Effects of different surgery methods on anti-mullerian hormone level and perioperative indicators in ovarian chocolate cyst patients
-
摘要:目的
比较不同手术方式对卵巢巧克力囊肿患者血清抗缪勒管激素(AMH)水平和围术期指标的影响, 并分析患者术后不良妊娠结局的影响因素。
方法回顾性选取102例卵巢巧克力囊肿患者作为研究对象,根据手术方式的不同分为腹腔镜组70例和开腹组32例。腹腔镜组采用腹腔镜下卵巢巧克力囊肿剥除术治疗,开腹组采用开腹囊肿剥除术治疗。观察并比较2组患者围术期指标、手术前后血清AMH水平,分析卵巢巧克力囊肿患者术后不良妊娠结局的影响因素。
结果腹腔镜组手术时间(51.34±5.82) min、术中出血量(27.83±5.62) mL、住院时间(6.99±1.39) d、排气时间(10.71±1.63) h, 分别短于或少于开腹组的(79.97±6.98) min、(50.16±15.24) mL、(11.66±1.49) d、(26.75±3.69) h, 差异有统计学意义(P < 0.05)。术后,腹腔镜组、开腹组AMH水平分别为(2.51±1.41)、(1.84±1.23) ng/mL, 均低于术前,但腹腔镜组高于开腹组,差异有统计学意义(P < 0.05)。多因素Logistic回归分析显示,年龄、病程、囊肿患侧、盆腔粘连、输卵管功能、术前不孕、术后助孕、手术方式、AMH水平均为术后不良妊娠结局的独立影响因素(P < 0.05)。术前AMH水平预测术后不良妊娠结局的曲线下面积为0.704, 特异度为0.859, 敏感度为0.763, 界值为1.765。
结论与开腹囊肿剥除术相比,腹腔镜下卵巢巧克力囊肿剥除术对患者血清AMH水平的影响更小,且各项围术期指标更优。年龄、病程、囊肿患侧、盆腔粘连、输卵管功能、术前不孕、术后助孕、手术方式、AMH水平均可影响卵巢巧克力囊肿患者术后妊娠结局,其中术前AMH水平可预测术后不良妊娠结局。
Abstract:ObjectiveTo analyze effect of varied surgeries the changes of serum anti-mullerian hormone (AMH) and influencing factors of adverse pregnancy in patients with ovarian chocolate cyst after laparoscopic surgery.
MethodsThe clinical data of 102 patients with ovarian chocolate cyst treated in Bozhou People's Hospital were collected retrospectively. They were divided into laparoscopy group (70 cases) and laparotomy group (32 cases) according to the operation methods. The laparoscopic group was treated with laparoscopic ovarian chocolate cyst exfoliation, and the open group was treated with laparotomy. The clinical indexes and the changes of serum AMH before and after operation were compared between the two groups, and the influencing factors of postoperative adverse pregnancy outcomes in patients with ovarian chocolate cyst were analyzed.
ResultsThe operation time (51.34±5.82) min, intraoperative bleeding (27.83±5.62) mL, hospital stay (6.99±1.39) d and exhaust time (10.71±1.63) h in the laparoscopic group were significantly lower or shorter than (79.97±6.98) min, (50.16±15.24) mL, (11.66±1.49) d and (26.75±3.69) h in the open group (P < 0.05). After surgery, AMH levels in the laparoscopic group and the open group were (2.51±1.41) and (1.84±1.23) ng/mL, respectively, which were lower than those before surgery, but the above indicators in the laparoscopic group were higher than those in the open group (P < 0.05). Multivariate Logistic regression analysis showed that age, course of disease, side of cyst, pelvic adhesion, fallopian tube function, preoperative infertility, postoperative assisted pregnancy, surgical method and AMH level were all independent influencing factors of postoperative adverse pregnancy outcomes (P < 0.05). The area under the curve for preoperative AMH level in predicting postoperative adverse pregnancy outcome was 0.704, the specificity was 0.859, the sensitivity was 0.763, and the threshold was 1.765.
ConclusionCompared with laparotomy, laparoscopic chocolate cyst removal of ovary has less effect on serum AMH levels and better perioperative indicators. Age, course of disease, side of cyst, pelvic adhesion, fallopian tube function, preoperative infertility, postoperative assistance for pregnancy, surgical method and AMH level can all affect the postoperative pregnancy outcomes of chocolate ovarian cyst patients, and preoperative AMH level can be used as a clinical indicator to predict postoperative adverse pregnancy outcomes.
