Design of subtalar joint fusion plate and its application
-
摘要:目的
设计一种带有距下关节加压融合功能的新型跟骨接骨板,评价其应用于SandersⅣ型跟骨骨折的临床疗效。
方法使用自行设计的距下关节融合板对50例需要一期融合距下关节的SandersⅣ型跟骨骨折患者进行内固定治疗,观察患者术前、术后和末次随访时的Bolher角、Gissane角以评估跟骨解剖形态,并采用美国足踝外科协会(AOFAS)踝-后足评分评估术后功能。
结果50例患者均顺利完成手术,手术时间37~72 min, 平均(48.04±9.32) min, 术中出血量90~140 mL, 平均(106.00±12.04) mL, 术中均无重要神经、血管损伤; 50例患者均获得随访,随访时间12~21个月,平均(16.36±2.24)个月; 50例患者末次随访时均达到骨性愈合,骨性愈合时间为8~14周,平均(9.52±1.25)周。术后、末次随访时,患者Bolher角、Gissane角均大于术前,差异有统计学意义(P < 0.001); 患者术后Bolher角、Gissane角与末次随访时比较,差异无统计学意义(P=0.372、0.140)。末次随访时,患者平均AOFAS踝-后足评分为(83.78±5.61)分,优9足(90~100分)、良39足(75~ < 90分)、可2足(50~ < 75分),优良率为96.00%; 3例患者术后出现切口皮缘坏死,经过多次换药后切口愈合。
结论距下关节融合板设计合理,可以提供坚强、牢固的固定,术中骨折复位满意,手术操作简单,是治疗需要一期融合距下关节的SandersⅣ型跟骨骨折的理想内固定材料。
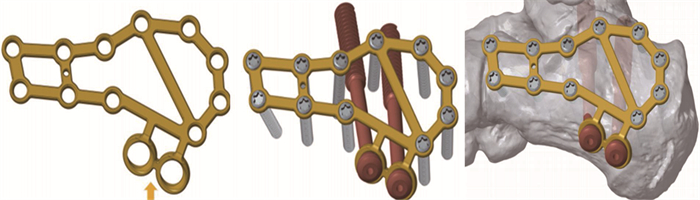
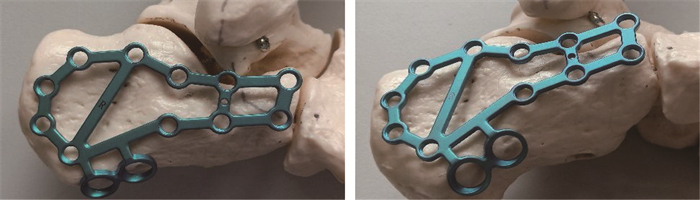
Abstract:ObjectiveTo design a new calcaneal plate with function of subtalar joint compression fusion, and to evaluate its clinical effect for Sanders type Ⅳ calcaneal fracture.
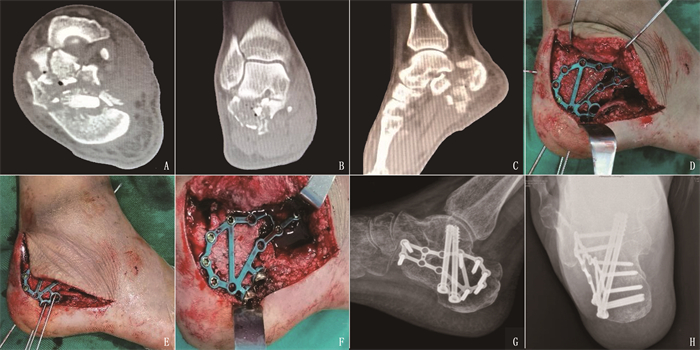
MethodsA total of 50 cases with Sanders type Ⅳ calcaneal fracture requiring primary subtalar joint fusion were treated with internal fixation using a self-designed subtalar joint fusion plate. The anatomical morphology of the calcaneus was evaluated by observing Bolher Angle and Gissane Angle before operation, after operation and at the last follow-up, and the postoperative function was evaluated by the American Association of Foot and Ankle Surgery (AOFAS) ankle-posterior foot score.
