The value of neutrophil-to-lymphocyte ratio combined with mean platelet volume-to-platelet count ratio in predicting the prognosis of patients with septic shock
-
摘要:目的
探讨早期外周血中性粒细胞与淋巴细胞比值(NLR)、平均血小板体积与血小板计数比值(MPV/PLT)对感染性休克患者预后的评估价值。
方法回顾性分析112例住院治疗的感染性休克患者的临床资料,根据28 d预后情况分为存活组69例和死亡组43例。比较2组患者年龄、性别、入院时休克指数、氧合指数、C反应蛋白(CRP)、降钙素原(PCT)、白细胞(WBC)、血乳酸(Lac)、急性生理学与慢性健康状况评分系统Ⅱ(APACHEⅡ)评分、序贯器官衰竭评估(SOFA)评分、D-二聚体等临床资料和入院24 h内NLR、MPV/PLT。绘制受试者工作特征(ROC)曲线,评估各项指标对感染性休克患者28 d死亡风险的预测价值;采用多因素Logistic回归分析法分析感染性休克患者预后的危险因素;采用Kaplan-Meier生存曲线分析不同NLR-MPV/PLT评分与总生存时间的相关性。
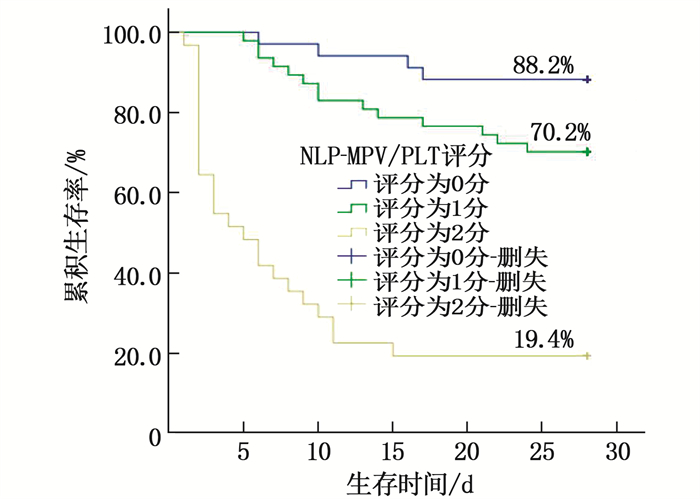
结果2组患者年龄、性别、休克指数、氧合指数、CRP比较,差异无统计学意义(P>0.05);死亡组NLR、MPV/PLT、WBC、PCT、Lac、D-二聚体、APACHEⅡ评分、SOFA评分高于存活组,差异有统计学意义(P < 0.05)。NLR预测患者死亡风险的曲线下面积(AUC)为0.724,当最佳截断值为12.49时,敏感度为74.4%,特异度为68.1%;MPV/PLT预测患者死亡风险的AUC为0.731,当最佳截断值为0.10时,敏感度为74.4%,特异度为69.6%。NLR、MPV/PLT、WBC、PCT、Lac、D-二聚体是感染性休克患者28 d死亡的独立影响因素(P < 0.05)。根据NLR-MPV/PLT评分将感染性休克患者分为0分组、1分组、2分组,其28 d累积生存率分别为88.2%、70.2%、19.4%,差异有统计学意义(P < 0.05)。
结论早期NLR、MPV/PLT对感染性休克患者的预后具有较高的预测价值,可作为有效而简便的评估指标用于急诊患者的早期诊断和后续治疗的临床指导。
-
关键词:
- 感染性休克 /
- 中性粒细胞与淋巴细胞比值 /
- 平均血小板体积与血小板计数比值 /
- 预后
Abstract:ObjectiveTo investigate the value of early peripheral blood neutrophil-to-lymphocyte Ratio (NLR) combined with mean platelet volume-to-platelet count ratio (MPV/PLT) in evaluating the prognosis in patients with septic shock.