-
卵巢巧克力囊肿是指子宫内膜异位后在卵巢中生长,随月经周期出血积攒而成的囊肿[1]。卵巢巧克力囊肿是子宫内膜异位症的一种表现形式,主要症状为痛经、慢性盆腔痛、月经量增多、经期延长和不孕等。目前,卵巢巧克力囊肿的发病机制尚未阐明,患者大多采用药物、手术方式进行治疗[2]。药物治疗对机体的损伤较小,主要适用于绝经前或近绝经期女性,手术治疗对于症状相对较轻、病灶较大、年龄偏小的女性而言是首选方案[3]。近年来,腹腔镜技术的临床应用范围日益扩大,且已有学者[4]证实腹腔镜手术相较其他手术方式对卵巢功能伤害更小。血清抗缪勒管激素(AMH)可作为卵巢储备功能的评估指标,能够清晰显示机体卵巢状态[5]。本研究回顾性分析102例卵巢巧克力囊肿患者的临床资料,比较不同手术方式对患者血清AMH水平的影响,并分析术后不良妊娠结局的影响因素,现报告如下。
1. 资料与方法
1.1 一般资料
采用回顾性研究方式收集2018年1月—2020年6月于亳州市人民医院接受治疗的102例卵巢巧克力囊肿患者的临床资料,根据手术方式的不同将患者分为腹腔镜组70例和开腹组32例。纳入标准: ①符合《子宫内膜异位症中西医结合诊治指南》[6]中卵巢巧克力囊肿的诊断标准者; ②年龄20~40岁,未绝经者; ③有强烈生育意愿,符合巧克力囊肿手术适应证者; ④配偶无精液异常或其他影响生育疾病者; ⑤无手术禁忌证者; ⑥手术前后均检测AHM水平者。排除标准: ①入院前1个月内接受性激素治疗者; ②合并其他机体内分泌疾病者; ③合并肝肾功能异常、心脑血管疾病、恶性肿瘤(如结直肠癌)、不宜妊娠类疾病者; ④临床资料缺失、随访缺失者。腹腔镜组患者年龄21~36岁,平均(28.76±3.10)岁; 病程1~22个月,平均(12.11±4.12)个月; 囊肿直径4.68~9.21 cm, 平均(7.11±0.88) cm。开腹组患者年龄20~37岁,平均(28.06±3.61)岁; 病程2~21个月,平均(12.03± 4.83)个月; 囊肿直径4.96~8.99 cm, 平均(7.21±0.98) cm。2组患者一般资料比较,差异均无统计学意义(P>0.05), 具有可比性。
1.2 方法
开腹组采用开腹囊肿剥除术治疗,全身麻醉后逐层切开进入腹腔,确定病灶位置后去除病灶,用可吸收线缝合止血,缝合切口。腹腔镜组采用腹腔镜下卵巢巧克力囊肿剥除术治疗,将患者置于平卧位,进行全身麻醉,麻醉起效后于患者脐部做1个开口(1 cm), 将套针置入腹腔,建立人工气腹(充入CO2气体使腹腔内气压达到14 mmHg); 放置12 mm腹腔镜Trocar, 探查病灶位置; 通过腹腔镜于脐部左侧、右侧与骼前上棘连线外侧穿孔,判断内环境状态(有无积血、子宫内膜异位等); 吸取囊液,进行冲洗,分离粘连,游离囊肿; 加大卵巢表面切口,用2把分离钳夹取囊壁,反向牵引剥除囊壁; 修剪卵巢包膜,用可吸收线缝合止血,用生理盐水冲洗盆腔,探查腹盆腔是否存在其他病灶。2组患者术后均接受预防感染及能量补充处理。
1.3 观察指标
① 围术期指标: 记录患者手术时间、术中出血量、住院时间和排气时间。② AHM水平: 分别于手术实施前月经期第2天与手术实施后月经期第2天对患者进行静脉采血(3 mL), 3 000转/min离心10 min, 取上层血清置于-20 ℃冰箱保存。取血清用全自动酶免仪(意大利AdaItis公司,型号LAB)测定AMH水平,试剂盒购于南京诺唯赞医疗科技有限公司(产品批号20182400783)。③妊娠结局: 收集患者术后18个月电话随访或门诊随访结果,记录术后备孕1年未妊娠以及妊娠期高血压、早产、流产等不良妊娠结局发生情况。④输卵管功能: 输卵管功能异常是指单侧或双侧输卵管存在闭合、粘连、发育不全、畸形、中部阶段缺失或存在输卵管缩短、卷曲等现象,输卵管功能正常是指输卵管无上述现象。
1.4 统计学处理
