Echocardiography of patients with secondary operation after artificial heart valve replacement
-
摘要:目的
分析人工瓣膜置换术(HVR)后再次手术患者术前、术后超声心动图的变化,探讨超声心动图对HVR术后再次手术患者心功能及再次手术效果的评估价值。
方法选取HVR术后需再次手术的30例患者,根据再次手术原因分为瓣膜异常组16例,术后重度三尖瓣反流(TR)组14例,分别于术前,术后1、2周,以及术后3、6、12个月复查超声心动图,评估右心功能、三尖瓣及TR程度变化。
结果术后6、12个月, 2组左房内径(LAD)、左室内径(LVD)、右心房最大长轴径(RAmla)、右心室径(RVD)、右心室游离壁厚度(RVWT)均小于术前,右心室容积变化分数(RVFAC)高于术前,差异有统计学意义(P < 0.05); 2组术后1周右室心肌功能指数(RIMP)下降,术后3个月开始升高,术后12个月均高于术前,差异有统计学意义(P < 0.05); 2组术后12个月心脏结构及右心功能比较,差异均无统计意义(P>0.05)。术后6、12个月, 2组三尖瓣瓣环舒张期末内径(TVAEDD)、三尖瓣瓣环收缩期末内径(TVAESD)均较术前降低,三尖瓣瓣环收缩期位移(TAPSE)较术前升高,差异有统计学意义(P < 0.05)。2组手术前后TVAEDD、TVAESD、三尖瓣瓣环缩短分数(PSTVA)、TAPSE比较,差异均无统计学意义(P>0.05)。术后12个月, 2组TR程度均较术前改善,差异有统计学意义(P < 0.05)。2组术后1、2周以及术后3、6、12个月TR程度比较,差异均无统计学意义(P>0.05)。
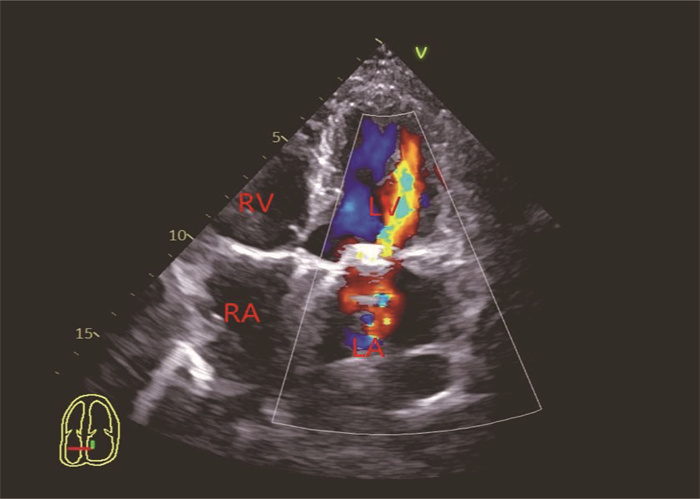
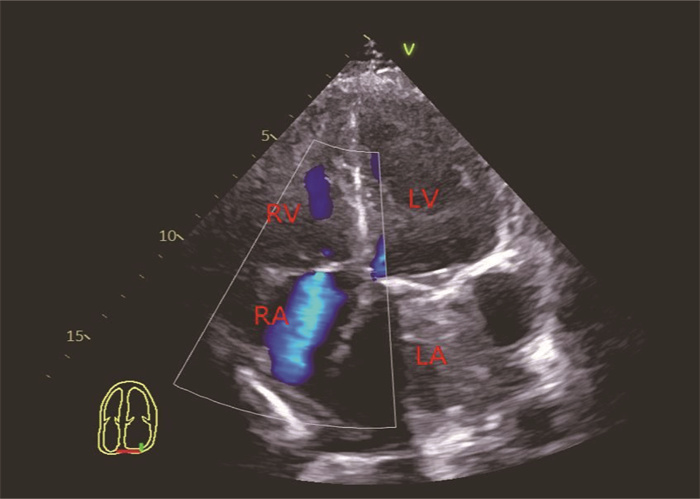
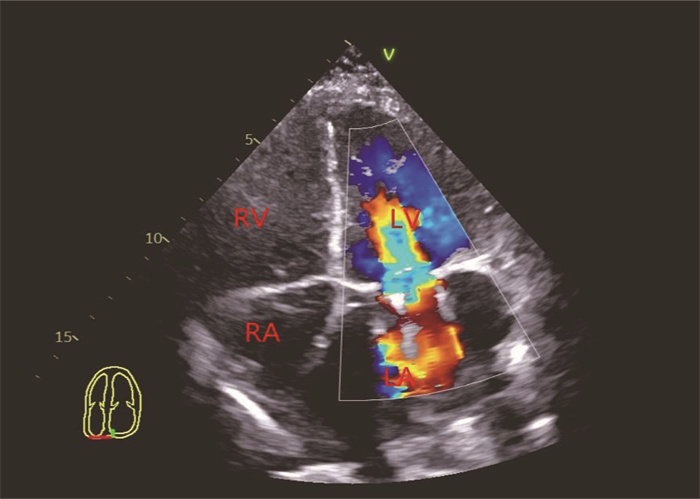
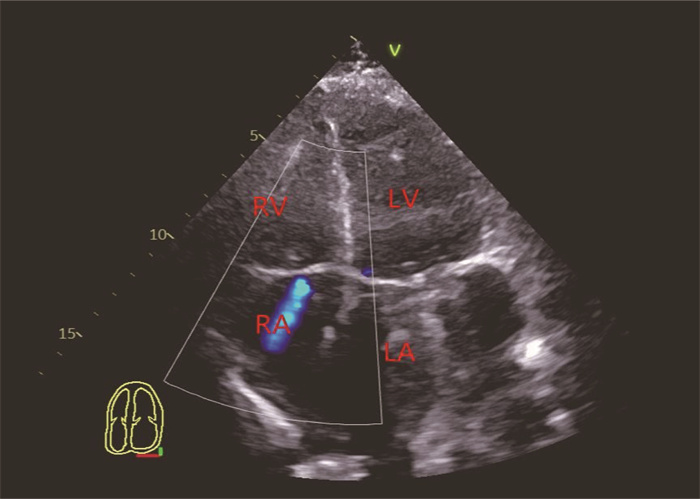
结论超声心动图可通过多个角度观察HVR术后再次手术患者术前、术后的心脏形态结构,全面评估右心功能,评价再次手术的治疗效果,可为临床治疗和预后评估提供参考依据。
Abstract:ObjectiveTo analyze the preoperative and postoperative echocardiographic changes in patients with secondary operation after artificial heart valve replacement (HVR), and to investigate the value of echocardiography in evaluating cardiac function and effect of secondary operation in patients with secondary operation after HVR.
MethodsA total of 30 patients with secondary operation after HVR were selected. According to the reasons of secondary operation, the patients were divided into valve abnormality group (n=16) and severe tricuspid regurgitation after operation group (TR group, n=14). Echocardiography was performed at the time points of before operation, 1 week and 2 weeks after operation, and 3, 6 and 12 months after operation, respectively, and the changes of right heart function, tricuspid valve and TR degree were evaluated.
