Effect of ambrisentan combined with sildenafil evaluated by echocardiograph on right ventricular pulmonary arterial coupling in patients with severe pulmonary hypertension
-
摘要:目的
探讨超声心动图评估安立生坦联合西地那非对重度肺动脉高压(PAH)患者右心室-肺动脉耦联(RVPAC)影响的可行性及临床相关因素。
方法选取33例重度PAH患者作为研究对象,给予安立生坦(5~10 mg/d)和西地那非(50 mg/d)连续治疗至少6个月。采用酶联免疫吸附试验(ELISA)法检测血浆N末端-B型利钠肽前体(NT-proBNP)水平,并检测平均肺动脉压(mPAP)、肺动脉楔压(PAWP)、肺血管阻力(PVR)和心脏指数(CI);使用超声心动图测量患者常规超声参数,并计算RVPAC指标,包括右心室面积变化分数(RVFAC)/肺动脉收缩压(PASP)、三尖瓣环平面收缩偏移(TAPSE)/PASP、三尖瓣环收缩期速度(S')/PASP和右心室每搏量(RVSV)/右心室收缩末容积(RVESV)。治疗后常规随访6个月,并记录患者临床预后,以死亡为终点事件。采用二分类Logisitc回归分析法分析RVPAC指标与患者预后的关联;绘制受试者工作特征(ROC)曲线,分析RVPAC指标预测临床预后的效能。
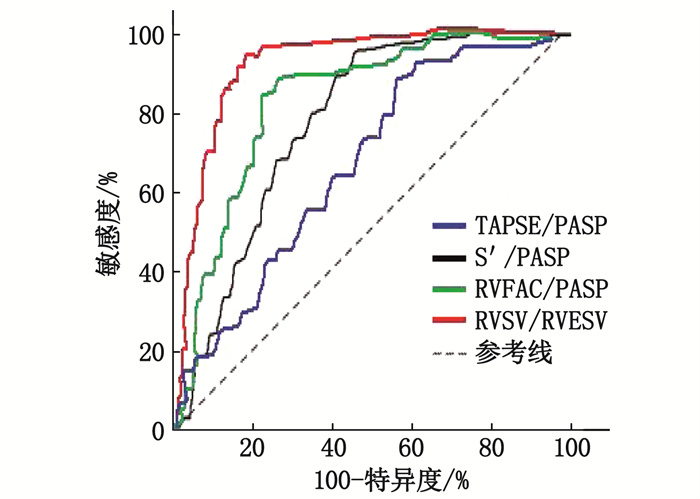
结果33例患者治疗6个月后NT-proBNP水平为356.7(141.8,1 126.2)pg/mL,低于治疗前的1 748.4(696.8,3 012.4)pg/mL,差异有统计学意义(P < 0.001)。相较于治疗前,患者治疗后S'、TAPSE、右心室射血分数(RVEF)、RVFAC升高,PASP、RVESV降低,RVFAC/PASP、TAPSE/PASP、S'/PASP、RVSV/RVESV升高,差异均有统计学意义(P < 0.05)。Spearman检验显示,治疗前RVFAC/PASP、TAPSE/PASP、S'/PASP、RVSV/RVESV均分别与NT-proBNP、mPAP、PAWP、PVR呈负相关(P < 0.001),且均分别与收缩末期弹性/肺动脉弹性(Ees/Ea)呈正相关(P < 0.001)。33例患者中,6例发生终点事件。二分类Logisitc回归分析显示,治疗前RVFAC/PASP、TAPSE/PASP、S'/PASP、RVSV/RVESV降低均为终点事件的危险因素(P < 0.05)。ROC曲线显示,治疗前RVFAC/PASP、TAPSE/PASP、S'/PASP和RVSV/RVESV预测临床预后的曲线下面积分别为0.839、0.745、0.768和0.856。
结论安立生坦联合西地那非治疗重度PAH可显著改善RVPAC,基于超声心动图无创检测的RVPAC指标与NT-proBNP和右心导管术测量指标具有较好的相关性,且RVPAC指标还可用于评估患者的临床预后。
Abstract:ObjectiveTo explore the feasibility and clinical relevant factors of ambrisentan combined with sildenafil evaluated by echocardiograph in right ventricular pulmonary arterial coupling(RVPAC) patients with severe pulmonary hypertension (PAH).
