Application value of visual feedback guidance in breath holding training of breast cancer patients with radiotherapy
-
摘要:目的
观察左侧乳腺癌患者在深吸气屏气(DIBH)放射治疗中应用视觉反馈结合语音引导训练的临床效果。
方法将海宁市人民医院30例左侧乳腺癌患者随机分为视觉反馈组和无视觉反馈组,每组15例。视觉反馈组应用视觉反馈功能结合语音引导DIBH, 无视觉反馈组仅应用语音引导进行DIBH。2组患者定位前采用瑜伽呼吸训练的方式指导练习屏气。分析患者治疗时的呼吸曲线; 比较2组患者屏气水平的重复性和稳定性; 比较2组患者的屏气次数和治疗时间。
结果视觉反馈组的屏气平均幅度为(28.92±8.18) mm, 无视觉反馈组的屏气平均幅度为(24.68±10.64) mm; 视觉反馈组屏气幅度标准差均值为(1.17±0.81) mm, 无视觉反馈组为(1.94±0.94) mm; 2组屏气平均幅度、标准差均值比较,差异均有统计学意义(P < 0.05)。视觉反馈组、无视觉反馈组屏气期间最大幅度下降到最小幅度的差值分别为(1.89±1.41)、(4.56±2.80) mm, 差异有统计学意义(P < 0.01)。2组患者屏气时间比较,差异无统计学意义(P>0.05); 视觉反馈组屏气次数少于无视觉反馈组,差异有统计学意义(P < 0.05); 视觉反馈组治疗总时间短于无视觉反馈组,差异有统计学意义(P < 0.05)。
结论左侧乳腺癌患者通过应用视觉反馈结合语音引导DIBH的放射治疗方式,能够提高患者屏气水平的重复性和稳定性,值得临床推广。
Abstract:ObjectiveTo observe the clinical effect of visual feedback combined with voice-guided training in patients with deep inspiratory breath holding (DIBH) radiotherapy for left-sided breast cancer.
MethodsThirty patients with left-sided breast cancer in Haining City People′s Hospital were randomly divided into visual feedback group and no visual feedback group, with 15 cases in each group. The visual feedback group was conducted with visual feedback function combined with voice-guided DIBH, while the no visual feedback group was only conducted with voice-guided DIBH. Patients in both groups were instructed to hold their breath through yoga breathing training before positioning. Respiratory curve of the patients during treatment was analyzed; the repeatability and stability of breath holding levels were compared between two groups; the number of breath holding and treatment time were compared between the two groups.
ResultsThe mean amplitude of breath holding was (28.92±8.18) mm in the visual feedback group and (24.68±10.64) mm in the no visual feedback group; the mean standard deviation of breath holding amplitude was (1.17±0.81) mm in the visual feedback group and (1.94±0.94) mm in the no visual feedback group; there were significant differences in the mean amplitude of breath holding and standard deviation between the two groups (P < 0.05). The difference between the maximum amplitude and minimum amplitude in the breath holding period was (1.89±1.41) mm in the visual feedback group and (4.56±2.80) mm in the no visual feedback group, and there was a significant difference between two groups (P < 0.01). There was no significant difference in breath holding time between the two groups (P>0.05); the number of breath holding in the visual feedback group was significantly less than that in the no visual feedback group (P < 0.05); the total treatment time of the visual feedback group was significantly shorter than that of the no visual feedback group (P < 0.05).
ConclusionFor the patients with left-sided breast cancer, radiotherapy by visual feedback combined with voice-guided DIBH can improve the repeatability and stability of breath holding level, so it is worthy of clinical promotion.
