/L) 1.141(0.879~1.481) 0.320 - - 总胆固醇/(mmol/L) 0.669(0.461~0.970) 0.034 - - 甘油三酯/(mmol/L) 0.746(0.500~1.114) 0.152 - - 高密度脂蛋白胆固醇/(mmol/L) 0.179(0.039~0.821) 0.027 - - 低密度脂蛋白胆固醇/(mmol/L) 0.724(0.491~1.067) 0.103 - - 钙/(mmol/L) 0.005(0~0.100) 0.001 - - 磷/(mmol/L) 4.238(1.609~11.166) 0.003 - - 超敏C反应蛋白/(mg/L) 1.019(0.898~1.157) 0.769 - - eGFR/[mL/(min·1.73 m2)] 0.973(0.956~0.990) 0.002 - - eGFR: 估算肾小球滤过率。 表 5 影响CKD女性组患者LVH的Logistic回归分析
自变量 单因素Logistic回归分析 多因素Logistic回归分析 OR(95%CI) P OR(95%CI) P 年龄/岁 1.068(1.031~1.107) < 0.001 1.064(1.019~1.111) 0.005 体质量指数/(kg/m2) 1.005(0.909~1.111) 0.919 - - 收缩压/mmHg 1.032(1.006~1.059) 0.017 - - 舒张压/mmHg 0.970(0.932~1.009) 0.133 - - 平均动脉压/mmHg 1.006(0.970~1.043) 0.761 - - 脉压/mmHg 1.068(1.029~1.108) 0.001 - - 中性粒细胞与淋巴细胞比值 0.929(0.731~1.181) 0.548 - - 淋巴细胞与单核细胞比值 1.044(0.795~1.371) 0.756 - - 血小板与淋巴细胞比值 0.998(0.990~1.005) 0.543 - - 全身免疫炎症指数/(×1012/L) 1.000(0.999~1.001) 0.923 - - 血红蛋白/(g/L) 0.942(0.916~0.969) < 0.001 0.953(0.926~0.982) 0.002 红细胞分布宽度/% 1.593(1.041~2.439) 0.032 - - 血小板/(×1012/L) 0.986(0.977~0.994) 0.001 - - 碱性磷酸酶/(U/L) 1.013(0.995~1.032) 0.150 - - 白蛋白/(g/L) 0.999(0.938~1.064) 0.974 - - 尿素氮/(mmol/L) 1.095(1.036~1.157) 0.001 - - 血清肌酐/(μmol/L) 1.004(1.002~1.007) 0.001 - - 尿酸/(μmol/L) 1.006(1.002~1.011) 0.004 1.006(1.001~1.012) 0.031 血糖/(mmol/L) 0.735(0.507~1.064) 0.102 - - 总胆固醇/(mmol/L) 0.578(0.372~0.898) 0.015 - - 甘油三酯/(mmol/L) 0.957(0.664~1.380) 0.814 - - 高密度脂蛋白胆固醇/(mmol/L) 0.148(0.035~0.618) 0.009 - - 低密度脂蛋白胆固醇/(mmol/L) 0.457(0.262~0.795) 0.006 - - 钙/(mmol/L) 0.056(0.002~1.288) 0.072 - - 磷/(mmol/L) 4.108(0.965~7.482) 0.056 - - 超敏C反应蛋白/(mg/L) 1.027(0.916~1.152) 0.650 - - eGFR/(mL/min/1.73 m2) 0.970(0.954~0.986) < 0.001 - - eGFR: 估算肾小球滤过率。 -
[1] JHA V, GARCIA-GARCIA G, ISEKI K, et al. Chronic kidney disease: global dimension and perspectives[J]. Lancet, 2013, 382(9888): 260-272. doi: 10.1016/S0140-6736(13)60687-X
[2] PARK M, HSU C Y, LI Y M, et al. Associations between kidney function and subclinical cardiac abnormalities in CKD[J]. J Am Soc Nephrol, 2012, 23(10): 1725-1734. doi: 10.1681/ASN.2012020145
[3] LONDON G M, PANNIER B, GUERIN A P, et al. Alterations of left ventricular hypertrophy in and survival of patients receiving hemodialysis: follow-up of an interventional study[J]. J Am Soc Nephrol, 2001, 12(12): 2759-2767. doi: 10.1681/ASN.V12122759
[4] ZOCCALI C, BENEDETTO F A, MALLAMACI F, et al. Left ventricular mass monitoring in the follow-up of dialysis patients: prognostic value of left ventricular hypertrophy progression[J]. Kidney Int, 2004, 65(4): 1492-1498. doi: 10.1111/j.1523-1755.2004.00530.x
[5] MASIHA S, SUNDSTRÖM J, LIND L. Inflammatory markers are associated with left ventricular hypertrophy and diastolic dysfunction in a population-based sample of elderly men and women[J]. J Hum Hypertens, 27(1): 13-17. doi: 10.1038/jhh.2011.113