ResultsAt 6 and 12 months after operation, the left atrial diameter (LAD), left ventricular diameter (LVD), maximum long axis diameter of right atrium (RAmla), right ventricular diameter (RVD) and right ventricular free wall thickness (RVWT) in both groups were lower than those before operation, while the right ventricular fraction area change (RVFAC) was higher than that before operation (P < 0.05); the right ventricular myocardial function index (RIMP) in both groups decreased at 1 week after operation and began to rise at 3 months after operation, and the RIMP at 12 months after operation was higher than that before operation (P < 0.05); there were no significant differences in cardiac structure and right heart function between the two groups at 12 months after operation (P>0.05). At 6 and 12 months after operation, the tricuspid valve annular end diastolic diameter (TVAEDD) and the tricuspid valve annular end systolic diameter (TVAESD) in both groups were lower than those before operation, while the tricuspid annular plane systolic excusion (TAPSE) was higher than that before operation in both groups (P < 0.05). There were no significant differences in TVAEDD, TVAESD, percent shorting of tricuspid valve annulus (PSTVA) and TAPSE before and after operation between the two groups (P>0.05). At 12 months after operation, the degree of TR in both groups was significantly improved (P < 0.05). There were no significant differences in TR between the two groups at 1 week and 2 weeks after operation as well as 3, 6 and 12 months after operation (P>0.05).
