Establishment of a prediction model of lymph node metastasis in patients with non-small cell lung cancer at high altitude areas based on energy spectrum CT parameters and clinicopathological factors
-
摘要:目的
探讨高海拔地区非小细胞肺癌(NSCLC)患者的淋巴结转移的能谱CT参数、临床病理因素、影响因素及其预测模型的应用效能。
方法选取青海省人民医院2020年1月—2021年7月收治的84例NSCLC患者作为研究对象,其中50例患者进行能谱CT检测并收集临床资料。依据淋巴结转移病理检查结果将50例患者分为转移组、未转移组,采用单因素分析2组患者的临床病理因素、能谱CT参数差异,采用多因素回归分析NSCLC患者发生淋巴结转移的影响因素并建立预测模型。应用预测模型分析其他34例NSCLC患者的淋巴结转移情况,以临床检测结果为金标准,评估预测模型的应用价值。
结果① 50例患者的淋巴结转移发生率为30.00%。转移组患者的术前癌胚抗原(CEA)、中央型隆突位置比率、淋巴结直径高于未转移组,差异有统计学意义(P < 0.05)。②转移组患者的淋巴结能谱曲线斜率(λHu)、标准化碘密度值(NIC)、淋巴结与原发病灶的λHu比值均低于未转移组,差异有统计学意义(P < 0.05)。③ NSCLC患者发生淋巴结转移的危险因素为淋巴结与原发病灶的λHu比值、术前CEA≥5 ng/mL、淋巴结直径≥3 cm。④ NSCLC患者淋巴结转移的预测模型诊断34例NSCLC患者的准确度、特异度、敏感度均在80.00%以上。
结论NSCLC患者淋巴结转移中可应用能谱CT参数以及临床病理因素中的相关危险因素建立预测模型进行准确预测,该模型可作为预测淋巴结转移的首选工具。
Abstract:ObjectiveTo explore the energy spectrum CT parameters, clinicopathological factors, influencing factors and the application efficiency of the prediction model of lymph node metastasis in patients with non-small cell lung cancer (NSCLC) at high altitude area.
MethodsA total of 84 NSCLC patients from January 2020 to July 2021 in Qinghai Provincial People′s Hospital were selected as research objects, of whom 50 patients were conducted with energy spectrum CT detection and their clinical materials were collected. According to the pathological examination results of lymph node metastasis, 50 patients were divided into metastasis group and non-metastasis group, the differences of clinicopathological factors and energy spectrum CT parameters between the two groups were analyzed by univariate analysis, the influencing factors of lymph node metastasis in NSCLC patients were analyzed by multivariate regression analysis, and a prediction model was established. The prediction model was used to analyze the lymph node metastasis of the other 34 NSCLC patients, and the clinical test results were used as the gold standard to evaluate the application value of the prediction model.
Results① The incidence of lymph node metastasis in 50 patients was 30.00%. The preoperative carcinoembryonic antigen (CEA), ratio of central carina position and lymph node diameter in the metastasis group were significantly higher than those in the non-metastasis group (P < 0.05). ② Slope of energy spectrum curve of lymph nodes (λHu), normalized iodine concentration (NIC) and λHu ratio of lymph nodes to primary lesions in the metastasis group were significantly lower than those in the non-metastasis group (P < 0.05). ③ The risk factors of lymph node metastasis in NSCLC patients were the λHu ratio of lymph nodes to primary lesions, preoperative CEA≥5 ng/mL and lymph node diameter≥3 cm. ④ The accuracy, specificity and sensitivity of the prediction model for lymph node metastasis in 34 patients with NSCLC were all above 80.00%.
ConclusionIn the NSCLC patients with lymph node metastasis, energy spectrum CT parameters and related risk factors in clinicopathological factors can be used to establish a prediction model for accurate prediction, and this model can be used as the preferred tool to predict lymph node metastasis.