MethodsA total of 33 patients with severe PAH were selected as research objects, ambesentan (5 to 10 mg/d) and sildenafil (50 mg/d) were given for at least 6 months. Plasma N-terminal pro-B-type natriuretic peptide (NT-proBNP) was detected by Enzyme linked immunosorbent assay (ELISA). Mean pulmonary artery pressure (mPAP), pulmonary arterial wedge pressure (PAWP), pulmonary vascular resistance (PVR) and cardiac index (CI) were measured by right heart catheterization. Conventional ultrasonic parameters were measured by echocardiography, and RVPAC related indexes including right ventricular fractional area change/pulmonary arterial systolic pressure (RVFAC/PASP), tricuspid annular plane systolic excursion(TAPSE)/PASP, tricuspid annular systolic velocity(S')/PASP and right ventricular stroke volume(RVSV)/right ventricular end systolic volume(RVESV)were calculated. The patients were followed up for 6 months, clinical prognosis was recorded, and end event was death. The correlations between RVPAC indexes and prognosis were analyzed by binary Logistic regression; receiver operating curve (ROC) was used to analyze the efficacy of RVPAC indexes for predicting clinical prognosis.
ResultsThe level of NT-proBNP in 33 patients after 6 months treatment was significantly lower than before treatment[356.7(141.8, 1 126.2) pg/mL versus 1 748.4(696.8, 3 012.4) pg/mL, P < 0.001]. After treatment, S', TAPSE, right ventricular ejection fraction (RVEF) and RVFAC increased significantly, while PASP and RVESV decreased significantly, RVFAC/PASP, TAPSE/PASP, S'/PASP and RVSV/RVESV also increased significantly compared with before treatment (P < 0.05). Spearman test showed that RVFAC/PASP, TAPSE/PASP, S'/PASP and RVSV/RVESV were separately negatively correlated with NT-proBNP, mPAP, PAWP and PVR before treatment (P < 0.001), and were all positively correlated with end-systolic elastance-to-arterial elastance ratio (Ees/Ea) (P < 0.05). A total of 6 patients occurred endpoint events in 33 patients. Binary Logistic regression analysis showed that decreased RVFAC/PASP, TAPSE/PASP, S'/PASP and RVSV/RVESV before treatment were risk factors of the endpoint events (P < 0.05). ROC showed that area under the curve of RVFAC/PASP, TAPSE/PASP, S'/PASP and RVSV/RVESV before treatment in prediction of clinical prognosis were 0.839, 0.745, 0.768 and 0.856, respectively.
ConclusionAmbrisentan combined with sildenafil in treatment of severe PAH could improve RVPAC. RVPAC indexes based on non-invasive echocardiographic detection has good correlations with NT-proBNP and right heart catheterization measurement index, and RVPAC index can also be used to evaluate the clinical prognosis of patients. RVPAC can also be used to evaluate clinical prognosis of patient.