ConclusionEchocardiography can be used to observe the preoperative and postoperative cardiac morphology and structure in patients with secondary operation after HVR through multiple viewpoints, comprehensively evaluate the right heart function, access the treatment effect of secondary operation, and provide reference for clinical treatment and prognosis evaluation.
-
-
表 1 2组手术前后心脏结构及右心功能比较(x±s)
组别 指标 术前 术后1周 术后2周 术后3个月 术后6个月 术后12个月 瓣膜异常组(n=16) LAD/mm 56.45±8.64 53.69±9.15 53.43±8.77 49.23±8.48* 47.59±7.81* 44.13±5.77* LVD/mm 54.13±8.53 51.23±7.12 50.98±6.87 49.31±8.61 48.61±4.15* 48.33±4.17* RAmla/mm 49.35±7.78 47.82±7.37 47.41±7.41 46.40±6.81 46.51±5.89 42.36±6.37* RVD/mm 21.84±3.35 21.23±4.27 21.17±4.04 20.37±4.81 21.64±4.41 19.23±2.11* RVFAC/% 35.38±9.36 39.73±9.42 39.87±9.06 42.23±10.54 45.15±8.85* 46.36±7.87* RVWT/mm 4.88±0.84 4.84±0.78 4.64±0.74 4.74±0.71 4.31±0.87* 4.17±0.52* RIMP 0.45±0.12 0.34±0.07* 0.36±0.07* 0.37±0.08* 0.39±0.14 0.47±0.08 TR组(n=14) LAD/mm 54.91±9.15 52.71±8.29 52.47±8.03 46.35±7.57* 44.31±8.57* 43.35±6.41* LVD/mm 54.70±8.91 49.12±6.68 48.87±6.05 47.25±6.27 46.37±4.61* 46.21±5.58* RAmla/mm 51.13±7.48 49.73±6.33 49.41±6.35 47.34±7.64 44.47±8.43* 41.13±5.45* RVD/mm 22.71±3.29 22.62±3.62 22.51±3.17 21.85±4.55 20.45±3.47 20.04±2.64* RVFAC/% 37.17±10.73 43.55±3.75 43.62±3.55 44.85±9.46 46.07±8.81* 47.20±8.51* RVWT/mm 4.65±0.96 4.61±0.82 4.62±0.79 4.57±0.75 4.10±0.51* 3.91±0.61* RIMP 0.41±0.13 0.37±0.08 0.38±0.08 0.39±0.07 0.42±0.11 0.48±0.13* LAD: 左心房径; LVD: 左心室径; RAmla: 右心房最大长轴径; RVD: 右心室径; RVFAC: 右心室面积变化分数; RVWT: 心室游离壁厚度;
RVEF: 右心室射血分数; RIMP: 右室心肌功能指数。与术前比较, *P < 0.05。表 2 2组患者手术前后三尖瓣功能比较(x±s)
组别 指标 术前 术后1周 术后2周 术后3个月 术后6个月 术后12个月 瓣膜异常组(n=16) TVAEDD/mm 32.12±5.34 30.45±4.57 30.12±4.37 29.75±4.36 27.69±5.15* 28.37±3.64* TVAESD/mm 27.87±4.64 25.11±4.65 25.03±4.39 24.85±4.55 22.33±4.17* 23.37±3.77* PSTVA/% 21.79±5.12 22.14±4.71 22.31±4.61 22.85±4.55 23.12±3.87 22.26±3.36 TAPSE/mm 11.76±2.66 11.14±2.28 11.24±2.37 12.45±2.51 13.02±2.87* 14.72±3.11* TR组(n=14) TVAEDD/mm 34.75±6.85 33.91±4.77 33.62±4.48 32.37±4.88 30.71±5.26* 29.33±4.14* TVAESD/mm 28.64±5.12 26.23±4.38 26.02±4.12 25.37±4.81 24.81±5.65* 25.14±4.84* PSTVA/% 20.84±5.04 21.65±5.12 21.82±5.27 22.37±4.81 22.80±3.51 21.14±3.38 TAPSE/mm 11.14±2.51 10.95±2.46 11.03±2.52 11.37±2.81 12.50±2.18* 14.35±3.06* TVAEDD: 三尖瓣瓣环舒张期末内径; TVAESD: 三尖瓣瓣环收缩期末内径; PSTVA: 三尖瓣环缩短分数; TAPSE: 三尖瓣瓣环收缩期位移。