采用SPSS 22.0统计学软件分析数据,计数资料以[n(%)]表示,比较采用χ2检验; 服从正态分布的计量资料如围术期指标、年龄、囊肿直径等以(x±s)表示,比较行t检验; 不符合正态分布的计量资料采用[M(P25, P75)]表示,行非参数检验。采用单因素分析和多因素Logistic回归分析探讨术后不良妊娠结局的影响因素; 构建受试者工作特征(ROC)曲线,分析AMH水平预测术后不良妊娠结局的价值。P < 0.05为差异有统计学意义。
2. 结果
2.1 围术期指标比较
腹腔镜组手术时间、住院时间、排气时间均短于开腹组,术中出血量少于开腹组,差异有统计学意义(P < 0.05), 见表 1。
表 1 2组患者围术期指标比较(x±s)组别 n 手术时间/min 术中出血量/mL 住院时间/d 排气时间/h 开腹组 32 79.97±6.98 50.16±15.24 11.66±1.49 26.75±3.69 腹腔镜组 70 51.34±5.82* 27.83±5.62* 6.99±1.39* 10.71±1.63* 与开腹组比较, * P < 0.05。 2.2 手术前后血清AMH水平比较
术前, 2组患者血清AMH水平比较,差异无统计学意义(P>0.05); 术后, 2组患者血清AMH水平均低于术前,但腹腔镜组血清AMH水平高于开腹组,差异有统计学意义(P < 0.05),见表 2。
表 2 2组手术前后血清抗缪勒管激素水平比较(x±s)ng/mL 组别 n 术前 术后 开腹组 32 3.12±1.98 1.84±1.23* 腹腔镜组 70 3.10±2.01 2.51±1.41*# 与术前比较, * P < 0.05; 与开腹组比较, #P < 0.05。 2.3 术后妊娠结局的影响因素分析
102例患者术后不良妊娠结局发生率为37.25%(38/102)。单因素分析结果显示,不同妊娠结局患者在年龄、病程、囊肿患侧、盆腔粘连、输卵管功能、术前不孕、术后助孕、手术方式和AMH水平方面比较,差异有统计学意义(P < 0.05), 见表 3。以单因素分析中差异有统计学意义的指标为自变量,以术后妊娠结局为因变量,进行多因素Logistic回归分析,结果显示,年龄、病程、囊肿患侧、盆腔粘连、输卵管功能、术前不孕、术后助孕、手术方式、AMH水平均为术后不良妊娠结局的独立影响因素(P < 0.05), 见表 4。
表 3 术后妊娠结局的单因素分析(x±s)[n(%)][M(P25, P75)]因素 分类 妊娠结局良好(n=64) 妊娠结局不良(n=38) χ2/t/Z P 年龄/岁 27.61±2.68 30.11±3.59 -3.995 < 0.001 病程/月 9.97±3.83 15.66±2.33 -8.277 < 0.001 囊肿直径/cm 7.07±0.85 7.27±0.99 -1.035 0.303 囊肿患侧 单侧 59(92.19) 22(57.89) 17.150 < 0.001 双侧 5(7.81) 16(42.11) 盆腔粘连 有 15(23.44) 22(57.89) 12.246 < 0.001 无 49(76.56) 16(42.11) 输卵管功能 正常 58(90.62) 20(52.63) 19.128 < 0.001 受损 6(9.38) 18(47.37) 术前不孕 是 41(64.06) 34(89.47) 7.910 0.005 否 23(35.94) 4(10.53) 术后助孕 是 19(29.69) 4(10.53) 5.012 0.025 否 45(70.31) 34(89.47) 手术方式 腹腔镜下囊肿剥除术 49(76.56) 21(55.26) 5.024 0.025 开腹囊肿剥除术 15(23.44) 17(44.74) 抗缪勒管激素/(ng/mL) 4.18(2.45, 5.06) 1.30(0.98, 2.56) -3.433 0.001 表 4 术后不良妊娠结局的多因素Logistic回归分析因素 β S. E. Wald P OR 95%CI 年龄 0.287 0.083 11.841 0.001 1.332 1.131~1.569 病程 1.045 0.222 22.111 < 0.001 2.844 