-
-
表 1 33例患者治疗前后超声指标比较(x±s)[n(%)]
指标 治疗前 治疗后 t/χ2 P S′/(cm/s) 9.3±1.9 12.5±2.6 6.325 0.001 E/E′ 6.9±2.4 6.7±2.5 0.854 0.321 TAPSE/mm 14.2±1.9 17.8±2.6 5.754 0.005 三尖瓣反流 轻度 6(18.2) 8(24.2) 1.534 0.464 中度 18(54.5) 20(60.6) 重度 9(27.3) 5(15.2) PASP/mmHg 105.4±26.9 89.7±23.3 10.235 < 0.001 RVSV/mL 47.5±16.7 50.2±18.9 1.021 0.125 RVESV/mL 64.5±16.3 53.4±15.2 9.624 < 0.001 RVEF/% 40.9±4.3 46.8±4.2 7.521 < 0.001 RVFAC/% 28.6±5.4 36.5±7.9 6.635 0.001 S′: 三尖瓣环收缩期速度; E/E′: 二尖瓣舒张早期血流峰值速度/二尖瓣环舒张早期运动峰值速度; TAPSE: 三尖瓣环平面收缩偏移; PASP: 肺动脉收缩压; RVSV: 右心室每搏量; RVESV: 右心室收缩末容积; RVEF: 右心室射血分数; RVFAC: 右心室面积变化分数。 表 2 33例患者治疗前后RVPAC指标比较(x±s)
指标 治疗前 治疗后 t P (RVFAC/PASP)/(%/mmHg) 0.29±0.06 0.42±0.13 13.326 < 0.001 (TAPSE/PASP)/(mm/mmHg) 0.14±0.03 0.19±0.05 6.859 < 0.001 (S′/PASP)/[cm/(s·mmHg)] 0.09±0.02 0.13±0.04 5.756 0.001 RVSV/RVESV 0.81±0.19 0.96±0.22 6.323 0.001 RVFAC/PASP: 右心室面积变化分数/肺动脉收缩压; TAPSE/PASP: 三尖瓣环平面收缩偏移/肺动脉收缩压; S′/PASP: 三尖瓣环收缩期速度/肺动脉收缩压; RVSV/RVESV: 右心室每搏量/右心室收缩末容积。 表 3 治疗前RVPAC指标与NT-proBNP和右心导管术指标的相关性分析
指标 NT-proBNP mPAP PAWP PVR CI Ees/Ea r P r P r P r P r P r P RVFAC/PASP -0.856 < 0.001 -0.868 < 0.001 -0.796 < 0.001 -0.736 < 0.001 -0.052 0.569 0.785 < 0.001 TAPSE/PASP -0.831 < 0.001 -0.821 < 0.001 -0.827 < 0.001 -0.767 < 0.001 0.203 0.675 0.749 < 0.001 S′/PASP -0.798 < 0.001 -0.909 < 0.001 -0.906 < 0.001 -0.752 < 0.001 -0.113 0.756 0.827 < 0.001 RVSV/RVESV -0.813 < 0.001 -0.848 < 0.001 -0.862 < 0.001 -0.831 < 0.001 -0.231 0.542 0.863 < 0.001 NT-proBNP: N末端-B型利钠肽前体; mPAP: 平均肺动脉压; PAWP: 肺动脉楔压; PVR: 肺血管阻力; CI: 心脏指数; Ees/Ea: 收缩末期弹性/肺动脉弹性。 表 4 治疗前RVPAC指标与预后的二分类Logisitc回归分析
因素 β Wald P OR 95%CI RVFAC/PASP -0.458 8.021 < 0.001 2.011 1.654~2.342 TAPSE/PASP -0.369 6.754 < 0.001 1.853 1.426~2.103 S′/PASP -0.526 11.203 < 0.001 2.423 1.759~2.854 RVSV/RVESV -0.237 5.526 < 0.001 1.654 1.231~1.967 表 5 治疗前RVPAC指标对临床预后的预测效能
指标 AUC 95%CI P 敏感度/% 特异度/% RVFAC/PASP 0.839 0.745~0.902 < 0.001 83.3 80.7 TAPSE/PASP 0.745 0.667~0.832 < 0.001 80.5 74.6 S′/PASP 0.768 0.696~0.855 < 0.001 75.9 81.2 RVSV/RVESV 0.856 0.765~0.934 < 0.001 89.6 95.3 -
[1] THENAPPAN T, ORMISTON M L, RYAN J J, et al. Pulmonary arterial hypertension: pathogenesis and clinical management[J]. BMJ, 2018, 360: j5492.
