Effect of EZH2 knockout on podocyte injury and JAK2/STAT3 signaling pathway in mice with focal segmental glomerulosclerosis
-
摘要:目的
探讨EZH2基因敲除对局灶节段性肾小球硬化(FSGS)模型小鼠肾脏足细胞损伤和JAK2/STAT3信号通路的影响。
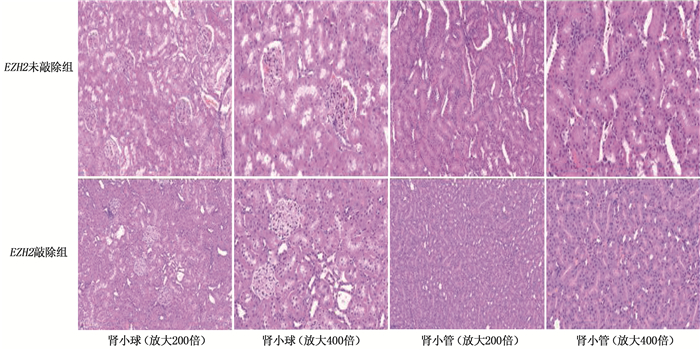
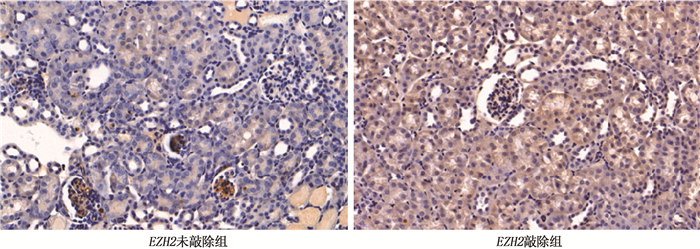
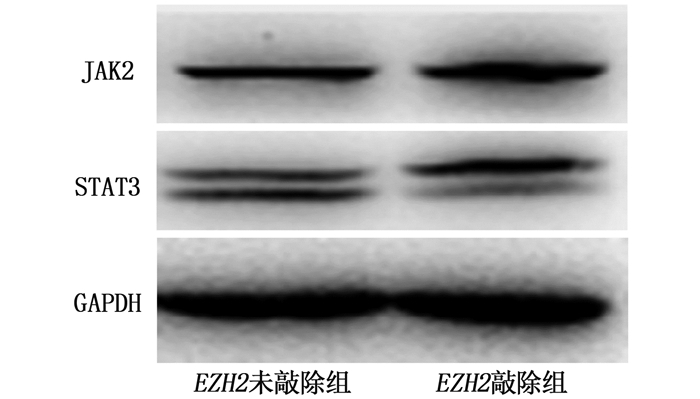
方法将60只Cas9小鼠随机分为EZH2敲除组和EZH2未敲除组,每组30只。EZH2敲除组小鼠肾静脉注射重组腺病毒(AAV9-sgRNA-EZH2),EZH2未敲除组小鼠肾静脉注射磷酸盐缓冲液(PBS),且2组小鼠均单次尾静脉注射阿霉素,分别建立EZH2敲除FSGS模型和EZH2未敲除FSGS模型。采用苏木素-伊红(HE)染色法观察2组小鼠肾组织病理变化;采用双重免疫荧光染色法观察2组小鼠足细胞nephrin、podocin表达情况;采用TUNEL法检测2组小鼠足细胞凋亡指数;采用免疫印迹(Western blot)法检测2组小鼠肾组织JAK2、STAT3蛋白表达水平。
结果与EZH2未敲除组FSGS小鼠相比,EZH2敲除组FSGS小鼠肾小球病变更严重,足突广泛融合,肾小球基底膜明显增厚,系膜基质增多,毛细血管闭塞。与EZH2未敲除组FSGS小鼠相比,EZH2敲除组FSGS小鼠足细胞nephrin、podocin表达减少,差异有统计学意义(P < 0.01)。EZH2敲除组足细胞凋亡指数为(40.94±2.13)%,高于EZH2未敲除组的(21.23±3.30)%,差异有统计学意义(P < 0.01)。EZH2敲除组FSGS小鼠JAK2、STAT3蛋白表达水平依次为(2.67±0.41)、(2.37±0.53),分别高于EZH2未敲除组的(1.72±0.31)、(1.70±0.48),差异有统计学意义(P < 0.01)。
结论EZH2基因敲除可能参与JAK2/STAT3信号通路的激活,并加重FSGS小鼠肾脏足细胞损伤。
-
关键词:
- EZH2基因 /
- 局灶节段性肾小球硬化 /
- JAK2/STAT3信号通路 /
- 足细胞 /
- 基因敲除
Abstract:ObjectiveTo explore effect of EZH2 knockout on podocyte injury and JAK2/STAT3 signaling pathway in mice model with focal segmental glomerulosclerosis(FSGS).
