Establishment of early high-risk disease prediction model for preschool children with acute upper respiratory tract infection and febrile convulsion
-
摘要:目的
分析学龄前急性上呼吸道感染高热惊厥患儿早期病情变化的影响因素,建立其高危病情的预测模型。
方法采取便利抽样的方法选取2019年1月—2021年6月本院儿科收治学龄前急性上呼吸道感染高热后发生惊厥的患儿384例为研究对象,基于儿童早期预警评分系统(PEWS)将患儿分为低危组294例、中危组65例和高危组25例。采用单因素比较和多元有序Logistic回归分析确定学龄前急性上呼吸道感染高热惊厥患儿早期病情变化的影响因素; 采用二元Logistic回归分析确定学龄前急性上呼吸道感染高热惊厥患儿早期病情高危的影响因素; 采用受试者工作特征(ROC)曲线分析早期病情高危影响因素的预测效能。基于二元Logistic回归结果绘制高危病情变化列线图。
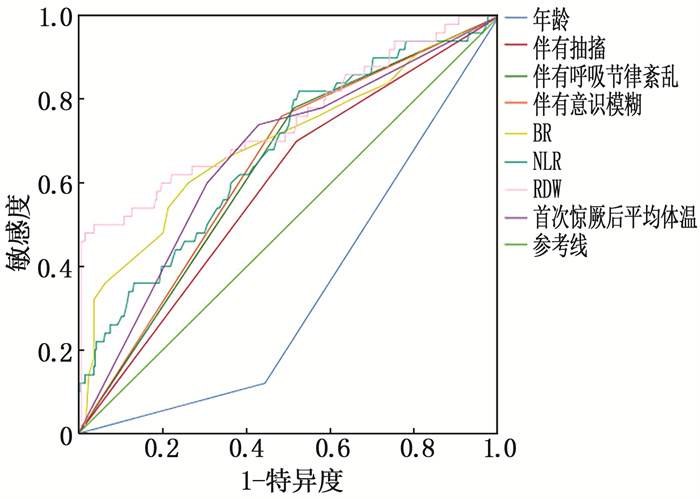
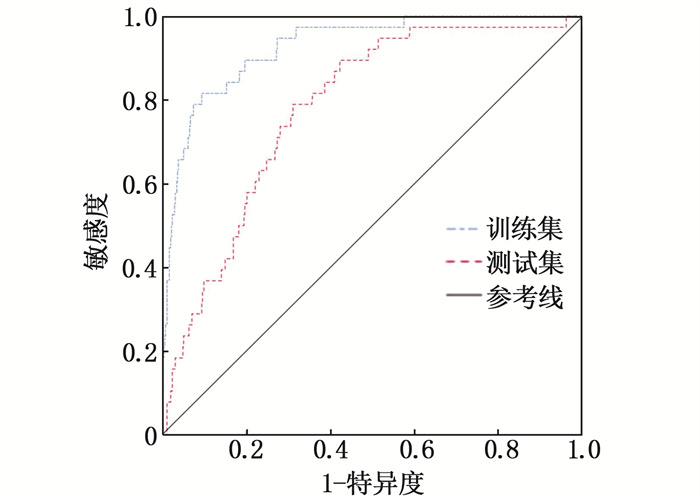
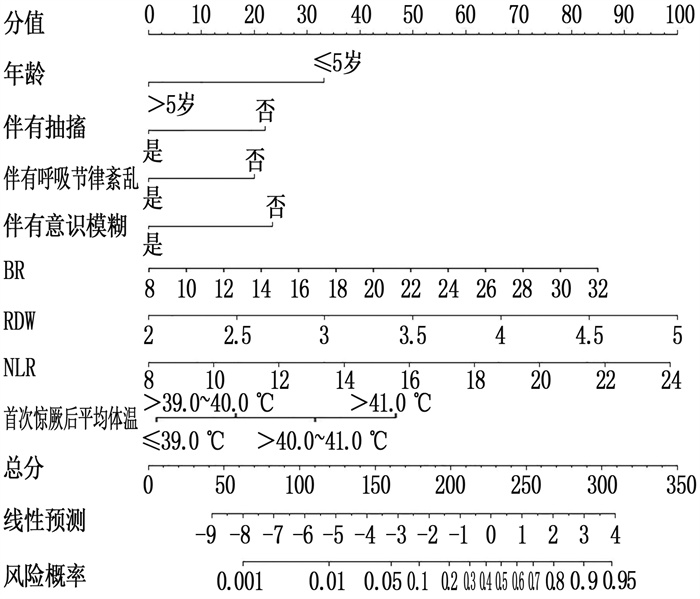
结果多元有序Logistic回归分析结果发现,年龄、伴有抽搐、伴有呼吸节律紊乱、伴有意识模糊、呼吸频率(BR)、中性粒细胞与淋巴细胞的比值(NLR)、红细胞分布宽度(RDW)、首次惊厥后平均体温均是学龄前急性上呼吸道感染高热惊厥患儿早期病情变化的影响因素(P < 0.05)。二元Logistic回归分析结果发现,年龄(>5岁)、伴有抽搐、伴有呼吸节律紊乱、伴有意识模糊、BR、NLR、RDW、首次惊厥后平均体温高(>40.0~41.0 ℃和>39.0~40.0 ℃)均是学龄前急性上呼吸道感染高热惊厥患儿早期病情的高危影响因素(P < 0.05)。ROC曲线显示,年龄(>5岁)、伴有抽搐、伴有呼吸节律紊乱、伴有意识模糊、BR、RDW、NLR和首次惊厥后平均体温高对高热惊厥患儿早期高危病情预测效能较好(P < 0.05)。列线图分析显示,学龄前急性上呼吸道感染高热惊厥患儿高危病情预测模型预测得分为85~287分,可有效评估0.1%~95.0%的风险概率。
结论学龄前急性上呼吸道感染高热惊厥患儿早期病情变化可能受到伴有抽搐、伴有呼吸节律紊乱、伴有意识模糊、BR、NLR、RDW、首次惊厥后平均体温等因素影响,应针对学龄前急性上呼吸道感染高热惊厥患儿采取相应干预措施以预防其早期病情恶化。
Abstract:ObjectiveTo analyze the influencing factors of early condition changes in preschool children with acute upper respiratory tract infection and febrile convulsion, and to establish a high-risk disease prediction model.
MethodsA total of 384 preschool children with convulsion after high fever of acute upper respiratory tract infection in our hospital from January 2019 to June 2021 were selected as research objects. Based on the early warning scoring system (PEWS), the children were divided into low-risk group(n=294), medium-risk group(n=65) and high-risk group(n=25). Univariate comparison and multiple ordered Logistic regression analysis were used to determine the influencing factors of early condition of preschool children with acute upper respiratory tract infection and febrile convulsion, binary Logistic regression analysis was used to determine the high-risk influencing factors of early condition of preschool children with acute upper respiratory tract infection and febrile convulsion; ROC curve was used to analyze the prediction efficiency of high-risk influencing factors of early condition. The nomogram of high-risk disease changes was drawn based on the results of binary Logsitic regression.
