Development and validation of a risk prediction model for renal anemia in non-dialysis chronic kidney disease patients
-
摘要:目的
探讨非透析慢性肾脏病(CKD)患者发生肾性贫血的影响因素,建立非透析CKD患者发生肾性贫血的风险模型,并验证预测模型的有效性。
方法回顾性分析2017年1月—2021年12月收治的非透析CKD患者的临床资料,按7∶3比例随机分为训练集(n=388)与验证集(n=165)。利用单因素和多因素Logistic回归分析筛选影响肾性贫血的影响因素,基于赤池信息准则(AIC)最小值选取最终预测因素构建列线图,并验证模型效能。
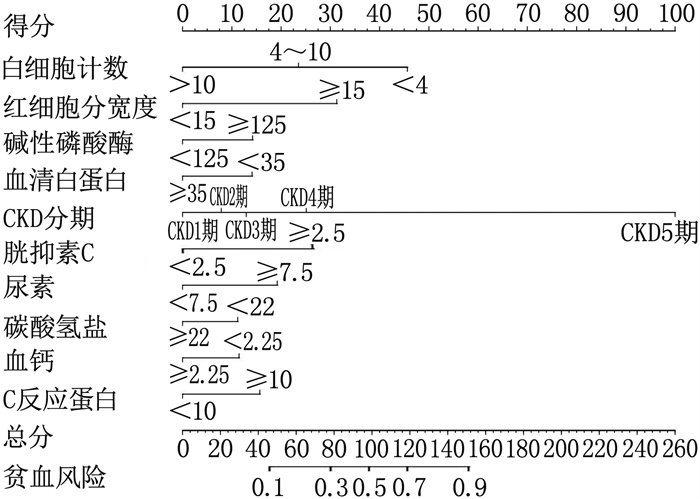
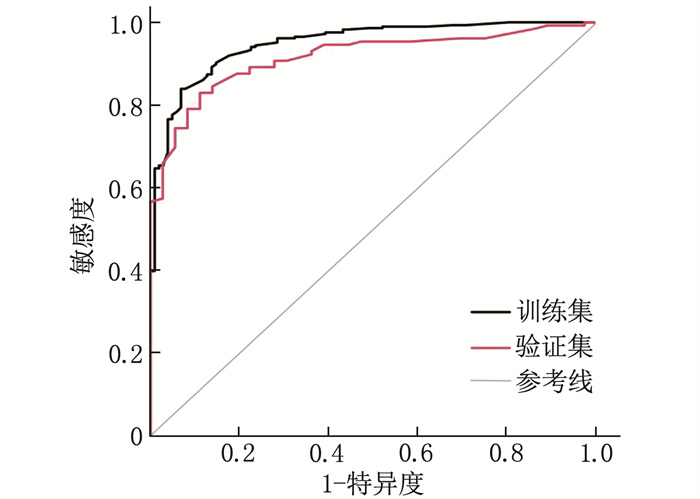
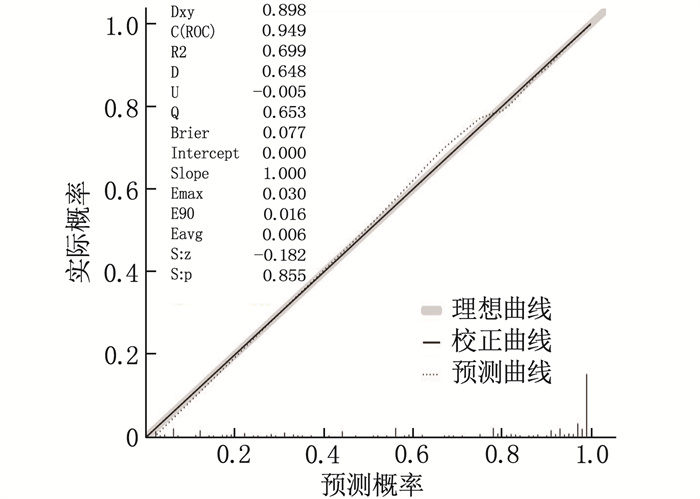
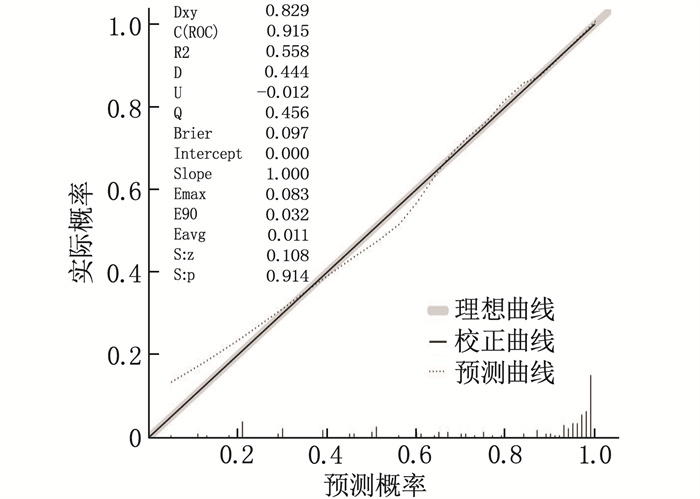
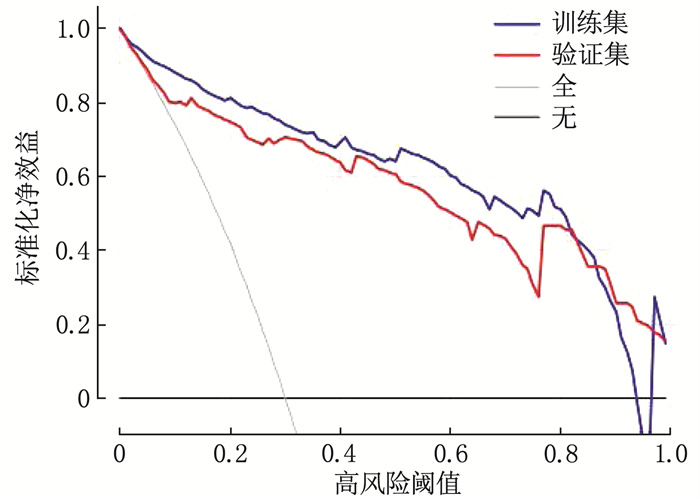
结果单因素Logistic回归分析显示, 17个变量[白细胞计数、中性粒细胞百分比、红细胞分布宽度(RDW)、血小板压积、碱性磷酸酶、血清白蛋白(ALB)、血胱抑素C、尿素、CKD分期、碳酸氢钠、血钾、血钙、血磷、C反应蛋白(CRP)、甘油三酯、尿白蛋白、尿隐血]与贫血的发生相关(P < 0.05)。多因素Logistic回归分析结果提示,白细胞计数、CRP、RDW、ALB、血胱抑素C、尿素、CKD分期、碳酸氢盐、血钙是贫血独立影响因素(P < 0.05)。利用危险因素构建列线图,经验证模型具有较好的区分度[训练集ROC曲线下面积(AUC)为0.915(95%CI: 0.870~0.959), 验证集为0.949(95%CI: 0.927~0.971)]。校准曲线及H-L检验均提示模型预测值与实际值差异无统计学意义(P>0.05)。临床决策曲线分析(DCA)表明该模型具有良好的临床应用价值。
结论本研究开发的预测模型能较好地预测非透析CKD患者肾性贫血的发生风险,为临床决策提供参考。
Abstract:ObjectiveTo investigate the influencing factors of renal anemia in non-dialysis chronic kidney disease (CKD) patients, and to establish a risk model of renal anemia in non-dialysis CKD patients and verify its validity.
MethodsThe clinical data of non-dialysis CKD patients admitted from January 2017 to December 2021 were retrospectively analyzed. The patients were randomly divided into training set (n=388) and validation set (n=165) at a ratio of 7∶3. Univariate and multivariate Logistic regression analysis was used to screen out the influencing factors for renal anemia. Based on the minimum Akaike Information Criterion (AIC) criterion, the final predictors were selected to construct the nomogram, and the efficiency of the model was verified.