MethodsSixty Cas9 mice were randomly divided into EZH2 knockout group(n=30) and the EZH2 non-knockout group (n=30). Mice in EZH2 knockout group were intravenously injected with recombinant adenovirus (AAV9-sgRNA-EZH2), those in the EZH2 non-knockout group were intravenously injected with phosphate buffered solution (PBS). Mice in the two groups were injected with doxorubicin once through tail vein to establish EZH2 knockout FSGS model and EZH2 non-knockout FSGS model, respectively. The renal tissue pathological changes were observed by hematoxylin and eosin (HE) staining. The nephrin and podocin expressions were observed by double immunofluorescence. Podocyte apoptosis index was detected by TUNEL. The JAK2 and STAT3 protein expressions were detected by western blot method.
ResultsCompared with mice in the EZH2 non-knockout group, the mice had more serious glomerular pathological changes, widely fused foot processes, significantly thickened glomerular basement membrane, increased mesangial matrix and blocked capillaries. Compared with FSGS mice in the EZH2 non-knockout group, the expressions of nephrin and podocin in podocytes of FSGS mice in the EZH2 knockout group were decreased (P < 0.01). The apoptosis index of podocytic cells in the EZH2 knockout group was (40.94±2.13)%, which was higher than (21.23±3.30)% in the EZH2 non-knockout group (P < 0.01). The protein expression levels of JAK2 and STAT3 in the EZH2 knockout group were (2.67±0.41) and (2.37±0.53) respectively, which were higher than (1.72±0.31) and (1.70±0.48) in the EZH2 non-knockout group (P < 0.01).
ConclusionEZH2 gene knockout may be involved in the activation of JAK2/STAT3 signaling pathway and aggravate renal podocyte injury in FSGS mice.
-
-
表 1 2组FSGS小鼠生化指标水平比较(x±s)
指标 EZH2未敲除组(n=30) EZH2敲除组(n=30) 24 h尿蛋白定量/mg 241.87±31.21 386.65±42.30** BUN/(mmol/L) 13.08±3.08 19.54±3.22** Cr/(μmol/L) 73.50±8.96 96.48±9.32** ALT/(U/L) 41.10±3.91 42.59±7.07 AST/(U/L) 38.35±7.30 40.84±5.41 BUN: 尿素氮; Cr: 肌酐; ALT: 丙氨酸氨基转移酶; AST: 天门冬氨酸氨基转移酶。与EZH2未敲除组比较, **P < 0.01。 表 2 2组FSGS小鼠足细胞JAK2、STAT3蛋白表达水平比较(x±s)
指标 EZH2未敲除组(n=30) EZH2敲除组(n=30) JAK2蛋白 1.72±0.31 2.67±0.41** STAT3蛋白 1.70±0.48 2.37±0.53** 与EZH2未敲除组比较, **P < 0.01。 -
[1] HO J, NG K H, ROSEN S, et al. Podocyte-specific loss of functional microRNAs leads to rapid glomerular and tubular injury[J]. J Am Soc Nephrol, 2008, 19(11): 2069-2075.