[2] KUWANA M, BLAIR C, TAKAHASHI T, et al. Initial combination therapy of ambrisentan and tadalafil in connective tissue disease-associated pulmonary arterial hypertension (CTD-PAH) in the modified intention-to-treat population of the AMBITION study: post hoc analysis[J]. Ann Rheum Dis, 2020, 79(5): 626-634. doi: 10.1136/annrheumdis-2019-216274
[3] MONZO L, REICHENBACH A, AL-HITI H, et al. Acute unloading effects of sildenafil enhance right ventricular-pulmonary artery coupling in heart failure[J]. J Card Fail, 2021, 27(2): 224-232. doi: 10.1016/j.cardfail.2020.11.007
[4] BESHAY S, SAHAY S, HUMBERT M. Evaluation and management of pulmonary arterial hypertension[J]. Respir Med, 2020, 171: 106099. doi: 10.1016/j.rmed.2020.106099
[5] TELLO K, DALMER A, AXMANN J, et al. Reserve of right ventricular-arterial coupling in the setting of chronic overload[J]. Circ Heart Fail, 2019, 12(1): e005512. doi: 10.1161/CIRCHEARTFAILURE.118.005512
[6] NOCHIOKA K, ROCA G Q, CLAGGETT B, et al. Right ventricular function, right ventricular-pulmonary artery coupling, and heart failure risk in 4 US communities: the atherosclerosis risk in communities (ARIC) study[J]. JAMA Cardiol, 2018, 3(10): 939-948. doi: 10.1001/jamacardio.2018.2454
[7] FORTON K, MOTOJI Y, CARAVITA S, et al. Exercise stress echocardiography of the pulmonary circulation and right ventricular-arterial coupling in healthy adolescents[J]. Eur Heart J Cardiovasc Imaging, 2021, 22(6): 688-694. doi: 10.1093/ehjci/jeaa085
[8] HOEPER M M, GHOFRANI H A, GRVNIG E, et al. Pulmonary hypertension[J]. Dtsch Arztebl Int, 2017, 114(5): 73-84.
[9] KRISHNAN A, MARKHAM R, SAVAGE M, et al. Right heart catheterisation: how to do it[J]. Heart Lung Circ, 2019, 28(4): 71-78. doi: 10.1016/j.hlc.2018.08.005
[10] 袁文悦, 宋宏宁, 郭瑞强. 超声心动图定量分析早期心功能受损的研究进展[J]. 临床超声医学杂志, 2022, 24(1): 48-52. https://www.cnki.com.cn/Article/CJFDTOTAL-LCCY202201010.htm [11] MEHMOOD M. Right ventricular-pulmonary artery coupling-let's not lose the forest for the trees[J]. JAMA Cardiol, 2019, 4(2): 188.
[12] GALIō N, CHANNICK R N, FRANTZ R P, et al. Risk stratification and medical therapy of pulmonary arterial hypertension[J]. Eur Respir J, 2019, 53(1): 1801889. doi: 10.1183/13993003.01889-2018
[13] BASHLINE M J, SIMON M A. Use of tricuspid annular plane systolic excursion/pulmonary artery systolic pressure as a non-invasive method to assess right ventricular-PA coupling in patients with pulmonary hypertension[J]. Circ Cardiovasc Imaging, 2019, 12(7): e009648.
[14] JONE P N, SCHÄFER M, PAN Z X, et al. Right ventricular-arterial coupling ratio derived from 3-dimensional echocardiography predicts outcomes in pediatric pulmonary hypertension[J]. Circ Cardiovasc Imaging, 2019, 12(1): e008176.
[15] VONK NOORDEGRAAF A, WESTERHOF B E, WESTERHOF N. The relationship between the right ventricle and its load in pulmonary hypertension[J]. J Am Coll Cardiol, 2017, 69(2): 236-243. doi: 10.1016/j.jacc.2016.10.047
[16] VRIZ O, PIRISI M, BOSSONE E, et al. Right ventricular-pulmonary arterial uncoupling in mild-to-moderate systemic hypertension[J]. J Hypertens, 2020, 38(9): 274-281.