ResultsMultivariate Logistic regression analysis showed that 17 variables including white blood cell, percentage of neutrophil granulocyte, erythrocyte distribution width (RDW), thrombocytocrit, alkaline phosphatase, serum albumin (ALB), cystatin C, urea, CKD stage, bicarbonate, potassium, calcium, phosphorus, C-reactive protein (CRP), triglyceride, urinary albumin, occult urine were associated with anemia(P < 0.05). Multiple Logistic regression analysis showed that white blood cell count, CRP, RDW, ALB, cystatin C, urea, CKD stage, bicarbonate and blood calcium were independent influencing factors for anemia (P < 0.05). Using risk factors to construct a nomogram, the validation model had good discrimination [the area under ROC curve (AUC) of the training set was 0.915(95%CI, 0.870 to 0.959), and the validation set was 0.949(95%CI, 0.927 to 0.971)]. The calibration curve and H-L test showed that there was no significant difference between the predicted value and the actual value of the model(P>0.05). The clinical decision curve analysis (DCA) showed that the model had good clinical application value.
ConclusionThe model developed in this study can better predict the risk of renal anemia in non-dialysis CKD patients, and provide reference for clinical decision-making.
-
Keywords:
- non-dialysis chronic renal disease /
- anemia /
- risk factors /
- prediction model /
- nomogram /
- differentiation degree
-
-
表 1 训练集及验证集基本资料比较[n(%)]
变量 分类 训练集 验证集 贫血组(n=286) 非贫血组(n=102) 合计(n=388) 贫血组(n=129) 非贫血组(n=36) 合计(n=165) 年龄 18~44岁 59 29 88(22.7) 30 12 42(25.5) 45~60岁 120 36 156(40.2) 42 18 60(36.4) > 60岁 107 37 144(37.1) 57 6 63(38.2) 性别 男 159 57 216(55.7) 82 16 98(59.4) 女 127 45 172(44.3) 47 20 67(40.6) 高血压 有 220 69 289(74.5) 102 27 129(78.2) 无 66 33 99(25.5) 27 9 36(21.8) 糖尿病 有 82 33 115(29.6) 44 9 53(32.1) 无 204 69 273(70.4) 85 27 112(67.9) 白细胞计数 < 4×109/L 18 1 19(4.9) 11 0 11(6.7) (4~10)×109/L 242 86 328(84.5) 107 29 136(82.4) > 10×109/L 26 15 41(10.6) 11 7 18(10.9) 中性粒细胞百分比 < 70% 108 56 164(42.3) 54 26 80(48.5) ≥70% 78 46 124(57.7) 75 10 85(51.5) 淋巴细胞百分比 < 40% 280 99 379(97.7) 127 36 163(98.8) ≥40% 6 3 9(2.3) 2 0 2(1.2) 红细胞分布宽度 < 15% 224 101 325(83.8) 110 36 146(88.5) ≥15% 62 1 63(16.2) 19 0 19(11.5) 血小板计数 < 300×109/L 237 86 323(83.2) 115 30 145(87.9) ≥300×109/L 49 16 65(16.8) 14 6 20(12.1) 平均血小板容积 < 9 fl 19 2 21(5.4) 6 0 6(3.6) ≥9 fl 267 100 367(94.6) 123 36 159(96.4) 血小板分布宽度 < 17% 277 94 371(95.6) 126 31 157(95.2) ≥17% 9 8 17(4.4) 3 5 8(4.8) 血小板压积 < 0.23% 147 32 179(46.1) 73 7 80(48.5) ≥0.23% 139 70 209(53.9) 