-
目前全球乳腺癌呈高发趋势,其中左侧乳腺放疗心脏保护的问题越来越受到临床的重视,特别是对于心脏冠状动脉左降前支的剂量保护,因为此部位比较靠近心脏前壁,在进行切线野计划时,更容易受到射线的照射,造成放疗预后的长期心血管疾病风险增加。心脏所受放疗剂量与后期心脏、冠状动脉粥样硬化因素呈正相关[1-2]。目前,临床多应用深吸气屏气(DIBH)等措施来实施心、肺等危及器官的保护[3]。患者通过自主DIBH而使得肺部扩张,充分拉开心脏与胸壁的距离,让心脏远离计划靶区(PTV)的位置,避免受到辐射,从而降低远期冠心病的风险概率。在进行DIBH治疗的过程中,可以使用呼吸门控系统实时追踪患者的呼吸状态,以实现患者门控出束治疗。此过程需要关注患者的屏气质量,以保证每次屏气的重复性和稳定性[4]。临床医师实时监测患者屏气状态实施门控技术时,可以配合语音指导和视觉反馈训练的功能,让患者可以看到自己的呼吸状态、屏气的水平和需要屏气的位置,能够促进患者自主控制屏气的节奏以及时间。本研究探讨呼吸门控视觉反馈结合治疗前瑜伽式语音引导训练对左侧乳腺癌患者屏气门控治疗时屏气质量和屏气时间的影响,现将结果报告如下。
1. 资料与方法
1.1 一般资料
选取2021年7月—2022年12月海宁市人民医院收治的左侧乳腺保乳术后需要进行全乳腺放疗的患者为研究对象,年龄18~70岁,放射治疗靶区的位置均在患者的左侧乳腺部位,经过瑜伽式语音引导宣教训练后,患者能够熟练掌握DIBH的动作,保证每例患者屏气时间≥20 s, 并可以在此屏气时间基础上完成连续的重复屏气动作6次以上。共纳入患者30例,随机分为视觉反馈组和无视觉反馈组,每组15例。
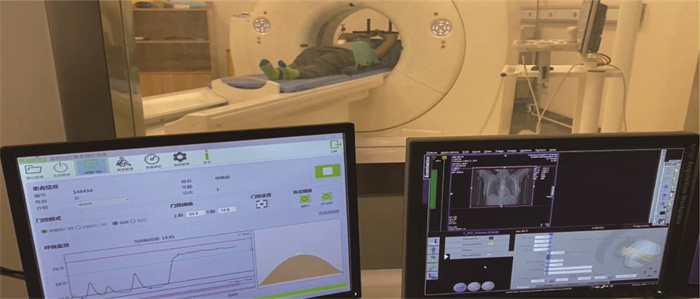
1.2 CT模拟定位
2组患者均实施仰卧位固定,选择左侧乳腺部位开窗膜片固定,将Orfit颈胸热塑膜在水箱中加热,变软之后覆盖于患者颈胸表面后进行卡扣固定,定型之后再拿剪刀分别在左侧乳腺的部位和剑突至肚脐需要放置追踪标记的位置剪出孔位,需要注意将患侧的乳腺完全暴露。开始扫描前先对患者进行屏气训练指导, 2组患者采用瑜伽的方式进行语音指引,进行屏气训练; 实施时先将热塑膜取下,让患者左手放在胸前,右手放在肚脐的开窗部位上,指导其深吸一口气,让患者感受到右手的抬升,然后屏住呼吸保持20 s以上,以语音“请您深吸一口气然后屏住”开始,以语音“请您放松呼吸”结束; 在模拟定位之前进行3~5次训练,直至患者能够掌握该种屏气的状态; 在进行扫描时,再将热塑膜扣上,期间采用广州科莱瑞迪呼吸门控系统基于双目立体红外相机追踪的技术原理,在患者肚脐暴露的位置放置追踪标记块,相机会实时追踪标记块运动以反映实时追踪患者的呼吸变化; 同时,采用呼吸门控系统的语音引导功能告知患者DIBH配合并维持稳定状态,同步在广州科莱瑞迪呼吸门控系统中设置好门控窗的位置,上、下限不超过5 mm, 见图 1。在深吸气的状态下进行CT扫描,西门子CT扫描条件为: 电压120 kV, 电流140 mA, 层厚3.0 mm。呼吸门控系统会自动计算出患者前5个呼吸周期的呼吸末平均位置作为呼吸基线,并将CT扫描期间设置的门控窗口位置记录在系统数据库内,在治疗的时候能直接调出。扫描结束后放置追踪标记块的位置需要画线标记。
1.3 治疗计划
2组患者治疗计划根据《乳腺癌放射治疗指南(中国医师协会2020版)》[5]相关标准拟定,左侧乳腺患者保乳术全乳腺(胸壁)临床靶区(CTV)包括内乳照射、胸壁和锁骨上淋巴引流区, PTV外扩5 mm。采用6 MV-X线进行调强放疗,要求95%剂量等效剂量包围PTV, 处方总剂量50 Gy, 分25次, 5周完成。
1.4 治疗实施