-
肺癌最常见的类型是非小细胞肺癌(NSCLC), 其具有细胞增殖缓慢、晚期转移率高、死亡率高等特点[1-3]。目前, NSCLC的治疗包括手术治疗、化疗和免疫治疗,而大多数NSCLC患者在发病前期不会有明显的症状表现,确诊时多为晚期,且伴有血行转移或淋巴结转移,而淋巴结转移会直接影响手术治疗的效果[4]。本研究分析NSCLC患者淋巴结转移的影响因素,根据影响因素建立预测模型,并进一步验证模型的临床预测价值,现将结果报告如下。
1. 资料与方法
1.1 一般资料
选取青海省人民医院2020年1月—2021年7月收治的NSCLC患者84例作为研究对象,年龄50~70岁,平均(64.45±2.32)岁,男38例,女46例,肿瘤位于左侧肺39例,右侧肺45例,有吸烟史者40例。选取其中50例患者进行能谱CT检查并收集临床资料,依据淋巴结转移病理检查结果分为转移组和未转移组。其余34例患者作为预测模型的验证研究对象。纳入标准: ①经病理学检查结果证实为NSCLC者[5]; ②临床资料完整者; ③能谱CT成像的能谱曲线参数偏差较小者; ④预期存活时间超过3个月者。排除标准: ①已接受舒尼替尼、多西紫杉醇、顺铂等放化疗治疗者; ②近1个月内服用其他抗炎抑制药物、抗癌药物者; ③合并肺结核、肺间质纤维化、肺源性心脏病以及其他恶性肿瘤者; ④精神疾病史或者有沟通障碍者。
1.2 方法
1.2.1 能谱CT成像检查
胸部CT增强扫描采用的设备为GE Revolution CT(美国GE公司生产),扫描范围为胸廓入口至肾上腺,由专业医务人员在扫描前进行呼吸训练指导,嘱咐患者在扫描时保持深吸气末屏气状态。利用高压注射器经肘静脉注射320 mg/mL低渗非离子型对比剂,注射速率为3.0 mL/s。延迟时间为0.5 s, 准直器宽度、层间距、扫描视野分别为40 mm、5 mm、32 cm, 双源切换数据为80~120 kVp, 将采集的原始数据依据单能重建算法重建图像后传入GE AW4.6r软件进行图像处理。
1.2.2 癌胚抗原(CEA)检测
采集50例研究对象的2 mL空腹静脉血,参照3 000转/min、20 cm离心半径的条件进行离心,持续10 min后收集血清,采用SIEMENS XP化学发光免疫分析仪测定CEA。
1.3 观察指标
① 记录50例患者的淋巴结转移发生情况并进行分组,收集并比较2组患者的临床病理资料,包括年龄、性别、吸烟史、隆突位置、术前CEA、淋巴结直径。②比较2组患者的能谱CT参数差异,包括动静脉期碘密度值(IC)、水密度值(WC), 计算淋巴结、原发病灶的能谱曲线斜率(λHu)及两者的λHu比值,记录标准化碘密度值(NIC)、标准化水密度值(NWC)、标化有效原子序数(Neff-Z)。③采用多因素分析NSCLC患者发生淋巴结转移的影响因素。④依据影响因素建立NSCLC患者淋巴结预测模型,以后续纳入的34例NSCLC患者的淋巴结转移情况进行验证研究,评估预测模型的特异度、敏感度、准确度。
1.4 统计学方法
采用SPSS 22.0软件进行数据处理,计量资料行正态性和方差齐性检验,满足正态分布时采用(x±s)表示,组间比较行t检验,计数资料采用[n(%)]表示,组间比较行χ2检验,采用多因素Logistic回归法分析NSCLC患者淋巴结转移的影响因素, P < 0.05为差异有统计学意义。
2. 结果
2.1 NSCLC患者淋巴结转移临床特征的单因素分析
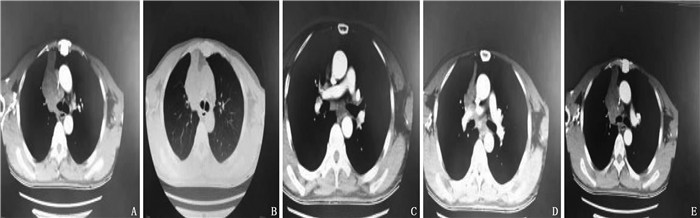
50例NSCLC患者中, 15例患者发生淋巴结转移,发生率为30.00%。转移组与未转移组在术前CEA、距隆突位置、淋巴结直径方面比较,差异均有统计学意义(P < 0.05), 见表 1、图 1。
表 1 NSCLC患者淋巴结转移临床特征的单因素分析[n(%)]临床特征 分类 转移组(n=15) 未转移组(n=35) χ2 P 年龄 < 60岁 6(40.00) 16(45.71) 0.139 0.709 ≥60岁 9(60.00) 19(54.29) 性别 男 5(33.33) 16(45.71) 0.661 0.416 女 10(66.67) 19(54.29) 术前癌胚抗原 < 5 ng/mL 3(20.00) 24(68.57) 9.972 0.002 ≥5 ng/mL 12(80.00) 11(31.43) 淋巴结直径 < 3 cm 4(26.67) 22(62.86) 5.510 0.019 ≥3 cm 11(73.33) 13(37.14) 距隆突位置 中央型 10(66.67) 10(28.57) 6.349 0.012 周围型 5(33.33) 25(71.43) 吸烟史 是 7(46.67) 16(45.71) 0.004 0.951 否 8(53.33) 19(54.29) 2.2 转移组与未转移组NSCLC患者的能谱CT参数比较