与术前比较, *P < 0.05。表 3 2组患者手术前后TR程度比较
例 组别 TR程度 术前 术后1周 术后2周 术后3个月 术后6个月 术后12个月 瓣膜异常组(n=16) 0 0 11 11 12 13 13 1 1 3 3 4 2 3 2 5 2 2 0 1 0 3 7 0 0 0 0 0 4 3 0 0 0 0 0 5 0 0 0 0 0 0 TR组(n=14) 0 0 8 9 10 11 10 1 0 3 3 3 1 1 2 0 2 2 1 2 3 3 0 1 1 0 0 0 4 9 0 0 0 0 0 5 5 0 0 0 0 0 TR: 三尖瓣反流。 -
[1] RAO N R, TREISTER N, AXTELL A, et al. Preoperative dental screening prior to cardiac valve surgery and 90-day postoperative mortality[J]. J Card Surg, 2020, 35(11): 2995-3003. doi: 10.1111/jocs.14957
[2] CHEN J M, HU K, MA W R, et al. Isolated reoperation for tricuspid regurgitation after left-sided valve surgery: technique evolution[J]. Eur J Cardiothorac Surg, 2020, 57(1): 142-150. doi: 10.1093/ejcts/ezz160
[3] PARK B, SUNG K, PARK P W. Clinical implication of transaortic mitral Pannus removal during repeat cardiac surgery for patients with mechanical mitral valve[J]. Circ J, 2018, 82(2): 396-402. doi: 10.1253/circj.CJ-17-0463
[4] 王蕊, 李静. 超声心动图对左室舒张性心力衰竭患者左心形态及舒张功能的评估价值[J]. 实用临床医药杂志, 2020, 24(3): 10-12, 15. doi: 10.7619/jcmp.202003003 [5] 李玲. 超声心动图评估主动脉瓣人工瓣膜置换置换术后室间隔运动异常情况[J]. 临床超声医学杂志, 2019, 21(3): 222-224. https://www.cnki.com.cn/Article/CJFDTOTAL-LCCY201903026.htm [6] COLOMBO T, RUSSO C, CILIBERTO G R, et al. Tricuspid regurgitation secondary to mitral valve disease: tricuspid annulus function as guide to tricuspid valve repair[J]. Cardiovasc Surg, 2001, 9(4): 369-377. doi: 10.1016/S0967-2109(00)00147-2
[7] 郑才斌. 128例再次心脏瓣膜置换术的临床分析[D]. 福州: 福建医科大学, 2018. [8] GAEDE L, BLUMENSTEIN J, KIM W K, et al. Trends in aortic valve replacement in Germany in 2015: transcatheter versus isolated surgical aortic valve repair[J]. Clin Res Cardiol, 2017, 106(6): 411-419. doi: 10.1007/s00392-016-1070-1
[9] SAAD A M, KASSIS N, ISOGAI T, et al. Trends in outcomes of transcatheter and surgical aortic valve replacement in the United States (2012-2017)[J]. Am J Cardiol, 2021, 141: 79-85. doi: 10.1016/j.amjcard.2020.10.065
[10] VAHANIAN A, BEYERSDORF F, PRAZ F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease[J]. Eur Heart J, 2022, 43(7): 561-632. doi: 10.1093/eurheartj/ehab395