1.840~4.398 囊肿患侧 -1.954 0.715 7.471 0.006 0.142 0.035~0.575 盆腔粘连 2.096 0.643 10.615 0.001 8.135 2.305~28.711 输卵管功能 -2.095 0.666 9.894 0.002 0.123 0.330~0.454 术前不孕 2.613 0.930 7.888 0.005 13.641 2.202~84.497 术后助孕 -2.047 0.882 5.388 0.020 0.129 0.023~0.727 手术方式 -0.972 0.440 4.887 0.027 0.378 0.160~0.869 抗缪勒管激素水平 -0.455 0.119 14.533 < 0.001 0.634 0.502~0.802 常量 -14.402 3.523 16.710 < 0.001 < 0.001 — 2.4 AMH水平预测术后不良妊娠结局的ROC曲线分析
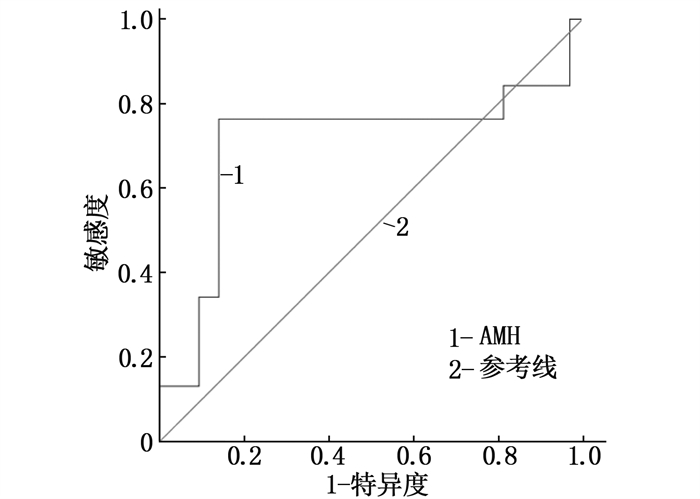
ROC曲线分析结果显示,术前AMH水平预测术后不良妊娠结局的曲线下面积为0.704, 特异度为0.859, 敏感度为0.763, 界值为1.765, 见图 1。
3. 讨论
流行病学调查[7]显示,卵巢巧克力囊肿在育龄妇女中的发病率为10%~15%。近年来,卵巢巧克力囊肿的发病率有所上升,且生育晚的女性发病率显著高于生育早的女性[8-9]。临床治疗卵巢巧克力囊肿多选用腹腔镜手术,但部分患者对腹腔镜治疗存在不适症状,仍需实施开腹手术[10-11]。卵巢储备功能可反映女性机体内卵子与激素生产能力, AMH参与调节卵泡发育,其水平在月经周期内较为稳定,是目前临床较为常用的卵巢功能评价指标, AMH水平下降提示卵巢储备功能不全,此时卵泡池可能有提早耗竭的情况,卵泡生长功能受到抑制。卵巢巧克力囊肿患者术后卵巢功能受到不同程度的损害, AMH水平下降,调控卵泡发育、性腺外神经内分泌能力减弱,故而可能影响妊娠率以及流产、早产、妊娠期高血压疾病等不良妊娠结局发生率[12]。
本研究结果显示,腹腔镜组与开腹组患者术后AMH水平显著低于术前,说明2种手术治疗方式对患者卵巢功能均有一定损害,其原因主要为剥除囊肿可能对卵巢组织产生一定损伤,但腹腔镜组AMH水平下降程度低于开腹组,说明与常规开腹治疗相比,腹腔镜治疗的损害相对较小。剥离卵巢巧克力囊肿组织时,卵泡、滤泡会出现丢失[13], 且手术会对卵巢内环境造成一定损害,导致机体出现炎症,影响卵巢功能[11, 14-15], 而腹腔镜手术创口较小,手术更精准,故手术损伤和炎症反应更轻。本研究结果还显示,腹腔镜组手术时间、住院时间、排气时间均显著短于开腹组,术中出血量显著少于开腹组,进一步证实腹腔镜手术影响更小,患者术后恢复更快。
本研究102例患者中有38例出现不良妊娠结局,其中腹腔镜手术患者的不良妊娠结局发生率为30.00%(21/70), 开腹手术患者的不良妊娠结局发生率为53.13%(17/32), 提示腹腔镜手术能够在一定程度上降低患者术后不良妊娠结局发生率。单因素分析和多因素Logistic回归分析结果显示,年龄、病程、囊肿患侧、盆腔粘连、输卵管功能、术前不孕、术后助孕、手术方式和AMH水平均可影响患者术后妊娠结局。分析原因如下: 年龄可影响术后子宫恢复速率,年龄低的患者恢复更快; 双侧囊肿患者的手术损伤较单侧囊肿患者更严重,恢复时间更长; 盆腔粘连、输卵管功能可通过抑制卵子排出而影响受孕; 与术前可妊娠的患者、病程不长的患者相比,术前不孕的患者、病程长的患者子宫结构及微环境异常程度更高,治疗效果会受到一定程度影响; 术后接受助孕干预的患者对机体情况了解更透彻,可更有针对性地改善术后妊娠结局; AMH水平可反映卵巢功能,卵巢功能较差的患者术后出现不良妊娠结局的概率更高[16-18]。ROC曲线分析结果显示,术前AMH水平预测术后不良妊娠结局的曲线下面积为0.704, 特异度为0.859, 敏感度为0.763, 界值为1.765, 表明术前AMH水平对术后不良妊娠结局具有一定预测价值。