[2] 王惠, 何方方, 张春. 足细胞损伤机制研究进展[J]. 中国中西医结合肾病杂志, 2008, 9(11): 1018-1021. doi: 10.3969/j.issn.1009-587X.2008.11.030 [3] LIEBISCH M, WOLF G. AGE-induced suppression of EZH2 mediates injury of podocytes by reducing H3K27me3[J]. Am J Nephrol, 2020, 51(9): 676-692. doi: 10.1159/000510140
[4] SUN G D, CUI W P, GUO Q Y, et al. Histone lysine methylation in diabetic nephropathy[J]. J Diabetes Res, 2014, 2014: 654148.
[5] PACE J, PALADUGU P, DAS B, et al. Targeting STAT3 signaling in kidney disease[J]. Am J Physiol Renal Physiol, 2019, 316(6): F1151-F1161. doi: 10.1152/ajprenal.00034.2019
[6] 邹杰锋, 许云鹏, 张燕子, 等. JAK2/STAT3信号通路在局灶节段性肾小球硬化足细胞损伤中的作用及机制[J]. 中华临床医师杂志: 电子版, 2021, 15(9): 683-690. doi: 10.3877/cma.j.issn.1674-0785.2021.09.008 [7] YANG J W, DETTMAR A K, KRONBICHLER A, et al. Recent advances of animal model of focal segmental glomerulosclerosis[J]. Clin Exp Nephrol, 2018, 22(4): 752-763. doi: 10.1007/s10157-018-1552-8
[8] LIU X, CAO W, QI J, et al. Leonurine ameliorates adriamycin-induced podocyte injury via suppression of oxidative stress[J]. Free Radic Res, 2018, 52(9): 952-960.
[9] 林乔轩, 马屹茕, 丁国华. 表观遗传学与糖尿病肾脏病[J]. 中华肾脏病杂志, 2020, 36(1): 58-62. doi: 10.3760/cma.j.issn.1001-7097.2020.01.013 [10] HONG W, ZHANG G, LU H, et al. Epithelial and interstitial Notch1 activity contributes to the myofibroblastic phenotype and fibrosis[J]. Cell Commun Signal, 2019, 17(1): 145. doi: 10.1186/s12964-019-0455-y
[11] MAJUMDER S, THIEME K, BATCHU S N, et al. Shifts in podocyte histone H3K27me3 regulate mouse and human glomerular disease[J]. J Clin Invest, 2018, 128(1): 483-499.
[12] SIDDIQI F S, MAJUMDER S, THAI K, et al. The histone methyltransferase enzyme enhancer of zeste homolog 2 protects against podocyte oxidative stress and renal injury in diabetes[J]. J Am Soc Nephrol, 2016, 27(7): 2021-2034.
[13] ZHANG L, WANG Y, MA J, et al. Exogenous MSCs ameliorate hypoxia/reoxygenation injury in renal tubular epithelial cells through JAK/STAT signaling pathway-mediated regulation of HMGB1[J]. Am J Transl Res, 2017, 9(5): 2412-2420.
[14] 曹宇, 王保兴. JAK/STAT通路在肾脏疾病发病中的作用[J]. 中华临床医师杂志: 电子版, 2017, 11(1): 114-118. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLYD201701024.htm [15] 袁树珍, 隋晓露, 顾凤娟, 等. 组蛋白H3K27me3介导JAK2/STAT3信号通路对足细胞损伤的调控机制[J]. 医学理论与实践, 2021, 34(17): 2929-2933, 2945. https://www.cnki.com.cn/Article/CJFDTOTAL-YXLL202117001.htm -
期刊类型引用(1)
1. 谷胜男,史梦迪,杨阳,刘璐佳,王有鹏. 分消走泄法治疗儿童特应性皮炎机制研究进展. 陕西中医. 2024(05): 715-718 .  百度学术
百度学术
其他类型引用(3)




 下载:
下载:


 苏公网安备 32100302010246号
苏公网安备 32100302010246号