[6] 卢进, 张洪旭, 张育琴, 等. 维持性血液透析患者发生左心室肥厚的影响因素及RDW、hs-CRP的预测价值[J]. 中国医药导报, 2020, 17(12): 185-188. https://www.cnki.com.cn/Article/CJFDTOTAL-YYCY202012047.htm [7] 权钰迪, 周巧, 冯锦红, 等. 控制营养状态评分和血小板/淋巴细胞比值与腹膜透析患者左心室肥厚的关系[J]. 临床肾脏病杂志, 2020, 20(12): 946-950. doi: 10.3969/j.issn.1671-2390.2020.12.003 [8] 史倩雯, 胡雅玲, 范彦君, 等. 维持性血液透析患者中性粒细胞/淋巴细胞比值与左心室肥厚的临床研究[J]. 中国中西医结合肾病杂志, 2020, 21(1): 49-52. doi: 10.3969/j.issn.1009-587X.2020.01.016 [9] 韩博, 吴舜, 何先东, 等. 基于免疫细胞计数的系统性炎症反应指数在预测肾透明细胞癌患者预后中的作用研究[J]. 免疫学杂志, 2020, 36(2): 160-164, 184. https://www.cnki.com.cn/Article/CJFDTOTAL-MYXZ202002014.htm [10] 罗永祥, 周涛. 全身免疫炎症指数对失代偿期肝硬化患者预后的评估价值[J]. 中国肝脏病杂志: 电子版, 2021, 13(1): 52-58. doi: 10.3969/j.issn.1674-7380.2021.01.009 [11] STEVENS L A, LI S Y, WANG C C, et al. Prevalence of CKD and comorbid illness in elderly patients in the United States: results from the Kidney Early Evaluation Program (KEEP)[J]. Am J Kidney Dis, 2010, 55(3 Suppl 2): S23-S33.
[12] PAOLETTI E, BELLINO D, CASSOTTANA P, et al. Left ventricular hypertrophy in nondiabetic predialysis CKD[J]. Am J Kidney Dis, 2005, 46(2): 320-327. doi: 10.1053/j.ajkd.2005.04.031
[13] 侯凡凡, 马志刚, 梅长林, 等. 中国五省市自治区慢性肾脏病患者心血管疾病的患病率调查[J]. 中华医学杂志, 2005, 85(7): 458-463. doi: 10.3760/j:issn:0376-2491.2005.07.009 [14] 肖玉枝. 性激素在女性心血管疾病中的作用研究[J]. 中外健康文摘, 2010, 7(11): 104-106. [15] 王朝霞, 吕吉元. 绝经后雌激素补充治疗与女性心血管疾病关系研究进展[J]. 中西医结合心脑血管病杂志, 2015, 13(4): 502-505. doi: 10.3969/j.issn.16721349.2015.04.029 [16] 孙宁玲, CHEN J W, 王继光, 等. 亚洲高血压合并左心室肥厚诊治专家共识[J]. 中华高血压杂志, 2016, 24(7): 619-627, 600. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGGZ201607008.htm [17] 冉兵, 晁玥, 安县朝, 等. 高血压左室肥厚伴左心衰竭的心脏彩超诊断分析[J]. 实用临床医药杂志, 2017, 21(23): 122-123. doi: 10.7619/jcmp.201723045 [18] DI LULLO L, GORINI A, RUSSO D, et al. Left ventricular hypertrophy in chronic kidney disease patients: from pathophysiology to treatment[J]. Cardiorenal Med, 2015, 5(4): 254-266. doi: 10.1159/000435838
[19] YOUSIF N G, HADI N R, AL-AMRAN F, et al. Cardioprotective effects of irbesartan in polymicrobial Sepsis: the role of the p38MAPK/NF-κB signaling pathway[J]. Herz, 2018, 43(2): 140-145.
[20] MATSUMOTO M, IO H, FURUKAWA M, et al. Risk factors associated with increased left ventricular mass index in chronic kidney disease patients evaluated using echocardiography[J]. J Nephrol, 2012, 25(5): 794-801. doi: 10.5301/jn.5000066
[21] LONDON G M. Left ventricular hypertrophy: why does it happen[J]. Nephrol Dial Transplant, 2003, 18(Suppl 8): viii2-viii6.
[22] PORTOLÉS J, TORRALBO A, MARTIN P, et al. Cardiovascular effects of recombinant human erythropoietin in predialysis patients[J]. Am J Kidney Dis, 1997, 29(4): 541-548.