综上所述,与开腹囊肿剥除术相比,腹腔镜下卵巢巧克力囊肿剥除术对患者血清AMH水平的影响更小,且术中出血量、手术时间、住院时间等围术期指标结果更优。年龄、病程、囊肿患侧、盆腔粘连、输卵管功能、术前不孕、术后助孕、手术方式和AMH水平均为术后妊娠结局的独立影响因素,且术前AMH水平可作为预测术后不良妊娠结局的临床指标。但本研究随访观察时间较短,未来还需进一步开展长期随访研究加以证实。
-
表 1 2组患者围术期指标比较(x±s)
组别 n 手术时间/min 术中出血量/mL 住院时间/d 排气时间/h 开腹组 32 79.97±6.98 50.16±15.24 11.66±1.49 26.75±3.69 腹腔镜组 70 51.34±5.82* 27.83±5.62* 6.99±1.39* 10.71±1.63* 与开腹组比较, * P < 0.05。 表 2 2组手术前后血清抗缪勒管激素水平比较(x±s)
ng/mL 组别 n 术前 术后 开腹组 32 3.12±1.98 1.84±1.23* 腹腔镜组 70 3.10±2.01 2.51±1.41*# 与术前比较, * P < 0.05; 与开腹组比较, #P < 0.05。 表 3 术后妊娠结局的单因素分析(x±s)[n(%)][M(P25, P75)]
因素 分类 妊娠结局良好(n=64) 妊娠结局不良(n=38) χ2/t/Z P 年龄/岁 27.61±2.68 30.11±3.59 -3.995 < 0.001 病程/月 9.97±3.83 15.66±2.33 -8.277 < 0.001 囊肿直径/cm 7.07±0.85 7.27±0.99 -1.035 0.303 囊肿患侧 单侧 59(92.19) 22(57.89) 17.150 < 0.001 双侧 5(7.81) 16(42.11) 盆腔粘连 有 15(23.44) 22(57.89) 12.246 < 0.001 无 49(76.56) 16(42.11) 输卵管功能 正常 58(90.62) 20(52.63) 19.128 < 0.001 受损 6(9.38) 18(47.37) 术前不孕 是 41(64.06) 34(89.47) 7.910 0.005 否 23(35.94) 4(10.53) 术后助孕 是 19(29.69) 4(10.53) 5.012 0.025 否 45(70.31) 34(89.47) 手术方式 腹腔镜下囊肿剥除术 49(76.56) 21(55.26) 5.024 0.025 开腹囊肿剥除术 15(23.44) 17(44.74) 抗缪勒管激素/(ng/mL) 4.18(2.45, 5.06) 1.30(0.98, 2.56) -3.433 0.001 表 4 术后不良妊娠结局的多因素Logistic回归分析
因素 β S. E. Wald P OR 95%CI 年龄 0.287 0.083 11.841 0.001 1.332 1.131~1.569 病程 1.045 0.222 22.111 < 0.001 2.844 1.840~4.398 囊肿患侧 -1.954 0.715 7.471 0.006 0.142 0.035~0.575 盆腔粘连 2.096 0.643 10.615 0.001 8.135 2.305~28.711 输卵管功能 -2.095 0.666 9.894 0.002 0.123 0.330~0.454 术前不孕 2.613 0.930 7.888 0.005 13.641 2.202~84.497 术后助孕 -2.047 0.882 5.388 0.020 0.129 0.023~0.727 手术方式 -0.972 0.440 4.887 0.027 0.378 0.160~0.869 抗缪勒管激素水平 -0.455 0.119 14.533 < 0.001 0.634 0.502~0.802 常量 -14.402 3.523 16.710 < 0.001 < 0.001 — -