将2组患者以模拟定位相同体位对准激光灯标记线摆好体位,追踪标记块画线标记的地方重新摆放标记块,同时打开治疗室内呼吸门控系统摄像机,对患者的呼吸进行重新采集计算,此时呼吸门控系统会自动加载在CT端确定的呼吸基线以及门控窗口的位置。实施治疗前,为视觉反馈组的患者安装上门控系统配套的手机屏幕以显示视觉反馈的内容,其中屏气的幅度变化以柱状图升降表示; 视觉反馈组患者可以看到自身的屏气幅度并保持稳定在门控窗口内,当手机屏幕内的门控窗体显示绿色则说明屏气在治疗范围内,告知患者深吸气屏住之后稳定在此期间内,并结合语音引导告知患者吸气屏住和放松配合。无视觉反馈组患者仅使用语音引导功能告知患者吸气和放松配合。所有患者的呼吸曲线都会在治疗室内实时显示,以方便治疗师及时了解患者的呼吸状态变化。见图 2。
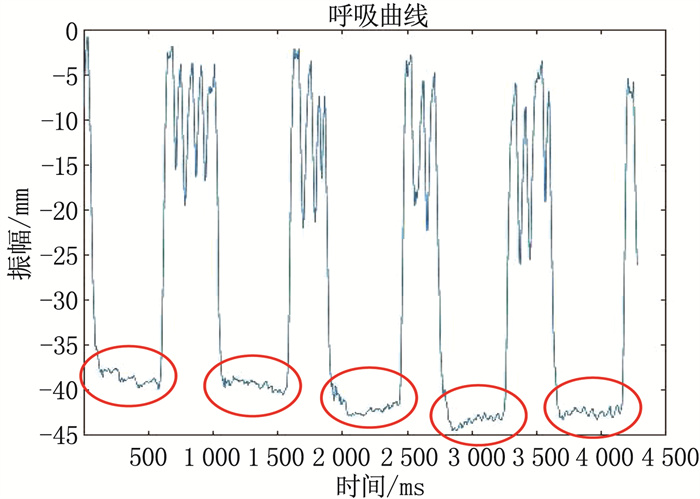
1.5 收集数据
屏气状态的重复性和稳定性: 为表示屏气状态的重复性,统计患者在治疗期间每次屏气从基线到屏住气幅度的一致性,利用患者记录的呼吸曲线,计算出每例患者每次屏气开始到屏气结束的幅度平均值和标准差,平均值表示患者每次屏气的平均位置变化情况,采用标准差的均值衡量屏气的重复性。为表示患者屏气的稳定性,统计患者每次屏气期间幅度位置发生的变化,计算每次屏气期间内的最大幅度和最小幅度的差值,以反映屏气的稳定性。见图 3。广州科莱瑞迪呼吸门控系统在监测患者的呼吸运动过程中会每间隔40 ms记录1次呼吸幅度变化,保存在呼吸曲线文件中,因此可以利用此文件记录的信息分析患者的屏气情况。另外,在呼吸曲线的文件上同时统计每例患者每次屏气的时间,统计每次分次治疗期间的每次屏气从开始屏气再到屏气结束的时间。
1.6 统计学分析
导出患者每次治疗的呼吸曲线文件数据,将患者的呼吸曲线采用Matlab软件绘制为曲线图形,然后在曲线图形中找到每次治疗重复屏气的位置,统计出开始屏气到结束屏气的平均幅度、屏气期间的幅度最大值和最小值以及屏气的时间。采用SPSS 16.0统计软件进行数据分析,收集参数呈正态分布,所有数据采用(x±s)表示,采用独立样本t检验方法分析组间数据的差异。P < 0.05为差异有统计学意义。
2. 结果
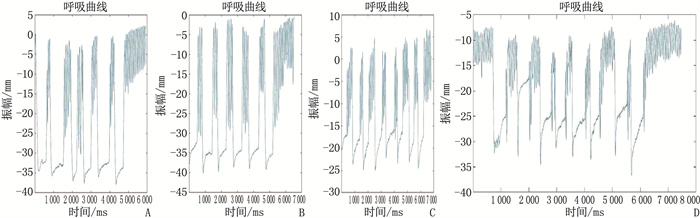
2.1 2组患者呼吸曲线变化
视觉反馈组患者共完成分次治疗375次,共完成屏气2 241次; 无视觉反馈组患者共完成分次治疗295次,共完成屏气2 318次。绘制并分析2组4例患者(每组2例)某次的呼吸曲线,结果显示应用手机视觉反馈的视觉反馈组在呼吸曲线的屏气阶段的形态上更具有重复、稳定的趋势,每次屏住位置能够相对保持,而且屏住后下降的幅度变化小于未使用视觉反馈的无视觉反馈组。见图 4。
2.2 2组患者屏气状态的重复性
视觉反馈组的屏气平均幅度为(28.92±8.18) mm, 无视觉反馈组的屏气平均幅度为(24.68±10.64) mm; 采用屏气平均幅度的标准差来衡量幅度的重复性,视觉反馈组标准差均值为(1.17±0.81) mm, 小于无视觉反馈组的(1.94±0.94) mm; 2组屏气平均幅度、标准差均值比较,差异均有统计学意义(P < 0.05)。
2.3 2组患者屏气状态稳定性比较
视觉反馈组、无视觉反馈组屏气期间最大幅度下降到最小幅度的差值分别为(1.89±1.41)、(4.56±2.80) mm, 差异有统计学意义(P < 0.01)。
2.4 2组患者屏气时间、屏气次数和治疗总时间的比较
2组患者屏气时间比较,差异无统计学意义(P>0.05); 视觉反馈组屏气次数少于无视觉反馈组,差异有统计学意义(P < 0.05); 视觉反馈组治疗总时间短于无视觉反馈组,差异有统计学意义(P < 0.05)。见表 1。
表 1 2组患者屏气时间、屏气次数及治疗总时间比较(x±s)指标 视觉反馈组(n=15) 无视觉反馈组(n=15) 屏气时间/s 17.33±4.35 16.22±4.72 屏气次数/次 6.20±0.86 8.33±2.47* 治疗总时间/s 255.22±53.46 311.53±74.04* 与视觉反馈组比较, *P < 0.05。 3. 讨论