转移组患者的淋巴结λHu、淋巴结与原发病灶λHu比值、NIC均低于未转移组患者,差异均有统计学意义(P < 0.05); 转移组与未转移组患者的原发病灶λHu、Neff-Z、IC、WC、NWC比较,差异无统计学意义(P>0.05)。见表 2。
表 2 转移组与未转移组能谱CT参数比较(x±s)参数 转移组(n=15) 未转移组(n=35) 淋巴结λHu 1.82±0.57* 2.22±0.27 原发病灶λHu 1.71±0.47 1.67±0.43 淋巴结与原发病灶的λHu比值 1.02±0.22* 1.32±0.49 Neff-Z 0.79±0.02 0.78±0.02 IC 17.82±3.23 17.22±3.27 WC 1.00±0.01 1.00±0.02 NIC 0.22±0.02* 0.72±0.09 NWC 1.02±0.01 1.02±0.02 λHu: 能谱曲线斜率; Neff-Z: 标化有效原子序数; IC: 碘密度值; WC: 水密度值; NIC: 标准化碘密度值; NWC: 标准化水密度值。与未转移组比较, *P < 0.05。 2.3 NSCLC患者淋巴结转移的影响因素的多因素分析
将P < 0.05的变量设为自变量,包括淋巴结λHu、淋巴结与原发病灶的λHu比值、NIC、距隆突位置、术前CEA、淋巴结直径,将NSCLC患者发生淋巴结转移设为因变量,采用多因素回归分析NSCLC患者发生淋巴结转移的影响因素,结果显示,淋巴结与原发病灶的λHu比值、术前CEA≥5 ng/mL、淋巴结直径≥3 cm是NSCLC患者发生淋巴结转移的危险因素(P < 0.05)。见表 3、表 4。上述回归分析结果准确、可靠,回归方程的拟合度R2=0.265, 拟合度显著(F=4.001, P=0.002),提示本回归模型存在显著意义,即自变量中至少有1个可以显著影响,回归方程的残差情况见图 2。
表 3 变量赋值表变量 编号 赋值 隆突位置 X1 1=中央型, 2=周围型 术前CEA X2 1=≥5 ng/mL, 2= < 5 ng/mL 淋巴结直径 X3 1=≥3 cm, 2= < 3 cm 淋巴结λHu X4 — 淋巴结与原发病灶的λHu比值 X5 — NIC X6 — 淋巴结转移 Y 1=是, 2=否 CEA: 癌胚抗原; λHu: 能谱曲线斜率; NIC: 标准化碘密度值。 表 4 多因素分析NSCLC患者淋巴结转移的影响因素变量 非标准化系数 标准错误 标准系数 T P VIF 常数 2.689 0.560 — 4.799 < 0.001 — 术前CEA -0.403 0.115 -0.439 -3.497 0.001 1.055 淋巴结直径 0.337 0.119 -0.367 -2.829 0.007 1.127 距隆突位置 -0.088 0.127 -0.088 -0.688 0.495 1.085 淋巴结与原发病灶的λHu比值 0.463 0.174 -0.419 -2.332 0.004 1.032 淋巴结λHu -0.139 0.166 -0.107 -0.834 0.409 1.105 NIC -0.132 0.161 -0.102 -0.828 0.411 1.102 2.4 NSCLC患者淋巴结转移预测模型的建立与验证
NSCLC患者淋巴结预测模型为: 0.269+0.463×淋巴结与原发病灶的λHu比值+0.337×淋巴结直径-0.403×术前CEA。将用于验证的NSCLC患者的淋巴结转移危险因素带入列线图预测模型,计算其概率值。以50%作为预测概率值的淋巴结转移判定值,预测概率值≥50%认为发生淋巴结转移的可能性高,为高危患者; 预测概率值< 50%认为发生淋巴结转移的可能性低,为低危患者。34例患者中,共有20例发生淋巴结转移, 14例未发生转移, NSCLC淋巴结预测模型检出21例淋巴结转移, 13例未转移,检测准确度为85.29%, 敏感度为85.71%, 特异度为84.62%。
3. 讨论