MethodsA total of 112 patients with infectious stroke who were hospitalized were retrospectively selected. According to the prognosis of the patients within 28 days, they were divided into survival group(n=69) and death group (n=43). Age, gender, shock index, oxygenation index, C-reactive protein (CRP), procalcitonin (PCT), white blood cell (WBC), lactic acid (Lac), acute physiology and chronic health evaluation Ⅱ(APACHEⅡ) score, sequential organ failure assessment (SOFA) score, D-dimer, NLR and MPV/PLT within 24 hours after admission were recorded. The receiver operating characteristic curve (ROC) was used to evaluate the clinical predictive value of various indicators for the 28-day mortality risk of patients with septic shock. Multivariate Logistic regression was used to analyze the risk factors for the prognosis of patients with septic shock. Kaplan-Meier survival curve was used to analyze the correlations of different NLR-MPV/PLT scores with overall survival.
ResultsThere were no significant differences in age, gender, shock index, oxygenation index, and CRP between the two groups (P>0.05). Compared with the survival group, NLR, MPV/PLT, WBC, PCT, Lac, D-dimer, APACHEⅡ score and SOFA score in the death group were higher than those in the control group(P < 0.05). The area under the curve (AUC) of NLR in predicting death risk was 0.724, when the optimal cut-off value was 12.49, the sensitivity was 74.4% and the specificity was 68.1%. The AUC for MPV/PLT in predicting death risk was 0.731, with a sensitivity of 74.4% and specificity of 69.6% when the optimal cut-off value was 0.10. NLR, MPV/PLT, WBC, PCT, Lac and D-dimer were independent influencing factors of death in septic shock patients at 28 d (P < 0.05). Patients with septic shock were divided into 0 score group, one score group, two scores group according to NLR-MPV/PLT score, the 28-day cumulative survival rates were 88.2%, 70.2% and 19.4%, respectively(P < 0.05).