随着复杂的左侧乳腺调强治疗计划在临床上的更多应用,临床医师需要更加关注呼吸运动带来靶区不稳定性的影响,呼吸运动会增加剂量传递的不确定性,一方面会导致乳腺靶区漏照的风险增加,另一方面也会增加临近心肺组织的剂量,造成远期心脏辐射相关疾病的风险增加。因此,需要进行呼吸运动管理来保证放疗的精确性,其中DIBH的呼吸运动管理策略是临床放疗常用的一种技术手段[6]。DIBH技术在乳腺癌术后辅助放疗中不仅可以预防呼吸运动造成的靶区漏照,还可以降低心脏、冠状动脉左降前支、同侧肺组织等危及器官的辐射剂量[7]。
患者在放疗过程中会因多种因素而影响DIBH的质量,例如自身因素、认知情况以及反应能力都能够对DIBH技术的实施造成影响。研究[8]表明,需要进行DIBH放疗的患者产生的放疗相关焦虑和压力反应较普通疗程的患者更为强烈,这是因为患者需要进行严格的长时间屏气,会因不习惯而造成情绪紧张。同时,屏气需要胸部及腹部肌肉的相互协调,才能实现长时间、稳定屏气,在短时间内要快速反应并配合治疗,这对患者的反应能力要求较高[9]。因此需要对实施DIBH患者进行必要的呼吸相关训练,以适应屏气的状态,提高治疗期间的重复性和治疗效率。国外研究[10]报道,采用视觉反馈的呼吸训练在DIBH放疗方面具有很大的应用潜力。患者通过自身的呼吸信号视觉反馈提高了每次屏气的水平以及稳定性,这对于放疗靶区的精准照射以及周围危及器官的保护具有重要意义[11]。
本研究对30例左侧乳腺癌患者应用广州科莱瑞迪呼吸门控系统中的呼吸视觉反馈功能,并结合语音引导训练方式实现DIBH放疗。在患者定位前的训练中,采用瑜伽呼吸训练可让患者快速掌握长时间屏气的技巧,结合视觉反馈的机制可让患者体验成功感,提高治疗的效果。本研究结果显示,使用视觉反馈患者的屏气质量和屏气次数显著改善,屏气重复性和稳定性显著高于未使用者,每次屏气的幅度变化显著小于未使用者,说明患者治疗前的训练有助于有效掌握屏气的技巧,利用视觉反馈能看到自身呼吸信号的变化,每次能够屏气在相同位置,始终保持在门控窗口范围内,从而大大提高了DIBH放疗中的呼吸重复性和稳定性。SWAMIDAS J等[12]研究采用视频护目镜连通呼吸门控软件,患者视觉反馈引导的DIBH较单纯音频引导的DIBH具有更好的可重复性屏气水平。YAMAUCHI R等[13]通过光学体表追踪方式追踪患者的呼吸运动,应用DIBH技术行呼吸视觉反馈后, 95%的患者屏气的重复性得到改善。
本研究中,实施呼吸训练患者均给予瑜伽呼吸训练,但部分患者在实施治疗时因边看手机屏幕边治疗而更易产生紧张感,未来或可尝试治疗室环境、居家训练等模式来优化患者的屏气训练。在未使用视觉反馈功能前,本科对左侧乳腺癌患者采用的是单纯语音引导下自愿DIBH进行门控治疗; 当患者使用视觉反馈进行呼吸控制后,对临床的DIBH工作有很大的帮助,与单纯的语音引导DIBH相比,患者可以通过手机视觉反馈的屏幕来调节自己的屏气水平,能够维持相对稳定的屏气状态,将屏气的幅度控制在相对一致的范围内。本研究2组患者屏气时间的差异无统计学意义(P>0.05), 分析原因可能是本科采用的是治疗师手动控制语音引导的播报,患者听到指令后配合屏气和放松,在屏气的时间上会受到治疗师人为控制的影响,故屏气时间会受其他的误差因素影响。此外,使用视觉反馈后患者能够在单次或者2次的屏气周期完成1个射野的照射,减少了屏气次数,缩短了整个治疗的时间。有研究[14]通过应用视觉反馈统计患者的憋气次数显著减少,在4~5个屏气周期内可以完成治疗,使用视觉反馈的治疗时间较未使用视觉反馈缩短了245 s。DOLEZEL M等[15]证实了在DIBH中采用视听导航可以显著缩短治疗时间。本研究中,使用视觉反馈患者的平均治疗时间较未使用视觉反馈者缩短,屏气次数减少,说明应用视觉反馈的患者可根据自身的呼吸状态来更好地控制屏气状态,具有更好的耐受性。
-
表 1 2组患者屏气时间、屏气次数及治疗总时间比较(x±s)
指标 视觉反馈组(n=15) 无视觉反馈组(n=15) 屏气时间/s 17.33±4.35 16.22±4.72 屏气次数/次 6.20±0.86 8.33±2.47* 治疗总时间/s 255.22±53.46 311.53±74.04* 与视觉反馈组比较, *P < 0.05。 -