ResultsAll 50 patients completed operations successfully, the operation time was from 37 to 72 min, with an average of (48.04±9.32) min, intraoperative bleeding volume was from 90 to 140 mL, with an average of (106.00±12.04) mL. There was no significant nerve and vascular injury during operation. All 50 patients were followed up, with follow-up time of 12 to 21 months and an average of (16.36±2.24) months. Bone healing was achieved at the last follow-up in all 50 patients, and the healing time was 8 to 14 weeks, with an average of (9.52±1.25) weeks. The postoperative and final follow-up Bolher angles were significantly larger compared with that before surgery (P < 0.001), while there were no statistically significant differences in Bolher angle and Gissane angle between postoperative and final follow-up (P=0.372, 0.140). AOFAS score at the last follow-up was (83.78±5.61), including 9 feet with excellent rating (score of 90 to 100), 39 feet with fine rating (score of 75 to less than 90), and 2 feet with good rating(score of 50 to less than 75), with an excellent and good rate of 96.00%. Postoperative skin edge necrosis occurred in 3 patients, and wound healed after multiple dressing changes.
ConclusionThe subtalar joint fusion plate is reasonable in designand can provide ]strong and firm fixation, with satisfactory intraoperative fracture reductionand simple operation. It is an ideal internal fixation material for Sanders type Ⅳ calcaneal fracture requiring primary subtalar joint fusion.
-
Keywords:
- calcaneal fracture /
- subtalar joint /
- joint fusion /
- innovative type /
- calcaneal locking plate
-
-
表 1 150例患者不同时点影像学指标比较(x±s)
° 指标 术前 术后 末次随访 Bolher角 12.57±2.24 31.99±4.19* 32.17±3.54*** Gissane角 88.46±6.46 129.49±5.92* 129.85±5.44*** 与术前比较, * * * P < 0.001。 -
[1] BENIRSCHKE S K, KRAMER P A. Joint-preserving osteotomies for malaligned intraarticular calcaneal fractures[J]. Foot Ankle Clin, 2016, 21(1): 111-122. doi: 10.1016/j.fcl.2015.09.013
[2] OUYANG H B, DENG Y P, XIE P S, et al. Biomechanical comparison of conventional and optimised locking plates for the fixation of intraarticular calcaneal fractures: a finite element analysis[J]. Comput Methods Biomech Biomed Engin, 2017, 20(12): 1339-1349. doi: 10.1080/10255842.2017.1361938
[3] ALMEIDA J F, VALE C, GONZALEZ T, et al. Osteosynthesis or primary arthrodesis for displaced intra-articular calcaneus fractures Sanders type IV-A systematic review[J]. Foot Ankle Surg, 2021: Published online ahead of print.
[4] ROUKIS T S. Joint-sparing surgical management of sanders IV displaced intra-articular calcaneal fractures[J]. Clin Podiatr Med Surg, 2019, 36(2): 251-268. doi: 10.1016/j.cpm.2018.10.007
[5] HOLM J L, LAXSON S E, SCHUBERTH J M. Primary subtalar joint arthrodesis for comminuted fractures of the calcaneus[J]. J Foot Ankle Surg, 2015, 54(1): 61-65. doi: 10.1053/j.jfas.2014.07.013
[6] 程千, 赵建忠, 狄东华, 等. 改良切口与传统L形切口治疗跟骨骨折的临床疗效对比[J]. 实用医学杂志, 2016, 32(14): 2374-2376. doi: 10.3969/j.issn.1006-5725.2016.14.036 [7] BLÄSIUS F M, LINK B C, BEERES F J P, et al. Impact of surgical procedures on soft tissue microcirculation in calcaneal fractures: a prospective longitudinal cohort study[J]. Injury, 2019, 50(12): 2332-2338. doi: 10.1016/j.injury.2019.10.004
[8] KAPIL MANI K C, ACHARYA P, DIRGHA RAJ R C, et al. A modified minimally invasive technique for intra-articular displaced calcaneal fractures fixed by transverse and axial screws[J]. Eur J Orthop Surg Traumatol, 2017, 27(7): 997-1004. doi: 10.1007/s00590-017-1969-x
[9] LIU G T, VANPELT M D, LALLI T, et al. Surgical management of displaced intra-articular calcaneal fractures[J]. Clin Podiatric Med Surg, 2019, 36(2): 173-184. doi: 10.1016/j.cpm.2018.10.002
[10] 吴廷江. 跗骨窦"八"字形切口入路钢板内固定手术治疗SandersⅡ、Ⅲ型跟骨骨折的效果[J]. 实用临床医药杂志, 2020, 24(13): 47-50. https://www.cnki.com.cn/Article/CJFDTOTAL-XYZL202013015.htm [11] 熊雁, 王子明. 跟骨骨折的临床治疗进展[J]. 创伤外科杂志, 2020, 22(4): 241-244. doi: 10.3969/j.issn.1009-4237.2020.04.001 [12] 梁先勇, 陈志伟. 移位型跟骨关节内骨折的手术治疗进展[J]. 中国骨与关节杂志, 2016, 5(4): 279-283. doi: 10.3969/j.issn.2095-252X.2016.04.009 [13] KUMAR S, KRISHNA L G, SINGH D, et al. Evaluation of functional outcome and complications of locking calcaneum plate for fracture calcaneum[J]. J Clin Orthop Trauma, 2015, 6(3): 147-152. doi: 10.1016/j.jcot.2015.05.006
[14] LIN J T, XIE C L, CHEN K, et al. Comparison of sinus tarsi approach versus extensile lateral approach for displaced intra-articular calcaneal fractures Sanders type IV[J]. Int Orthop, 2019, 43(9): 2141-2149. doi: 10.1007/s00264-019-04318-w
[15] GUSIC N, FEDEL I, DARABOS N, et al. Operative treatment of intraarticular calcaneal fractures: anatomical and functional outcome of three different operative techniques[J]. Injury, 2015, 46(Suppl 6): S130-S133.