ConclusionEarly NLR and MPV/PLT have high predictive value for the prognosis of septic shock patients, which can be used as effective and simple evaluation index for early diagnosis of emergency patients and clinical guidance for follow-up treatment.
-
脓毒症是一种可危及生命的疾病,由机体对感染的极端反应引起。感染性休克属于脓毒症的一种严重情况,即脓毒症进一步加重造成机体器官功能损伤、细胞组织缺氧、有毒代谢产物蓄积,甚至多器官功能衰竭,最终导致机体出现以休克为主要症状的危重综合征[1], 致死率为30%~70%[2], 是重症监护室(ICU)患者死亡的主要原因之一。鉴于该疾病严重的不良预后和极快的进展速度,尽早通过有效的临床指标和血清生物标志物鉴别出高死亡风险患者并实施及时有效的治疗具有重要意义。中性粒细胞与淋巴细胞比值(NLR)是评估感染严重程度的一种简单且高效的指标,人体面对严重感染时会发生应激反应,可使体内中性粒细胞数量剧增和淋巴细胞数量下降,从而使NLR升高[3]。在脓毒症的病理生理学变化中,促炎和抗炎细胞因子的释放会导致凝血级联反应发生改变,使得机体抗凝血机制被严重抑制,并发生纤维蛋白溶解,而纤维蛋白溶解及纤维蛋白原消耗最终以弥散性血管内凝血(DIC)形式出现,可导致血小板破坏程度增大。平均血小板体积(MPV)升高可以反映脓毒症应激诱导血小板破坏后的代偿性骨髓生成情况[4], 而平均血小板体积与血小板计数比值(MPV/PLT)可评估感染严重程度。本研究探讨早期NLR和MPV/PLT对感染性休克患者预后的预测价值,以期为感染性休克的临床诊疗提供参考。
1. 对象与方法
1.1 研究对象
回顾性分析2019年10月—2022年10月在宜兴人民医院住院治疗的112例感染性休克患者的临床资料。以患者入住ICU首次诊断为感染性休克的时间为观察起点,以患者死亡时间或28 d时为观察终点,并根据28 d预后情况将患者分为存活组69例与死亡组43例。纳入标准: 符合2001年美国胸科医师学会/美国重症医学会(ACCP/SCCM)感染性休克诊断标准和《2016年脓毒症和感染性休克处理国际指南》[5], 即有明确的感染灶(血液、尿、脑脊液、伤口、呼吸道分泌物、其他体液等标本培养阳性)且快速序贯器官衰竭评分≥2分,使用足够液体补液及需要血管活性药物维持平均动脉压(MAP)≥65 mmHg, 血乳酸(Lac)>2 mmol/L者。排除标准: ①多发伤伴有活动性脏器出血者; ②有严重自身免疫性疾病者; ③恶性肿瘤终末期患者和使用多种靶向药物的肿瘤患者; ④近1周内使用过升高血小板药物或使用过粒细胞刺激因子药物者; ⑤妊娠期与哺乳期妇女。本研究相关过程、实验方法均符合中国医学伦理学相关法律要求,并经宜兴市人民医院医学伦理委员会审批(审批号2019-0915), 患者或其家属均知晓诊疗过程中的影像学检查、实验室检查相关结果及风险,并签署知情同意书。
1.2 研究方法
入院后收集患者基本病史和性别、年龄、既往病史等临床资料,记录患者入院时临床指标,包括休克指数(脉率/收缩压)、氧合指数、C反应蛋白(CRP)、降钙素原(PCT)、白细胞(WBC)、Lac、急性生理学与慢性健康状况评分系统Ⅱ(APACHEⅡ)评分、序贯器官衰竭评估(SOFA)评分、D-二聚体等,并记录患者入院24 h内NLR、MPV/PLT结果。检测仪器包括荧光免疫分析仪(型号FS-301, 购自广州万孚生物公司)、全自动生化分析仪(型号BC-7500, 购自Mindray迈瑞医疗公司)、全自动血气分析仪(型号GEM4000, 购自GEM公司); 检测试剂包括CRP乳胶增强免疫散射比浊法试剂(购自深圳迈瑞生物医疗有限公司)、PCT荧光免疫分析试剂(购自广州万孚生物技术股份有限公司)。
1.3 统计学分析
采用SPSS 20.0统计学软件分析数据,符合正态分布的计量资料以(x±s)描述, 2组间比较采用t检验,不符合正态分布的计量资料以[M(P25, P75)]表示, 2组间比较采用非参数Wilcoxon检验,计数资料以[n(%)]描述,比较采用χ2检验。绘制受试者工作特征(ROC)曲线,评估各项指标对感染性休克患者28 d死亡风险的预测价值; 采用多因素Logistic回归分析法分析感染性休克患者预后的危险因素; 采用Kaplan-Meier生存曲线分析不同NLR-MPV/PLT评分与总生存时间的相关性。P < 0.05表示差异有统计学意义。
2. 结果
2.1 临床资料比较
2组患者年龄、性别、既往病史(高血压病、糖尿病、冠心病)、休克指数、氧合指数、CRP比较,差异无统计学意义(P>0.05); 死亡组患者NLR、MPV/PLT、WBC、PCT、Lac、D-二聚体、APACHEⅡ评分、SOFA评分均高于存活组患者,差异有统计学意义(P < 0.05)。见表 1。