[1] FALCO M, MASOJC B, MACAŁA A, et al. Deep inspiration breath hold reduces the mean heart dose in left breast cancer radiotherapy[J]. Radiol Oncol, 2021, 55(2): 212-220. doi: 10.2478/raon-2021-0008
[2] PIROTH M D, BAUMANN R, BUDACH W, et al. Heart toxicity from breast cancer radiotherapy: current findings, assessment, and prevention[J]. Strahlenther Onkol, 2019, 195(1): 1-12. doi: 10.1007/s00066-018-1378-z
[3] CERVIÑO L I, GUPTA S, ROSE M A, et al. Using surface imaging and visual coaching to improve the reproducibility and stability of deep-inspiration breath hold for left-breast-cancer radiotherapy[J]. Phys Med Biol, 2009, 54(22): 6853-6865. doi: 10.1088/0031-9155/54/22/007
[4] MAYR N A, BORM K J, KALET A M, et al. Reducing cardiac radiation dose from breast cancer radiation therapy with breath hold training and cognitive behavioral therapy[J]. Top Magn Reson Imaging, 2020, 29(3): 135-148. doi: 10.1097/RMR.0000000000000241
[5] 中国医师协会放射肿瘤治疗医师分会, 李晔雄, 王玉, 等. 乳腺癌放射治疗指南(中国医师协会2020版)[J]. 中华放射肿瘤学杂志, 2021, 30(4): 321-342. doi: 10.3760/cma.j.cn113030-20210107-00010 [6] 胡皓, 李敏儿, 肖光莉. 深吸气屏气技术在左侧乳腺癌术后放疗中的应用(附41例)[J]. 现代肿瘤医学, 2020, 28(13): 2318-2322. doi: 10.3969/j.issn.1672-4992.2020.13.030 [7] MUROFUSHI K N, NAKAJIMA M, TOMITA T, et al. Impact of visual feedback on dose-volume histograms for organs at risk in postoperative radiotherapy with deep inspiration breath-holding for patients treated with breast-conserving therapy: a planning study[J]. Breast Cancer, 2018, 25(6): 656-662. doi: 10.1007/s12282-018-0870-8
[8] BRAY F, FERLAY J, SOERJOMATARAM I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2018, 68(6): 394-424. doi: 10.3322/caac.21492