2020年中国临床肿瘤学会(CSCO)《非小细胞肺癌诊疗指南(第8版)》明确提出了对于不同病理类型、分期和分子分型(包括不同驱动基因)的NSCLC, 临床治疗应采取不同的方案,其中纵隔淋巴结转移是影响NSCLC手术效果、预后的关键因素,针对N0~1期及N2~3的NSCLC患者应采用不同的治疗方案[6]。术前准确预测NSCLC纵隔淋巴结转移是制订科学、合理的治疗方案的关键[7]。作者在既往临床工作中发现患者胸部CT检查提示肺门及纵隔淋巴结多数肿大,临床多考虑转移,而术后病理证实多数为炎性反应增生淋巴结,术前预测纵隔淋巴结转移会直接影响到临床个体化综合治疗的效果,更为手术介入的时机提供依据,因此需要建立预测纵隔淋巴结转移的模型,以便提高预测的准确性。
碘是能谱CT成像所用对比剂中的主要成分,因此碘密度可反映肿瘤及淋巴结供血情况[8]。本研究结果显示,淋巴结转移NSCLC患者病灶中的淋巴结λHu、淋巴结与原发病灶的λHu比值以及NIC值均显著低于淋巴结未转移的患者,淋巴结与原发病灶的λHu比值是NSCLC患者发生淋巴结转移的危险因素,提示转移病灶与原发病灶存在一定的同源性, λHu值、NIC可有效反映转移淋巴结与原发病灶的同源性。相较于常规CT, 能谱CT可以避免射线硬化产生的效应问题,保证单能量水平与CT值的精准对应,还可保证随单能量变化获取对应的CT动态变化值,因此可准确检查出NSCLC患者的淋巴结转移情况,而淋巴结和原发病灶λHu比值可以作为预测NSCLC淋巴结转移的敏感指标[9]。
肺癌主要起源于支气管、肺叶支气管,中央型肺癌是指癌组织靠近肺门[10]。本研究结果显示,中央型肺癌较周围性肺癌的淋巴结转移率高,分析其原因可能是距离肺门较近的中央型肺癌对支气管壁以及周围正常肺部组织的侵袭程度更严重,另外由胸内肺门向纵隔淋巴结引流是肺癌胸内淋巴结转移的主要途径,因此NSCLC患者更容易发生淋巴结转移,该类患者更倾向于选择系统性淋巴结清扫,可以保证较为准确的淋巴结分期[11]。本研究转移组、未转移组患者的术前CEA水平存在显著差异,转移组患者的CEA水平更高,并且CEA是NSCLC患者淋巴结转移模型以及危险因素中的一项,与既往研究[12]基本相符,提示术前CEA在NSCLC患者淋巴结转移中具有较高的敏感性以及预测价值。产生上述结果的原因是CEA为临床常用的肿瘤敏感标志物,内胚层细胞分化的癌细胞表面是主要分布位置,形成于细胞浆,经细胞膜传递分泌于细胞外以及周围体液中,在血清、胃液等体液中均可检出,随着患者病情的加重, CEA水平会相应增加[13]。
本研究中,未转移组患者淋巴结直径显著小于转移组患者,并且纳入了预测NSCLC患者发生淋巴结转移的模型中,提示大直径淋巴结患者的转移风险更高。龚麒麟等[14]研究发现,淋巴结直径越小,其淋巴结转移的风险越低,与本研究结果相符,分析其原因可能是直径>1 cm的淋巴结为危险淋巴结,在一定程度上增加了患者淋巴结再转移的风险,而大直径的淋巴结提示肿瘤患者的肺内脉管侵及组织加重,进而增高患者侵袭脉管组织出现淋巴结转移的风险。本研究应用NSCLC患者淋巴结转移预测模型检测34例NSCLC患者淋巴结转移的准确度、敏感度、特异度均超过80.00%, 结合以上单因素、多因素结果分析均可说明应用NSCLC患者淋巴结影响因素制订的预测模型可准确、有效预测NSCLC患者的淋巴结转移情况,具备较高的预测价值。
本研究存在的局限性为受到图像储存和质量因素的影响而导致研究样本量相对较少,并且样本数据来源于单中心医疗机构,可能会增加数据偏倚发生风险。总之, NSCLC患者淋巴结转移中可应用能谱CT参数以及临床病理因素中的相关危险因素建立预测模型进行准确预测,该模型可作为预测淋巴结转移的首选工具。
-
表 1 NSCLC患者淋巴结转移临床特征的单因素分析[n(%)]
临床特征 分类 转移组(n=15) 未转移组(n=35) χ2 P 年龄 < 60岁 6(40.00) 16(45.71) 0.139 0.709 ≥60岁 9(60.00) 19(54.29) 性别 男 5(33.33) 16(45.71) 0.661 0.416 女 10(66.67) 19(54.29) 术前癌胚抗原 < 5 ng/mL 3(20.00) 24(68.57) 9.972 0.002 ≥5 ng/mL 12(80.00) 11(31.43) 淋巴结直径 < 3 cm 4(26.67) 22(62.86) 5.510 0.019 ≥3 cm 11(73.33) 13(37.14) 距隆突位置 中央型 10(66.67) 10(28.57) 6.349 0.012 周围型 5(33.33) 25(71.43) 吸烟史 是 7(46.67) 16(45.71) 0.004 0.951 否 8(53.33) 19(54.29) 表 2 转移组与未转移组能谱CT参数比较(x±s)