表 1 存活组与死亡组患者临床资料比较(x±s)[n(%)][M(P25, P75)]指标 存活组(n=69) 死亡组(n=43) χ2/t/z P 年龄/岁 69.13±13.83 71.56±13.76 -0.905 0.376 性别 男 36(52.17) 26(60.47) 0.737 0.391 女 33(47.83) 17(39.53) 既往病史 高血压病 48(69.57) 25(58.14) 1.524 0.217 糖尿病 21(30.43) 15(34.88) 0.240 0.624 冠心病 19(27.54) 10(23.26) 0.253 0.615 休克指数 1.34±0.18 1.38±0.21 -1.122 0.409 氧合指数 266.09±42.31 251.58±52.63 1.605 0.111 CRP/(mg/L) 95.43±17.19 100.50±16.63 -1.563 0.121 WBC/(×109/L) 12.09±5.97 15.29±7.03 -2.572 0.011 PCT/(ng/mL) 44.37±20.64 52.99±18.58 -2.233 0.028 Lac/(mmol/L) 5.24±2.55 6.81±2.77 -3.055 0.003 D-二聚体/(ng/mL) 1 460.00(777.00, 2 598.00) 3 491.00(1 646.00, 6 249.00) -3.309 0.001 NLR 10.95±6.06 15.04±4.53 -3.816 0.001 MPV/PLT 0.09±0.05 0.13±0.06 -3.578 0.001 APACHEⅡ评分/分 21.90±4.61 24.26±3.19 -2.942 0.004 SOFA评分/分 9.52±2.01 10.63±2.63 -2.512 0.013 CRP: C反应蛋白; WBC: 白细胞; PCT: 降钙素原; Lac: 乳酸; NLR: 中性粒细胞与淋巴细胞比值;
MPV/PLT: 平均血小板体积与血小板计数比值; APACHEⅡ: 急性生理学与慢性健康状况评分系统Ⅱ;
SOFA: 序贯器官衰竭评估。2.2 各项指标对感染性休克患者28 d死亡风险的预测价值
NLR、MPV/PLT、WBC、PCT、Lac、D-二聚体、APACHEⅡ评分、SOFA评分对感染性休克患者28 d死亡风险具有预测价值(P < 0.05), 年龄、休克指数、氧合指数、CRP则对感染性休克患者28 d死亡风险无预测价值(P>0.05)。NLR预测患者死亡风险的曲线下面积(AUC)为0.724, 当最佳截断值为12.49时,敏感度为74.4%, 特异度为68.1%; MPV/PLT预测患者死亡风险的AUC为0.731, 当最佳截断值为0.10时,敏感度为74.4%, 特异度为69.6%。见表 2、图 1。
表 2 各项指标对感染性休克患者28 d死亡风险的预测价值指标 AUC 敏感度/% 特异度/% 截断值 P 95%CI 年龄/岁 0.552 79.1 33.3 65.50 0.360 0.442~0.661 休克指数 0.546 14.0 97.1 1.65 0.411 0.435~0.658 氧合指数 0.407 11.6 94.2 320.50 0.099 0.295~0.519 CRP/(mg/L) 0.570 72.1 43.5 92.23 0.214 0.462~0.678 WBC/(×109/L) 0.626 65.1 60.9 13.05 0.026 0.519~0.732 PCT/(ng/mL) 0.631 93.0 33.3 29.00 0.020 0.528~0.734 Lac/(mmol/L) 0.685 65.1 71.0 6.15 0.001 0.583~0.786 D-二聚体/(ng/mL) 0.706 58.1 81.2 3 108.50 0.001 0.601~0.811 NLR 0.724 74.4 68.1 12.49 0.001 0.631~0.817 MPV/PLT 0.731 74.4 69.6 0.10 0.001 0.638~0.823 APACHEⅡ评分/分 0.665 60.5 66.7 23.50 0.003 0.564~0.765 SOFA评分/分 0.616 67.4 56.5 9.50 0.040 0.507~0.725 2.3 感染性休克患者28 d死亡风险的多因素Logistic回归分析
以WBC、PCT、Lac、D-二聚体、NLR、MPV/PLT、APACHEⅡ评分、SOFA评分这8项差异有统计学意义的指标作为自变量,以患者28 d是否死亡作为因变量,进行多因素Logistic回归分析。分析结果显示, NLR、MPV/PLT和WBC、PCT、Lac、D-二聚体均为感染性休克患者28 d死亡的独立影响因素(P < 0.05), 见表 3。