[17] VONK NOORDEGRAAF A, CHIN K M, HADDAD F, et al. Pathophysiology of the right ventricle and of the pulmonary circulation in pulmonary hypertension: an update[J]. Eur Respir J, 2019, 53(1): 1801900. doi: 10.1183/13993003.01900-2018
[18] TELLO K, AXMANN J, GHOFRANI H A, et al. Relevance of the TAPSE/PASP ratio in pulmonary arterial hypertension[J]. Int J Cardiol, 2018, 266: 229-235. doi: 10.1016/j.ijcard.2018.01.053
[19] JENTZER J C, ANAVEKAR N S, REDDY Y N V, et al. Right ventricular pulmonary artery coupling and mortality in cardiac intensive care unit patients[J]. J Am Heart Assoc, 2021, 10(7): e019015. doi: 10.1161/JAHA.120.019015
[20] BRAGANÇA B, TRÊPA M, SANTOS R, et al. Echocardiographic assessment of right ventriculo-arterial coupling: clinical correlates and prognostic impact in heart failure patients undergoing cardiac resynchronization therapy[J]. J Cardiovasc Imaging, 2020, 28(2): 109-120.
-
期刊类型引用(13)
1. 刘春晓,何磊,张玲玲,李国良. 阿立哌唑联合脑循环系统治疗仪治疗精神分裂症的临床效果. 临床医药实践. 2025(01): 62-65 .  百度学术
百度学术
2. 张荣洪,邱吉明,刘菲,刘慧珍. 在不同肌松药联合丙泊酚麻醉下无抽搐电休克治疗对精神分裂症患者的影响. 中国医学创新. 2024(01): 53-56 .  百度学术
百度学术
3. 戴艺荣,叶小惠. 阿立哌唑联合无抽搐电休克治疗难治性精神分裂症的临床效果观察. 中国现代药物应用. 2024(07): 29-33 .  百度学术
百度学术
4. 沈洁. 研究无抽搐电休克治疗精神病患者的临床安全性. 系统医学. 2024(04): 97-99+106 .  百度学术
百度学术
5. 徐昕,赵楠,庞檬佼. 电休克治疗对精神分裂症患者认知功能及执行功能的影响. 心理月刊. 2024(06): 79-81 .  百度学术
百度学术
6. 马娟,丁宁,丁木兵. 精神分裂症患者的治疗依从性影响因素分析及对生活质量和生活能力的影响. 海军医学杂志. 2024(05): 521-525 .  百度学术
百度学术
7. 翁武彪,林剑凌,周长青. 无抽搐电休克治疗联合磁共振仪监测对精神分裂症患者短时瞬间记忆功能及对脑电功能的影响. 中国医疗器械信息. 2023(03): 128-130 .  百度学术
百度学术
8. 李世兴. 无抽搐电休克联合阿立哌唑对精神分裂症患者疗效及血清BDNF、S100B水平的影响. 中国现代药物应用. 2023(07): 124-127 .  百度学术
百度学术
9. 方钱禹,吴艳,程良红. 无抽搐电休克联合喹硫平对双相情感障碍躁狂发作患者氧化应激水平及认知功能的影响. 中国医学创新. 2023(12): 47-51 .  百度学术
百度学术
10. 李亚娇. 不同频次无抽搐电休克辅助治疗精神分裂症住院患者的效果. 中外医学研究. 2023(12): 116-120 .  百度学术
百度学术
11. 杨越琪,郑小涵,朱岩,周志勇,李晓欧. 八通道经颅刺激脑电调控系统的设计. 计算机测量与控制. 2022(01): 161-167 .  百度学术
百度学术
12. 吕杏放,罗肇明,夏伟梅,梁锐太,梁杰,罗端庆. 6种抗精神病药物治疗女性精神分裂症患者的效果及不良反应分析. 中外医学研究. 2022(16): 10-14 .  百度学术
百度学术
13. 秦荣,雷秀雯. 计算机认知矫正联合药物治疗对精神分裂症康复期患者心理推理能力和视空间工作记忆能力的影响. 内科. 2021(06): 750-753+784 .  百度学术
百度学术
其他类型引用(0)




 下载:
下载:
 苏公网安备 32100302010246号
苏公网安备 32100302010246号