56 29 85(51.5) 碱性磷酸酶 < 125 U/L 252 98 350(90.2) 119 34 153(92.7) ≥125 U/L 34 4 38(9.8) 10 2 12(7.3) 白蛋白 < 35 g/L 127 15 142(36.6) 47 9 56(33.9) ≥35 g/L 159 87 246(63.4) 82 27 109(66.1) 球蛋白 < 35 g/L 214 81 295(76) 90 29 119(72.1) ≥35 g/L 72 21 93(24) 39 7 46(27.9) 血胱抑素C < 2.5 mg/L 60 88 148(38.1) 28 30 58(35.2) ≥2.5 mg/L 226 14 240(61.9) 101 6 107(67.8) 尿素 < 7.5 mmol/L 11 44 55(14.2) 5 7 12(7.3) ≥7.5 mmol/L 275 58 333(85.8) 124 29 153(92.7) 慢性肾脏病分期 CKD1期 12 45 57(14.7) 9 12 21(12.7) CKD2期 23 26 49(12.6) 9 12 21(12.7) CKD3期 97 28 125(32.2) 38 10 48(29.1) CKD4期 81 3 84(21.6) 33 1 34(20.6) CKD5期 73 0 73(18.8) 40 1 41(24.8) 尿酸 < 420 μmol/L 115 50 165(42.5) 50 17 67(40.6) ≥420 μmol/L 171 52 223(57.5) 79 19 98(59.4) 碳酸氢盐 < 22 mmol/L 150 19 169(43.6) 57 5 62(37.6) ≥22 mmol/L 136 83 219(56.4) 72 31 103(62.4) 钾 < 5.5 mmol/L 231 96 327(84.3) 110 35 145(87.9) ≥5.5 mmol/L 55 6 61(15.7) 19 1 20(12.1) 钠 < 145 mmol/L 265 96 361(93) 119 34 153(92.7) ≥145 mmol/L 21 6 27(7) 10 2 12(7.3) 钙 < 2.25 mmol/L 227 46 273(70.4) 102 14 116(70.3) ≥2.25 mmol/L 59 56 115(29.6) 27 22 49(29.7) 磷 < 1.61 mmol/L 165 99 264(68) 70 33 103(62.4) ≥1.61 mmol/L 121 3 124(32) 59 3 62(37.6) C反应蛋白 < 10 mmol/L 204 94 298(76.8) 90 32 122(73.9) ≥10 mmol/L 82 8 90(23.2) 39 4 43(26.1) 总胆固醇 < 5.72 mmol/L 235 76 311(80.2) 114 22 136(82.4) ≥5.72 mmol/L 51 26 77(19.8) 15 14 29(17.6) 甘油三酯 < 1.7 mmol/L 158 40 198(51) 62 12 74(44.8) ≥1.7 mmol/L 128 62 190(49) 67 24 91(55.2) 高密度脂蛋白 < 0.9 mmol/L 92 26 118(30.4) 48 10 58(35.2) ≥0.9 mmol/L 194 76 270(69.6) 81 26 107(67.8) 低密度脂蛋白 < 4.1 mmol/L 266 95 361(93) 126 30 156(94.5) ≥4.1 mmol/L 20 7 27(7) 3 6 9(5.5) 尿白蛋白 0 30 29 59(15.2) 14 10 24(14.5) + 37 21 58(14.9) 22 4 26(15.8) 
85 26 111(28.6) 39 7 46(27.9) 
118 20 138(35.6) 46 13 59(35.8) 
16 6 22(5.7) 8 2 10(6.1) 尿隐血 0 99 60 159(41) 55 11 66(40.0) + 95 19 114(29.4) 37 9 46(27.9) 
68 14 82(21.1) 27 88 35(21.2) 
24 9 33(8.5) 10 8 18(10.9) 表 2 单因素及多因素Logistic回归分析
变量 分类 单因素分析 多因素分析 OR(95%CI) P OR(95%CI) P 年龄 18~44岁 1 45~60岁 1.64(0.92~2.93) 0.095 — — > 60岁 1.42(0.80~2.54) 0.235 — — 性别 女 1 男 0.99(0.63~1.56) 0.96 — — 高血压 无 1 有 1.59(0.97~2.62) 0.066 — — 糖尿病 无 1 有 0.84(0.52~1.37) 0.485 — — 白细胞计数 < 4×109/L 1 (4~10)×109/L 0.16(0.02~1.19) 0.073 0.13(0.01~2.10) 0.150 >10×109/L 0.10(0.01~0.80) 0.03 0.01(0~0.33) 0.008 中性粒细胞百分比 < 70% 1 — — ≥70% 2.01(1.27~3.17) 0.003 — — 淋巴细胞百分比 < 40% 1 ≥40% 0.71(0.17~2.88) 0.629 — — 红细胞分布宽度 < 15% 1 ≥15% 27.96(3.82~204.39) 0.001 18.03(1.97~164.85) 0.010 血小板计数 < 300×109/L 1 ≥300×109/L 1.11(0.60~2.06) 0.737 — — 平均血小板体积 < 9 fl 1 ≥9 fl 0.28(0.06~1.23) 