表 3 感染性休克患者28 d死亡风险的多因素Logistic回归分析因素 回归系数 标准误 Wald P OR 95%CI WBC 3.079 1.026 9.001 0.003 21.739 2.908~162.501 SOFA评分 0.686 0.640 1.150 0.284 1.986 0.567~6.957 APACHEⅡ评分 0.243 0.628 0.149 0.699 1.275 0.373~4.360 PCT 1.772 0.882 4.039 0.044 5.885 1.045~33.149 Lac 1.812 0.639 8.048 0.005 6.122 1.751~21.406 D-二聚体 1.366 0.654 4.360 0.037 3.921 1.087~14.137 NLR 1.781 0.627 8.083 0.004 5.938 1.739~20.274 MPV/PLT 1.989 0.644 9.531 0.002 7.308 2.067~25.833 2.4 预后分析
以NLR最佳截断值12.49和MPV/PLT最佳截断值0.10作为临界值,对NLR-MPV/PLT评分进行评估: NLR>12.49且MPV/PLT>0.10, NLR-MPV/PLT评分为2分; NLR>12.49或MPV/PLT>0.10, NLR-MPV/PLT评分为1分; NLR≤12.49且MPV/PLT≤0.10, NLR-MPV/PLT评分为0分。根据NLR-MPV/PLT评分将患者分为0分组、1分组、2分组, Kaplan-Meier生存曲线显示, 0分组、1分组、2分组感染性休克患者28 d累积生存率分别为88.2%、70.2%、19.4%, 差异有统计学意义(P < 0. 05), 见图 2。
3. 讨论
感染性休克属于脓毒症中最危重的一种类型,是被微生物感染的宿主出现应激反应失调而引起的严重器官功能障碍综合征,通常伴有严重的循环衰竭和细胞代谢功能障碍[6]。若未及时进行适当的治疗,感染性休克的致死率可高达60%[7]。在严重感染早期,为了保护宿主免受病原体侵袭,先天免疫细胞被显著激活以清除入侵病原体,若感染未得到适当控制,会导致逐级放大的先天免疫应答,释放大量促炎因子,进而损害自身器官,因此寻找易于获得、价格便宜且常规的实验室检查指标评估感染性休克患者疾病严重程度至关重要。
APACHE Ⅱ评分、SOFA评分目前已被广泛应用于ICU, 可较为准确地评估患者病情危重程度,反映感染性休克患者多个脏器功能衰竭程度,但其评估过程繁复,很多指标无法在疾病早期获取,难以在急诊抢救室及基层医院广泛应用,且可能增加感染性休克患者延误诊治的风险。近年来关于NRL和MPV/PLT应用于脓毒症的研究颇多。研究[8-9]发现,较高的NLR与脓毒症患者住院期间病死率和6个月病死率相关,且与多器官衰竭和脓毒症发展风险有关; LUBIS B等[10]发现, NLR与感染性休克患者死亡风险存在密切关联,并建议将NLR用作预测早期(第5天之前)和晚期(感染性休克发作后第5天或之后)病死率的指标; KIM C H等[11]发现,持续监测MPV可诊断脓毒症和感染性休克患者的死亡风险; AL HARBI G等[12]也发现,脓毒症患者MPV/PLT升高与病死率密切相关。本研究多因素Logistic回归分析结果显示, NLR和MPV/PLT均为感染性休克患者28 d死亡的独立影响因素; 当NLR取最佳截断值12.49时,其预测患者死亡风险的AUC为0.724, 敏感度为74.4%, 特异度为68.1%, 当MPV/PLT取最佳截断值0.10时,其预测患者死亡风险的AUC为0.731, 敏感度为74.4%, 特异度为69.6%, 提示NLR、MPV/PLT均对感染性休克患者死亡风险具有较高的预测价值。此外, Kaplan-Meier生存曲线显示,高NLR和高MPV/PLT患者的28 d死亡风险极高,这可能与感染性休克的病理生理机制相关。感染性休克时,机体免疫系统处于广泛激活状态[13], 中性粒细胞作为人体最“一线”的免疫细胞,在检测到微生物入侵后会迅速活化做出反应,导致迁移到循环中的中性粒细胞数量急剧增加[14], 中性粒细胞在先天免疫应答中发挥关键作用,包括通过吞噬直接杀死病原体、释放多种细胞因子和激活T细胞[15], 过程中还会释放大量促炎因子,但这种剧烈的免疫系统激活进程会导致组织损伤,继而引起多器官衰竭甚至死亡[16-17]。另外,大量抑制炎症的细胞因子被释放后介导机体免疫抑制,大量淋巴细胞被诱导凋亡[18], 且感染性休克时中性粒细胞会出现凋亡延迟,由骨髓产生的大量未成熟中性粒细胞被募集至循环中。MPV/PLT升高的主要原因是感染性休克时机体凝血系统被激活,抗凝血机制被抑制,纤维蛋白出现溶解,而纤维蛋白溶解和纤维蛋白原被消耗可引起DIC, 导致血小板破坏增加,同时脓毒症会导致患者体内毒素蓄积,直接抑制骨髓的造血功能,引起外周血中血小板数量急剧下降,血小板的大量消耗使得骨髓只能代偿性生成体积更大的血小板以增强其活性[19-20]。