[16] BUCKLEY R, LEIGHTON R, SANDERS D, et al. Open reduction and internal fixation compared with ORIF and primary subtalar arthrodesis for treatment of Sanders type IV calcaneal fractures: a randomized multicenter trial[J]. J Orthop Trauma, 2014, 28(10): 577-583. doi: 10.1097/BOT.0000000000000191
[17] GAJDOŠÍKOVÁ K, VESELY R, SUCHOMEL R, et al. Correction loss of calcaneal fractures by different type of osteosynthesis[J]. Acta ChirOrthopTraumatol Cech, 2019, 86(2): 124-130.
[18] CSIZY M, BUCKLEY R, TOUGH S, et al. Displaced intra-articular calcaneal fractures: variables predicting late subtalar fusion[J]. J Orthop Trauma, 2003, 17(2): 106-112. doi: 10.1097/00005131-200302000-00005
[19] SCHEPERS T. The primary arthrodesis for severely comminuted intra-articular fractures of the calcaneus: a systematic review[J]. Foot Ankle Surg, 2012, 18(2): 84-88. doi: 10.1016/j.fas.2011.04.004
[20] CHU C H, CHEN Y Y, LIN K P, et al. Anatomic locking plate for displaced intraarticular calcaneal fracture: design and application[J]. J Foot Ankle Surg, 2017, 56(6): 1165-1169. doi: 10.1053/j.jfas.2017.05.030
[21] CHEN K W, ZHANG H T, WANG G L, et al. Comparison of nonlocking plates and locking plates for intraarticular calcaneal fracture[J]. Foot Ankle Int, 2014, 35(12): 1298-1302. doi: 10.1177/1071100714547520
[22] RAK V, IRA D, MASEK M. Operative treatment of intra-articular calcaneal fractures with calcaneal plates and its complications[J]. Indian J Orthop, 2009, 43(3): 271-280. doi: 10.4103/0019-5413.49388
[23] 杨佳林, 张玉堂, 付炳金, 等. 3D打印技术辅助治疗SandersⅡ、Ⅲ型跟骨骨折的疗效观察[J]. 实用临床医药杂志, 2020, 24(13): 29-32. https://www.cnki.com.cn/Article/CJFDTOTAL-XYZL202013009.htm [24] 何平, 尹国栋, 罗剑, 等. 小切口撬拨复位克氏针内固定术与切开复位钢板内固定术治疗SandersⅡ、Ⅲ型跟骨骨折的疗效对比[J]. 实用医学杂志, 2020, 36(15): 2088-2093. https://www.cnki.com.cn/Article/CJFDTOTAL-SYYZ202015014.htm [25] 徐杨博, 魏代清, 邓勇, 等. 切开复位内固定加一期距下关节融合术治疗严重粉碎Sanders Ⅳ型跟骨骨折[J]. 中华创伤骨科杂志, 2017, 19(12): 1046-1051. doi: 10.3760/cma.j.issn.1671-7600.2017.12.007 [26] 焦振清, 刘玉昌, 彭阿钦. 距下关节融合钢板内固定治疗Sanders Ⅳ型跟骨骨折[J]. 中国矫形外科杂志, 2005, 13(4): 261-263. https://www.cnki.com.cn/Article/CJFDTOTAL-ZJXS200504007.htm




 下载:
下载:
 苏公网安备 32100302010246号
苏公网安备 32100302010246号