0.092 — — 血小板分布宽度 < 17% 1 ≥17% 0.38(0.14~1.02) 0.054 — — 血小板压积 < 0.23 fl 1 ≥0.23 fl 0.43(0.27~0.70) 0.001 — — 碱性磷酸酶 < 125 U/L 1 ≥125 U/L 3.31(1.14~9.56) 0.027 3.72(0.68~20.39) 0.130 白蛋白 < 35 g/L 1 ≥35 g/L 0.22(0.12~0.39) 0 0.27(0.11~0.70) 0.007 球蛋白 < 35 g/L 1 ≥35 g/L 1.30(0.75~2.25) 0.352 — — 血胱抑素C < 2.5 mg/L 1 ≥2.5 mg/L 23.68(12.60~44.50) 0 2.85(1.06~7.71) 0.039 尿素 < 7.5 mmol/L 1 ≥7.5 mmol/L 18.97(9.24~38.94) 0 5.90(2.04~17.08) 0.001 慢性肾脏病分期 CKD1期 1 CKD2期 3.32(1.42~7.75) 0.006 2.06(0.69~6.15) 0.193 CKD3期 12.99(6.06~27.85) 0 3.30(1.06~10.28) 0.040 CKD4期 101.25(27.13~377.93) 0 10.19(1.70~61.09) 0.011 CKD5期 433682 972.79(0~Inf) 0.979 86 627 793.63(0~Inf) 0.987 尿酸 < 420 mmol/L 1 ≥420 mmol/L 1.43(0.91~2.25) 0.123 — — 碳酸氢钠 < 22 mmol/L 1 ≥22 mmol/L 0.21(0.12~0.36) 0 0.36(0.15~0.82) 0.016 钾 < 5.5 mmol/L 1 ≥5.5 mmol/L 3.81(1.59~9.15) 0.003 — — 钠 < 145 mmol/L 1 ≥145 mmol/L 1.27(0.50~3.24) 0.619 — — 钙 < 2.25 mmol/L 1 ≥2.25 mmol/L 0.21(0.13~0.35) 0.000 0.35(0.16~0.75) 0.007 磷 < 1.61 mmol/L 1 ≥1.61 mmol/L 24.20(7.50~78.13) 0.000 — — C反应蛋白 < 10 mmol/L 1 ≥10 mmol/L 4.72(2.19~10.16) 0.000 4.26(1.19~15.20) 0.025 总胆固醇 < 5.72 mmol/L 1 ≥5.72 mmol/L 0.63(0.37~1.09) 0.098 — — 甘油三酯 < 1.7 mmol/L 1 ≥1.7 mmol/L 0.52(0.33~0.83) 0.006 — — 高密度脂蛋白 < 0.9 mmol/L 1 ≥0.9 mmol/L 0.72(0.43~1.20) 0.209 — — 低密度脂蛋白 < 4.1 mmol/L 1 ≥4.1 mmol/L 1.02(0.42~2.49) 0.965 — — 尿白蛋白 0 1 + 1.70(0.81~3.57) 0.158 — — 
3.16(1.61~6.20) 0.001 — — 
5.70(2.84~11.44) 0.000 — — 
2.58(0.89~7.50) 0.082 — — 尿隐血 0 1 + 3.03(1.68~5.46) 0.000 — — 
2.94(1.52~5.69) 0.001 — — 
1.62(0.70~3.71) 0.257 — — -
[1] KIM-MITSUYAMA S, SOEJIMA H, YASUDA O, et al. Anemia is an independent risk factor for cardiovascular and renal events in hypertensive outpatients with well-controlled blood pressure: a subgroup analysis of the ATTEMPT-CVD randomized trial[J]. Hypertens Res, 2019, 42(6): 883-891. doi: 10.1038/s41440-019-0210-1
[2] LEE G, CHOI S, KIM K, et al. Association of hemoglobin concentration and its change with cardiovascular and all-cause mortality[J]. J Am Heart Assoc, 2018, 7(3): e007723. doi: 10.1161/JAHA.117.007723
[3] ECKARDT K U, AGARWAL R, ASWAD A, et al. Safety and efficacy of vadadustat for Anemia in patients undergoing dialysis[J]. N Engl J Med, 2021, 384(17): 1601-1612. doi: 10.1056/NEJMoa2025956
[4] BALACHANDRAN V P, GONEN M, SMITH J J, et al. Nomograms in oncology: more than meets the eye[J]. Lancet Oncol, 2015, 16(4): e173-e180. doi: 10.1016/S1470-2045(14)71116-7