综上所述,早期NLR、MPV/PLT对感染性休克患者的预后具有较高的预测价值,可作为有效而简便的评估指标用于急诊患者的早期诊断和后续治疗。本研究为单中心回顾性研究,部分因果关系难以确定,虽然调整了多因素Logistic回归模型中影响结果的指标,但患者群体的基线差异仍会影响研究结论,未来还需开展多中心、大样本量的临床研究进一步验证。
-
表 1 存活组与死亡组患者临床资料比较(x±s)[n(%)][M(P25, P75)]
指标 存活组(n=69) 死亡组(n=43) χ2/t/z P 年龄/岁 69.13±13.83 71.56±13.76 -0.905 0.376 性别 男 36(52.17) 26(60.47) 0.737 0.391 女 33(47.83) 17(39.53) 既往病史 高血压病 48(69.57) 25(58.14) 1.524 0.217 糖尿病 21(30.43) 15(34.88) 0.240 0.624 冠心病 19(27.54) 10(23.26) 0.253 0.615 休克指数 1.34±0.18 1.38±0.21 -1.122 0.409 氧合指数 266.09±42.31 251.58±52.63 1.605 0.111 CRP/(mg/L) 95.43±17.19 100.50±16.63 -1.563 0.121 WBC/(×109/L) 12.09±5.97 15.29±7.03 -2.572 0.011 PCT/(ng/mL) 44.37±20.64 52.99±18.58 -2.233 0.028 Lac/(mmol/L) 5.24±2.55 6.81±2.77 -3.055 0.003 D-二聚体/(ng/mL) 1 460.00(777.00, 2 598.00) 3 491.00(1 646.00, 6 249.00) -3.309 0.001 NLR 10.95±6.06 15.04±4.53 -3.816 0.001 MPV/PLT 0.09±0.05 0.13±0.06 -3.578 0.001 APACHEⅡ评分/分 21.90±4.61 24.26±3.19 -2.942 0.004 SOFA评分/分 9.52±2.01 10.63±2.63 -2.512 0.013 CRP: C反应蛋白; WBC: 白细胞; PCT: 降钙素原; Lac: 乳酸; NLR: 中性粒细胞与淋巴细胞比值;
MPV/PLT: 平均血小板体积与血小板计数比值; APACHEⅡ: 急性生理学与慢性健康状况评分系统Ⅱ;
SOFA: 序贯器官衰竭评估。表 2 各项指标对感染性休克患者28 d死亡风险的预测价值
指标 AUC 敏感度/% 特异度/% 截断值 P 95%CI 年龄/岁 0.552 79.1 33.3 65.50 0.360 0.442~0.661 休克指数 0.546 14.0 97.1 1.65 0.411 0.435~0.658 氧合指数 0.407 11.6 94.2 320.50 0.099 0.295~0.519 CRP/(mg/L) 0.570 72.1 43.5 92.23 0.214 0.462~0.678 WBC/(×109/L) 0.626 65.1 60.9 13.05 0.026 0.519~0.732 PCT/(ng/mL) 0.631 93.0 33.3 29.00 0.020 0.528~0.734 Lac/(mmol/L) 0.685 65.1 71.0 6.15 0.001 0.583~0.786 D-二聚体/(ng/mL) 0.706 58.1 81.2 3 108.50 0.001 0.601~0.811 NLR 0.724 74.4 68.1 12.49 0.001 0.631~0.817 MPV/PLT 0.731 74.4 69.6 0.10 0.001 0.638~0.823 APACHEⅡ评分/分 0.665 60.5 66.7 23.50 0.003 0.564~0.765 SOFA评分/分 0.616 67.4 56.5 9.50 0.040 0.507~0.725 表 3 感染性休克患者28 d死亡风险的多因素Logistic回归分析