参数 转移组(n=15) 未转移组(n=35) 淋巴结λHu 1.82±0.57* 2.22±0.27 原发病灶λHu 1.71±0.47 1.67±0.43 淋巴结与原发病灶的λHu比值 1.02±0.22* 1.32±0.49 Neff-Z 0.79±0.02 0.78±0.02 IC 17.82±3.23 17.22±3.27 WC 1.00±0.01 1.00±0.02 NIC 0.22±0.02* 0.72±0.09 NWC 1.02±0.01 1.02±0.02 λHu: 能谱曲线斜率; Neff-Z: 标化有效原子序数; IC: 碘密度值; WC: 水密度值; NIC: 标准化碘密度值; NWC: 标准化水密度值。与未转移组比较, *P < 0.05。 表 3 变量赋值表
变量 编号 赋值 隆突位置 X1 1=中央型, 2=周围型 术前CEA X2 1=≥5 ng/mL, 2= < 5 ng/mL 淋巴结直径 X3 1=≥3 cm, 2= < 3 cm 淋巴结λHu X4 — 淋巴结与原发病灶的λHu比值 X5 — NIC X6 — 淋巴结转移 Y 1=是, 2=否 CEA: 癌胚抗原; λHu: 能谱曲线斜率; NIC: 标准化碘密度值。 表 4 多因素分析NSCLC患者淋巴结转移的影响因素
变量 非标准化系数 标准错误 标准系数 T P VIF 常数 2.689 0.560 — 4.799 < 0.001 — 术前CEA -0.403 0.115 -0.439 -3.497 0.001 1.055 淋巴结直径 0.337 0.119 -0.367 -2.829 0.007 1.127 距隆突位置 -0.088 0.127 -0.088 -0.688 0.495 1.085 淋巴结与原发病灶的λHu比值 0.463 0.174 -0.419 -2.332 0.004 1.032 淋巴结λHu -0.139 0.166 -0.107 -0.834 0.409 1.105 NIC -0.132 0.161 -0.102 -0.828 0.411 1.102 -
[1] CARBONE D P, RECK M, PAZ-ARES L, et al. First-line nivolumab in stage IV or recurrent non-small-cell lung cancer[J]. N Engl J Med, 2017, 376(25): 2415-2426. doi: 10.1056/NEJMoa1613493
[2] ETTINGER D S, WOOD D E, AISNER D L, et al. Non-small cell lung cancer, version 5. 2017, NCCN clinical practice guidelines in oncology[J]. J Natl Compr Canc Netw, 2017, 15(4): 504-535. doi: 10.6004/jnccn.2017.0050
[3] 张娇, 赖远阳, 孙盈, 等. 非小细胞肺癌淋巴结转移与临床病理特征及预后的关系[J]. 现代肿瘤医学, 2019, 27(18): 3238-3241. doi: 10.3969/j.issn.1672-4992.2019.18.017 [4] SORIA J C, TAN D S W, CHIARI R, et al. First-line ceritinib versus platinum-based chemotherapy in advanced ALK-rearranged non-small-cell lung cancer (ASCEND-4): a randomised, open-label, phase 3 study[J]. Lancet, 2017, 389(10072): 917-929. doi: 10.1016/S0140-6736(17)30123-X
[5] POSTMUS P E, KERR K M, OUDKERK M, et al. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up[J]. Ann Oncol, 2017, 28(suppl_4): iv1-iv21.