[5] Kidney Disease Improving Global Outcomes. KDIGO clinical practice guideline for anemia in chronic kidney disease[J]. Kidney Int Suppl, 2012, 12(2): 279-335. http://www.guideline.gov/summaries/downloadcontent/ngc-9272?contentType=pdf
[6] RYU S R, PARK S K, JUNG J Y, et al. The prevalence and management of Anemia in chronic kidney disease patients: result from the KoreaN cohort study for outcomes in patients with chronic kidney disease (KNOW-CKD)[J]. J Korean Med Sci, 2017, 32(2): 249-256. doi: 10.3346/jkms.2017.32.2.249
[7] 韩蓓, 韩俊岭, 曹靖昊, 等. 全段成纤维细胞生长因子23与维持性血液透析患者肾性贫血的相关性研究[J]. 实用临床医药杂志, 2021, 25(21): 114-118. doi: 10.7619/jcmp.20213812 [8] CHONCHOL M, LIPPI G, MONTAGNANA M, et al. Association of inflammation with anaemia in patients with chronic kidney disease not requiring chronic dialysis[J]. Nephrol Dial Transplant, 2008, 23(9): 2879-2883. doi: 10.1093/ndt/gfn109
[9] KEITHI-REDDY S R, ADDABBO F, PATEL T V, et al. Association of anemia and erythropoiesis stimulating agents with inflammatory biomarkers in chronic kidney disease[J]. Kidney Int, 2008, 74(6): 782-790. doi: 10.1038/ki.2008.245
[10] BEGUM S, LATUNDE-DADA G O. Anemia of inflammation with an emphasis on chronic kidney disease[J]. Nutrients, 2019, 11(10): 2424. doi: 10.3390/nu11102424
[11] HONG N, KIM C O, YOUM Y, et al. Elevated red blood cell distribution width is associated with morphometric vertebral fracture in community-dwelling older adults, independent of Anemia, inflammation, and nutritional status: the Korean urban rural elderly (KURE) study[J]. Calcif Tissue Int, 2019, 104(1): 26-33. doi: 10.1007/s00223-018-0470-9
[12] BAMGBOLA O F. Pattern of resistance to erythropoietin-stimulating agents in chronic kidney disease[J]. Kidney Int, 2011, 80(5): 464-474. doi: 10.1038/ki.2011.179
[13] ANGELINI A, CAPPUCCILLI M L, MAGNONI G, et al. The link between homocysteine, folic acid and vitamin B12 in chronic kidney disease[J]. G Ital Nefrol, 2021, 38(4): 221-226. http://pubmed.ncbi.nlm.nih.gov/34469084/
[14] CAPPUCCILLI M, BERGAMINI C, GIACOMELLI F A, et al. Vitamin B supplementation and nutritional intake of methyl donors in patients with chronic kidney disease: a critical review of the impact on epigenetic machinery[J]. Nutrients, 2020, 12(5): 1234. doi: 10.3390/nu12051234
[15] XANTHOPOULOS A, TRYPOSKIADIS K, DIMOS A, et al. Red blood cell distribution width in elderly hospitalized patients with cardiovascular disease[J]. World J Cardiol, 2021, 13(9): 503-513. doi: 10.4330/wjc.v13.i9.503
[16] WANG Y, WEI R B, SU T Y, et al. Clinical and pathological factors of renal anaemia in patients with IgA nephropathy in Chinese adults: a cross-sectional study[J]. BMJ Open, 2019, 9(1): e023479. doi: 10.1136/bmjopen-2018-023479