因素 回归系数 标准误 Wald P OR 95%CI WBC 3.079 1.026 9.001 0.003 21.739 2.908~162.501 SOFA评分 0.686 0.640 1.150 0.284 1.986 0.567~6.957 APACHEⅡ评分 0.243 0.628 0.149 0.699 1.275 0.373~4.360 PCT 1.772 0.882 4.039 0.044 5.885 1.045~33.149 Lac 1.812 0.639 8.048 0.005 6.122 1.751~21.406 D-二聚体 1.366 0.654 4.360 0.037 3.921 1.087~14.137 NLR 1.781 0.627 8.083 0.004 5.938 1.739~20.274 MPV/PLT 1.989 0.644 9.531 0.002 7.308 2.067~25.833 -
[1] EVANS L, RHODES A, ALHAZZANI W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021[J]. Intensive Care Med, 2021, 47(11): 1181-1247. doi: 10.1007/s00134-021-06506-y
[2] CHIU C, LEGRAND M. Epidemiology of sepsis and septic shock[J]. Curr Opin Anaesthesiol, 2021, 34(2): 71-76. doi: 10.1097/ACO.0000000000000958
[3] HWANG S Y, SHIN T G, JO I J, et al. Neutrophil-to-lymphocyte ratio as a prognostic marker in critically-ill septic patients[J]. Am J Emerg Med, 2017, 35(2): 234-239. doi: 10.1016/j.ajem.2016.10.055
[4] 赵雪, 周坤鹏, 李鹏飞, 等. 早期平均血小板体积变化对脓毒症休克患者预后的预测价值[J]. 中华老年多器官疾病杂志, 2021, 20(5): 326-331. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLQG202105002.htm [5] 程宁宁, 樊尚荣. "2016年脓毒症和感染性休克处理国际指南"解读[J]. 中华产科急救电子杂志, 2017, 6(3): 180-187. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHCJ201703012.htm [6] CECCONI M, EVANS L, LEVY M, et al. Sepsis and septic shock[J]. The Lancet, 2018, 392(10141): 75-87. doi: 10.1016/S0140-6736(18)30696-2
[7] 商娜. 脓毒症流行病学研究[J]. 中国急救医学, 2013, 33(1): 8-12. https://cdmd.cnki.com.cn/Article/CDMD-90031-1016277067.htm [8] SARl R, KARAKURT Z, AY M, et al. Neutrophil to lymphocyte ratio as a predictor of treatment response and mortality in septic shock patients in the intensive care unit[J]. Turk J Med Sci, 2019, 49(5): 1336-1349. doi: 10.3906/sag-1901-105
[9] LIBERSKI P S, SZEWCZYK M, KRZYCH Ł J. Haemogram-derived indices for screening and prognostication in critically ill septic shock patients: a case-control study[J]. Diagnostics (Basel), 2020, 10(9): 638. doi: 10.3390/diagnostics10090638
[10] LUBIS B, HASBY A Y, PUTRA A O, et al. Hubungan Neutrophil-Lymphocyte Ratio (NLR) terhadap mortalitas pasien sepsis di unit perawatan intensif RSUP Haji Adam Malik Pada Tahun 2018[J]. Maj Anest Cri Care, 2021, 39(1): 12-18.