[6] FENNELL D A, SUMMERS Y, CADRANEL J, et al. Cisplatin in the modern era: the backbone of first-line chemotherapy for non-small cell lung cancer[J]. Cancer Treat Rev, 2016, 44: 42-50. doi: 10.1016/j.ctrv.2016.01.003
[7] KATAKAMI N, UCHINO J, YOKOYAMA T, et al. Anamorelin (ONO-7643) for the treatment of patients with non-small cell lung cancer and Cachexia: results from a randomized, double-blind, placebo-controlled, multicenter study of Japanese patients (ONO-7643-04)[J]. Cancer, 2018, 124(3): 606-616. doi: 10.1002/cncr.31128
[8] LI A, WEI Z J, DING H, et al. Docetaxel versus docetaxel plus cisplatin for non-small-cell lung cancer: a meta-analysis of randomized clinical trials[J]. Oncotarget, 2017, 8(34): 57365-57378. doi: 10.18632/oncotarget.17071
[9] 陈盈, 姚琼瑛, 郑昊, 等. 能谱CT在肺癌淋巴结转移诊断中的临床应用研究[J]. 肿瘤学杂志, 2016, 22(8): 632-638. https://www.cnki.com.cn/Article/CJFDTOTAL-XHON201608005.htm [10] 李伟婷, 李永文, 张洪兵, 等. 基于TCGA数据库的中央型与周围型肺鳞癌基因表达差异性研究[J]. 中国肺癌杂志, 2019, 22(5): 280-288. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ201905005.htm [11] 申磊磊, 云天洋, 郭俊唐, 等. 左侧非小细胞肺癌4L组淋巴结转移的临床病理学特征及危险因素分析[J]. 南方医科大学学报, 2020, 40(12): 1793-1798. doi: 10.12122/j.issn.1673-4254.2020.12.14 [12] 李季, 沈艳, 姜研. CT仿真结肠镜联合肿瘤标志物检测在结直肠癌中的诊断价值[J]. 医学综述, 2021, 27(5): 1032-1036. doi: 10.3969/j.issn.1006-2084.2021.05.037 [13] 钱香, 王宏, 任真, 等. NLR与FIB和CEA及CA19-9在结直肠癌中的应用价值[J]. 中华预防医学杂志, 2021, 55(4): 499-505. doi: 10.3760/cma.j.cn112150-20200805-01094 [14] 龚麒麟, 边聪, 刘辉. 早期舌鳞状细胞癌颈隐匿性淋巴结转移的回顾性分析[J]. 中华耳鼻咽喉头颈外科杂志, 2016, 51(10): 773-775. doi: 10.3760/cma.j.issn.1673-0860.2016.10.012 -
期刊类型引用(5)
1. 李雅倩,刘义,刘百娜. 能谱CT定量参数联合MSCT三维重建在肺癌患者术前淋巴结转移评估中的应用价值. 实用癌症杂志. 2025(03): 479-483 .  百度学术
百度学术
2. 曾海燕,杨小林. CT能谱参数对结直肠癌病理类型鉴别的价值. 中外医学研究. 2024(09): 64-67 .  百度学术
百度学术
3. 王海波,段宏伟,左自军,丁琦峰,张鹏辉. 术前能谱CT多参数成像对晚期肺癌患者淋巴结转移的预测价值. 河南医学研究. 2024(06): 1071-1074 .  百度学术
百度学术
4. 刘贲,张楠,邓治平. miR-126及Th1相关细胞因子在非小细胞肺癌患者血清中的表达水平及临床意义. 热带医学杂志. 2024(08): 1154-1158 .  百度学术
百度学术
5. 周宇元. 增强CT联合能谱CT预测肺癌患者淋巴结转移的临床分析. 江西医药. 2024(07): 676-679 .  百度学术
百度学术
其他类型引用(0)




 下载:
下载:

 苏公网安备 32100302010246号
苏公网安备 32100302010246号