[1] LIU M J, ZHANG L, XIA Y, et al. New consideration of herlyn-Werner-wunderlich syndrome diagnosed by ultrasound[J]. J Ultrasound Med, 2021, 40(9): 1893-1900. doi: 10.1002/jum.15572
[2] ROS C, DE GUIRIOR C, MENSION E, et al. Transvaginal ultrasound for diagnosis of deep endometriosis involving uterosacral ligaments, torus uterinus and posterior vaginal fornix: prospective study[J]. Ultrasound Obstet Gynecol, 2021, 58(6): 926-932. doi: 10.1002/uog.23696
[3] 杜华文. 卵巢巧克力囊肿患者术后复发的影响因素分析[J]. 中国妇幼保健, 2020, 35(15): 2774-2776. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB202015013.htm [4] 杨智红, 陈光元, 谢家滨, 等. AMH在妇科腹腔镜手术前后卵巢功能中的评估价值[J]. 医学临床研究, 2018, 35(1): 8-10, 14. doi: 10.3969/j.issn.1671-7171.2018.01.003 [5] 马远东, 刘小彩, 毛凌哲. 两种分离方案对卵巢巧克力囊肿术后卵巢功能的影响[J]. 中国妇幼健康研究, 2019, 30(2): 240-243. doi: 10.3969/j.issn.1673-5293.2019.02.025 [6] 中国中西医结合学会妇产科专业委员会. 子宫内膜异位症中西医结合诊治指南[J]. 中国中西医结合杂志, 2019, 39(10): 1169-1176. doi: 10.7661/j.cjim.20190923.288 [7] ROMAN H, PROSSZER M, MARABHA J, et al. Live surgery of colorectal endometriosis broadcasted from a surgeon's routine operating theater is not associated with higher complications rate[J]. Acta Obstet Gynecol Scand, 2021, 100(12): 2176-2185. doi: 10.1111/aogs.14264
[8] 顾利华, 张婷婷. 腹腔镜下卵巢巧克力囊肿剥除术对卵巢功能及助孕结局的影响[J]. 中国性科学, 2019, 28(11): 63-68. doi: 10.3969/j.issn.1672-1993.2019.11.016 [9] 王凯丽, 祁秀娟. 卵巢子宫内膜异位囊肿不孕患者腹腔镜术后妊娠结局的影响因素分析[J]. 生殖医学杂志, 2019, 28(5): 488-493. doi: 10.3969/j.issn.1004-3845.2019.05.007 [10] 王金花, 李利. 不同腹腔镜术式对卵巢巧克力囊肿剥除术患者卵巢储备功能的影响[J]. 中国现代手术学杂志, 2018, 22(3): 201-204. https://www.cnki.com.cn/Article/CJFDTOTAL-XDSS201803010.htm [11] 杨屹, 康瑛, 罗金维. 腹腔镜下卵巢囊肿剥除术对不同性质卵巢囊肿患者卵巢储备功能的影响[J]. 中国性科学, 2019, 28(4): 68-72. doi: 10.3969/j.issn.1672-1993.2019.04.019 [12] 何翌晨, 吴琰婷, 黄荷凤. 