[11] KIM C H, KIM S J, LEE M J, et al. An increase in mean platelet volume from baseline is associated with mortality in patients with severe sepsis or septic shock[J]. PLoS One, 2015, 10(3): e0119437. doi: 10.1371/journal.pone.0119437
[12] AL HARBI G, CHAARI A. Platelets parameters in septic shock: clinical usefulness and prognostic value[J]. Blood Coagul Fibrinolysis, 2020, 31(7): 421-425. doi: 10.1097/MBC.0000000000000937
[13] 林怀德, 周稳兰, 朱蔚岗. 糖皮质激素治疗对感染性休克患者免疫炎症状态及预后的影响[J]. 临床与病理杂志, 2021, 41(11): 2543-2549. https://www.cnki.com.cn/Article/CJFDTOTAL-WYSB202111008.htm [14] STIEL L, MEZIANI F, HELMS J. Neutrophil activation during septic shock[J]. Shock, 2018, 49(4): 371-384. doi: 10.1097/SHK.0000000000000980
[15] TANG D L, WANG H C, BILLIAR T R, et al. Emerging mechanisms of immunocoagulation in sepsis and septic shock[J]. Trends Immunol, 2021, 42(6): 508-522. doi: 10.1016/j.it.2021.04.001
[16] GORECKI G, COCHIOR D, MOLDOVAN C, et al. Molecular mechanisms in septic shock (Review)[J]. Exp Ther Med, 2021, 22(4): 1161. doi: 10.3892/etm.2021.10595
[17] 庄雪明, 王诗波, 虞大为, 等. 脓毒性休克患者抗菌肽LL-37与降钙素原联合检测价值[J]. 实用临床医药杂志, 2021, 25(5): 96-100. doi: 10.7619/jcmp.20201396 [18] CARVELLI J, PIPEROGLOU C, BOURENNE J, et al. Imbalance of circulating innate lymphoid cell subpopulations in patients with septic shock[J]. Front Immunol, 2019, 10: 2179. doi: 10.3389/fimmu.2019.02179
[19] 许晓兰, 王海霞, 吴晓燕, 等. 早期感染性休克相关性血小板减少症的危险因素及对预后的影响[J]. 中华危重病急救医学, 2021, 33(8): 938-943. [20] VARDON-BOUNES F, GARCIA C, PITON A, et al. Evolution of platelet activation parameters during septic shock in intensive care unit[J]. Platelets, 2022, 33(6): 918-925.
-
期刊类型引用(2)
1. 史梦,蔡雪芹,李琼. NLR IL-6 CRP与重症肺炎合并感染性休克患者预后的关系研究. 河北医学. 2024(12): 2054-2059 .  百度学术
百度学术
2. 张诚实,徐明华,张青,冯契靓,王妮妮,陈荣荣,赵云峰. 平均血小板体积与血小板计数比值对老年呼吸衰竭患者预后的评估价值. 老年医学与保健. 2023(05): 964-968 .  百度学术
百度学术
其他类型引用(1)




 下载:
下载:

 苏公网安备 32100302010246号
苏公网安备 32100302010246号