[17] BORONAT M, SANTANA Á, BOSCH E, et al. Relationship between Anemia and serum concentrations of calcium and phosphorus in advanced non-dialysis-dependent chronic kidney disease[J]. Nephron, 2016, 135(2): 97-104. http://www.onacademic.com/detail/journal_1000039682676610_2b0b.html
[18] 万三红. CKD患者贫血的多因素及特点分析[D]. 长春: 吉林大学, 2018. [19] 束金莲, 李贺, 姚少峰, 等. 首次透析患者贫血的相关危险因素回顾性研究[J]. 中国现代医学杂志, 2021, 31(17): 96-100. doi: 10.3969/j.issn.1005-8982.2021.17.017 [20] MUN K C, KIM H C, KWAK C S. Cyanate as a hemolytic factor[J]. Ren Fail, 2000, 22(6): 809-814. doi: 10.1081/JDI-100101966
[21] MUN K C, GOLPER T A. Impaired biological activity of erythropoietin by cyanate carbamylation[J]. Blood Purif, 2000, 18(1): 13-17. doi: 10.1159/000014403
[22] PARK K D, MUN K C, CHANG E J, et al. Inhibition of erythropoietin activity by cyanate[J]. Scand J Urol Nephrol, 2004, 38(1): 69-72. doi: 10.1080/00365590310006291
[23] 赵洪雯, 吴雄飞, 刘宏. 尿毒症毒素对大鼠培养骨髓细胞红细胞生成素受体的影响[J]. 重庆医学, 2003, 32(6): 678-681. doi: 10.3969/j.issn.1671-8348.2003.06.016 [24] 李晓亮, 张黎. 中性粒细胞明胶酶相关脂质运载蛋白在诊断肾性贫血及评估病情中的应用价值[J]. 实用临床医药杂志, 2022, 26(18): 83-86. doi: 10.7619/jcmp.20221625 [25] JIA W P, WANG S S, LIU M, et al. Anemia in centenarians: prevalence and association with kidney function[J]. Hematology, 2020, 25(1): 26-33. doi: 10.1080/16078454.2019.1703448
[26] JONES H, TALWAR M, NOGUEIRA J M, et al. Anemia after kidney transplantation; its prevalence, risk factors, and independent association with graft and patient survival: a time-varying analysis[J]. Transplantation, 2012, 93(9): 923-928. doi: 10.1097/TP.0b013e31824b36fa
[27] TONG Q, HIRSCHLER-LASZKIEWICZ I, ZHANG W Y, et al. TRPC3 is the erythropoietin-regulated calcium channel in human erythroid cells[J]. J Biol Chem, 2008, 283(16): 10385-10395. doi: 10.1074/jbc.M710231200
[28] FENG Y, BOROSHA S, RATRI A, et al. DOT1L methyltransferase regulates calcium influx in erythroid progenitor cells in response to erythropoietin[J]. Int J Mol Sci, 2022, 23(9): 5137. doi: 10.3390/ijms23095137
[29] JIA W P, WANG S S, LIU M, et al. Anemia in centenarians: prevalence and association with kidney function[J]. Hematology, 2020, 25(1): 26-33. doi: 10.1080/16078454.2019.1703448
-
期刊类型引用(2)
1. 姬林娟,田欣,芮涛,姚永伟. 白细胞与红细胞比容比值对急性ST段抬高型心肌梗死再灌注治疗后院内主要不良心血管事件的预测价值. 实用临床医药杂志. 2024(15): 14-18+25 .  本站查看
本站查看
2. 莫妮娜. 冠心病冠状动脉介入术患者心功能改变及相关影响因素. 吉林医学. 2022(11): 2943-2946 .  百度学术
百度学术
其他类型引用(1)




 下载:
下载:
 苏公网安备 32100302010246号
苏公网安备 32100302010246号