抗苗勒管激素与女性生殖结局关系的研究进展[J]. 中华生殖与避孕杂志, 2020, 40(9): 767-772. doi: 10.3760/cma.j.cn101441-20200522-00300 [13] 谷小梅. 腹腔镜下卵巢巧克力囊肿剥除术联合GnRHa对卵巢功能的影响[J]. 中国计划生育学杂志, 2019, 27(2): 166-170. https://www.cnki.com.cn/Article/CJFDTOTAL-JHSY201902009.htm [14] 孙东梅, 朱张颍, 陶敏芳. 通过AMH、抑制素B探讨腹腔镜卵巢囊肿剥除术对卵巢功能的影响[J]. 生殖医学杂志, 2019, 28(11): 1329-1333. https://www.cnki.com.cn/Article/CJFDTOTAL-SZYX201911016.htm [15] 肖惠超, 陈继明. 腹腔镜卵巢囊肿剥除术治疗卵巢囊肿的临床效果[J]. 实用临床医药杂志, 2020, 24(11): 118-120. doi: 10.7619/jcmp.202011032 [16] 张船华, 王家建. 卵巢子宫内膜异位囊肿腹腔镜术后复发的相关因素分析[J]. 中国妇幼保健, 2019, 34(23): 5348-5351. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB201923008.htm [17] 宋华, 邬绍新, 张伟, 等. 改良腹腔镜下巨大卵巢囊肿剥除术32例报告[J]. 中国微创外科杂志, 2018, 18(8): 758-760. doi: 10.3969/j.issn.1009-6604.2018.08.021 [18] 查萍, 陈莹. 开腹卵巢囊肿剥除术与腹腔镜卵巢囊肿剥除术治疗良性卵巢囊肿的效果比较[J]. 实用临床医药杂志, 2020, 24(5): 110-113. doi: 10.7619/jcmp.202005030 -
期刊类型引用(9)
1. 任杰. 戈舍瑞林联合腹腔镜卵巢囊肿剥除术治疗卵巢巧克力囊肿的回顾性研究. 临床医学. 2025(01): 42-44 .  百度学术
百度学术
2. 张鹏玲,黄建璇,蔡楠,孙军萍. 凝血指标、生育指数评分与卵巢巧克力囊肿不孕术后妊娠的相关性分析. 实用医院临床杂志. 2025(02): 155-159 .  百度学术
百度学术
3. 冯钰玲,余姝婷. GnRH-a联合地诺孕素在卵巢巧克力囊肿术后维持治疗中的应用效果分析. 延边大学医学学报. 2025(02): 88-91 .  百度学术
百度学术
4. 章斌斌. 地诺孕素联合醋酸亮丙瑞林缓释微球应用于卵巢子宫内膜异位囊肿术后治疗的临床效果. 临床合理用药. 2024(25): 16-18+22 .  百度学术
百度学术
5. 车艳美. 卵巢巧克力囊肿术后患者使用地诺孕素的临床效果研究. 实用妇科内分泌电子杂志. 2023(01): 17-19 .  百度学术
百度学术
6. 侯宇飞,卜范玉. 地诺孕素不同给药时间对经腹腔镜术治疗卵巢巧克力囊肿的疗效及复发情况的影响. 中国药物经济学. 2023(10): 61-65 .  百度学术
百度学术
7. 吴珊. 腹腔镜卵巢囊肿剥除术结合醋酸亮丙瑞林治疗卵巢巧克力囊肿患者的临床疗效分析. 现代诊断与治疗. 2023(16): 2458-2460 .  百度学术
百度学术
8. 杨姣妹. 经腹部与经阴道超声联合检查在卵巢巧克力囊肿与盆腔炎性囊肿中的鉴别诊断价值分析. 影像研究与医学应用. 2023(21): 152-154 .  百度学术
百度学术
9. 刘杨雪珂,刘青,许文文. 超声介入治疗在卵巢巧克力囊肿患者中的应用价值. 透析与人工器官. 2023(04): 9-12 .  百度学术
百度学术
其他类型引用(0)




 下载:
下载:
 苏公网安备 32100302010246号
苏公网安备 32100302010246号