[11] KIM Y J, KWON D A, KIM H K, et al. Determinants of surgical outcome in patients with isolated tricuspid regurgitation[J]. Circulation, 2009, 120(17): 1672-1678. doi: 10.1161/CIRCULATIONAHA.109.849448
[12] 何洁欣, 张莹. 超声心动图评估右心室功能的应用进展[J]. 岭南心血管病杂志, 2021, 27(4): 504-507. doi: 10.3969/j.issn.1007-9688.2021.04.23 [13] 于湖, 杨辉, 段佳庆, 等. 超声心动图在房间隔缺损患者介入封堵术中的应用价值[J]. 实用临床医药杂志, 2020, 24(6): 37-39, 43. doi: 10.7619/jcmp.202006010 [14] 刘英军. 左心瓣膜置换术后再次手术治疗三尖瓣功能性关闭不全的疗效分析[J]. 国际医药卫生导报, 2017, 23(5): 670-672. doi: 10.3760/cma.j.issn.1007-1245.2017.05.017 [15] 邓云丹, 李永波, 钱永军, 等. 二尖瓣置换术患者同期行三尖瓣成形术后两年超声心动图评价的随机对照试验[J]. 中国胸心血管外科临床杂志, 2016, 23(7): 658-665. https://www.cnki.com.cn/Article/CJFDTOTAL-ZXYX201607004.htm [16] 谢溟, 李佼珊. 尖瓣置换同期三尖瓣成形术对二尖瓣病变合并轻度功能性三尖瓣关闭不全的临床治疗效果分析[J]. 临床医药文献电子杂志, 2018, 5(71): 48-48. https://www.cnki.com.cn/Article/CJFDTOTAL-LCWX201871043.htm -
期刊类型引用(16)
1. 杨璐,吕家葆,尤佳,王兴生,梁银. 帕罗西汀联合整合式心理疗法对抑郁症患者的效果及社会功能的影响. 国际精神病学杂志. 2024(02): 470-473+485 .  百度学术
百度学术
2. 郑萍,刘宁. 近十年我国脑卒中后抑郁护理研究的阶段特征及趋势——基于CiteSpace的知识图谱分析. 保健医学研究与实践. 2022(09): 166-170 .  百度学术
百度学术
3. 王子健,肖鹏,杨冬林. 正念认知疗法对抑郁症患者心理状态和生活质量的干预效果评价. 中国健康教育. 2021(09): 850-853 .  百度学术
百度学术
4. 李海军,张庆玉,苏童,苏万鋆. 个性化护理干预在改善重症脑卒中患者神经康复与反刍思维中的效果分析. 检验医学与临床. 2020(13): 1906-1909 .  百度学术
百度学术
5. 张秀辉. 针灸联合优质护理对脑卒中后焦虑、抑郁的影响. 中西医结合心血管病电子杂志. 2020(20): 68 .  百度学术
百度学术
6. 陈明霞,郑亚琦,冷伟. 正念疗法联合个体化药物治疗对老年抑郁症患者焦虑抑郁状态、日常生活能力和社会功能的影响. 实用医院临床杂志. 2019(02): 63-66 .  百度学术
百度学术
7. 柳杰,王静,钟洁. 优质护理对脑卒中患者康复效果的影响. 中国实用神经疾病杂志. 2019(05): 556-561 .  百度学术
百度学术
8. 翁宏娜. 优质护理服务对因缺血性卒中所致早期神经功能恶化患者神经功能和日常生活能力的影响. 中医临床研究. 2019(14): 70-74 .  百度学术
百度学术
9. 段颖. 优质护理干预对抑郁症伴自杀倾向患者心理健康和生活质量的影响分析. 心理月刊. 2019(17): 51-52 .  百度学术
百度学术
10. 韩雪. 早期综合康复护理联合优质护理对急性脑卒中患者神经功能、运动功能及预后的影响. 中国当代医药. 2019(30): 216-218 .  百度学术
百度学术
11. 刘荣. 优质护理对脑卒中伴抑郁患者独立生活能力以及心理状态的影响. 当代临床医刊. 2018(02): 3718-3719 .  百度学术
百度学术
12. 赵倩,张华平,陆海娟,倪春初. 优质护理服务用于康复科护理管理中的效果观察. 中医药管理杂志. 2018(11): 134-136 .  百度学术
百度学术
13. 叶乐乐. 营养治疗对卒中患者营养状况、吞咽功能以及生活质量的影响. 肿瘤代谢与营养电子杂志. 2018(03): 257-260 .  百度学术
百度学术
14. 谭琳. Orem自理模式护理对脑卒中患者心理状态及日常生活能力的影响. 中国民康医学. 2018(19): 96-98 .  百度学术
百度学术
15. 谢红. 心理疏导联合康复护理治疗脑卒中抑郁症随机平行对照评价. 实用心脑肺血管病杂志. 2018(S2): 130-132 .  百度学术
百度学术
16. 肖彬新,兰碧玉,林芳. 综合护理对脑卒中患者心理状态与生活质量的影响. 中国现代医生. 2017(32): 142-145 .  百度学术
百度学术
其他类型引用(2)




 下载:
下载:
 苏公网安备 32100302010246号
苏公网安备 32100302010246号