[9] KALET A M, KIM A, HIPPE D S, et al. The dosimetric benefit of in-advance respiratory training for deep inspiration breath holding is realized during daily treatment in left breast radiotherapy: a comparative retrospective study of serial surface motion tracking[J]. J Med Imaging Radiat Oncol, 2021, 65(3): 354-364. doi: 10.1111/1754-9485.13181
[10] STOCK M, KONTRISOVA K, DIECKMANN K, et al. Development and application of a real-time monitoring and feedback system for deep inspiration breath hold based on external marker tracking[J]. Med Phys, 2006, 33(8): 2868-2877. doi: 10.1118/1.2219775
[11] SCHÖNECKER S, WALTER F, FREISLEDERER P, et al. Treatment planning and evaluation of gated radiotherapy in left-sided breast cancer patients using the CatalystTM/SentinelTM system for deep inspiration breath-hold (DIBH)[J]. Radiat Oncol, 2016, 11(1): 143. doi: 10.1186/s13014-016-0716-5
[12] SWAMIDAS J, ROSE J, CHOPRA S, et al. Implementation of a visual feedback system for motion management during radiation therapy[J]. J Cancer Res Ther, 2021, 17(1): 148-151. doi: 10.4103/jcrt.JCRT_95_18
[13] YAMAUCHI R, MIZUNO N, ITAZAWA T, et al. Assessment of visual feedback system for reproducibility of voluntary deep inspiration breath hold in left-sided breast radiotherapy[J]. J Med Imaging Radiat Sci, 2021, 52(4): 544-551. doi: 10.1016/j.jmir.2021.08.018
[14] 李谭谭, 张江鹄, 王淑莲, 等. 基于视觉反馈的呼吸训练模块在左侧乳腺癌深吸气屏气放疗中的应用[J]. 中华放射肿瘤学杂志, 2021, 30(3): 258-261. [15] DOLEZEL M, ODRAZKA K, VANASEK J, et al. Audio-visual navigation reduces treatment time in deep-inspiration breath hold radiotherapy[J]. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub, 2020, 164(4): 461-466. doi: 10.5507/bp.2019.051




 下载:
下载:

 苏公网安备 32100302010246号
苏公网安备 32100302010246号