-
期刊类型引用(23)
1. 邓玉珍. 健身气功八段锦锻炼结合睡眠干预对改善冠心病行冠状动脉介入术患者生活质量的效果观察. 心血管病防治知识. 2024(03): 68-72 .  百度学术
百度学术
2. 王妍蝶,时贤君,秦庆祝. 认知行为干预结合健康教育对提高冠心病行经皮冠状动脉介入术后患者自我管理能力的效果. 慢性病学杂志. 2024(07): 1017-1020 .  百度学术
百度学术
3. 刘翠琴,郭小燕. 基于运动疗法的康复护理对风湿性心脏病瓣膜置换患者术后的影响. 心血管病防治知识. 2024(10): 135-137 .  百度学术
百度学术
4. 余媛媛,贺泽霞,张永佳,兰富霞,徐英. 4C干预模式对老年经皮冠状动脉介入术后患者的影响. 实用临床医药杂志. 2023(16): 68-71 .  本站查看
本站查看
5. 梁夷凤. 冠心病患者PCI术后应用基于5E理念的综合康复护理的效果分析. 中外医疗. 2023(23): 155-159 .  百度学术
百度学术
6. 吴伟,高鹃. 双心护理模式对冠心病经皮冠状动脉介入治疗患者心理健康状况和护理满意度的影响观察. 基层医学论坛. 2022(03): 87-89 .  百度学术
百度学术
7. 吴张平. 早期心脏康复训练对PCI术后患者的影响. 继续医学教育. 2022(05): 125-128 .  百度学术
百度学术
8. 牛杜娟,尚雯,张红. 以FTS理论为指导的系统化护理模式对PCI术后患者心功能的影响. 保健医学研究与实践. 2022(07): 82-85 .  百度学术
百度学术
9. 王琳,张亚铮,袁媛. 基于CSMS量表和CQQC的5E康复护理在冠心病PCI术后患者康复中的应用效果. 河北医药. 2022(14): 2228-2231 .  百度学术
百度学术
10. 刘娟,刘芳,张静. 临床护理路径在冠状动脉搭桥术患者术后康复中的应用效果研究. 中西医结合心血管病电子杂志. 2022(11): 4-6+13 .  百度学术
百度学术
11. 贾艳静,王新宙. 优质护理应用于老年冠心病患者护理中对患者生活质量和疗效的影响. 中国药物与临床. 2021(08): 1409-1411 .  百度学术
百度学术
12. 邹蓉蓉,李天兰,吴莉玫,尹艳华. 优化康复护理流程对PCl术后患者心肺功能以及预后的影响分析. 心血管病防治知识. 2021(04): 59-61+64 .  百度学术
百度学术
13. 宋敏. 整体化康复护理措施在冠心病患者中的应用. 黑龙江中医药. 2021(01): 294-295 .  百度学术
百度学术
14. 张善婷,冯俊,刘洋. 冠心病患者PCI介入治疗中的护患沟通对治疗依从性的影响. 河北医药. 2021(11): 1743-1746 .  百度学术
百度学术
15. 胥加艳,郭晓鑫. 5E护理在冠心病病人PCI术后康复中的应用研究. 循证护理. 2021(08): 1108-1111 .  百度学术
百度学术
16. 郭秀蝶,郑雅娟,林晨芳,吴群,张亚真. 评判性思维护理对缺铁性贫血伴缺血性心脏病患者贫血及心功能的影响. 心血管病防治知识. 2021(32): 26-29 .  百度学术
百度学术
17. 柯晓玲,吴娟娟. 早期康复护理对老年心血管病患者的效果观察. 心血管病防治知识(学术版). 2020(14): 68-70 .  百度学术
百度学术
18. 孙婧,李萍. 冠心病患者的系统性心肺康复护理. 实用临床医药杂志. 2020(14): 122-125 .  本站查看
本站查看
19. 陈燕华,张苗. 慢性肾脏病合并冠心病患者冠状动脉介入术后行血液透析护理研究. 山西医药杂志. 2020(18): 2548-2549 .  百度学术
百度学术
20. 刘姝娉. 过渡期康复护理措施对老年心血管疾病患者功能恢复及预后的影响. 心血管病防治知识. 2020(24): 70-72 .  百度学术
百度学术
21. 郑燕,常莉,刘桂玲,刘晚霞. 常规护理联合心脏康复护理对冠心病介入治疗后心功能的改善作用. 贵州医药. 2020(10): 1662-1663 .  百度学术
百度学术
22. 张书明. 探讨冠心病冠状动脉介入术患者心脏康复护理模式的建立对促进患者术后恢复的意义. 心血管病防治知识. 2020(31): 58-60 .  百度学术
百度学术
23. 聂志鑫. 时机理论下的家庭护理对经皮冠状动脉性心脏病介入治疗后患者预后和生活质量的影响. 中西医结合护理(中英文). 2020(11): 59-62 .  百度学术
百度学术
其他类型引用(0)




 下载:
下载:
 苏公网安备 32100302010246号
苏公网安备 32100302010246号