ResultsMultiple ordered Logistic regression analysis showed that age, convulsions, disordered respiratory rhythm, blurred consciousness, Br, NLR, RDW and average body temperature after the first convulsion were the influencing factors of the changes of early conditions of preschool children with febrile convulsion caused by acute upper respiratory tract infection (P < 0.05). Binary Logistic regression analysis showed that age over five years old, convulsion, respiratory rhythm disorder, confusion of consciousness, Br, NLR, RDW and average body temperature(>40.0 to 41.0 ℃ and >39.0 to 40.0 ℃) after the first convulsion were the high-risk factors of early condition in preschool children with acute upper respiratory tract infection and febrile convulsion (P < 0.05). ROC curve analysis showed that age (>5 yeas old), convulsion, respiratory rhythm disorder, confusion of consciousness, breath rate (BR), neutrophil to lymphocyte ratio (RDW), red cell distribution width (NLR) and high average temperature of the body after the first convulsion had better predictive effects on the early high-risk changes of children with febrile convulsion (P < 0.05). The nomogram showed the predicted score of the high-risk condition prediction model for preschool children with acute upper respiratory tract infection and high fever convulsion was from 85 to 287 points, which can effectively evaluate the risk rate from 0.1% to 95.0%.
ConclusionThe early condition changes of preschool children with acute upper respiratory tract infection and febrile convulsion may be affected by factors such as convulsion, respiratory rhythm disorder, complicating with confusion of consciousness, BR, NLR, RDW and average body temperature after the first convulsion. Corresponding intervention measures should be taken for preschool children with acute upper respiratory tract infection and febrile convulsion to prevent their early condition deterioration.
-
耳石症又称良性阵发性位置性眩晕(BPPV), 属于外周性前庭疾病之一,主要由头位改变诱发,占全部眩晕的17%~22%[1]。耳石症患者以突然的、短暂的眩晕为主要症状,常存在不同程度的恶心、呕吐等自主神经症状。耳石复位是临床治疗耳石症的主要方式,可迅速缓解临床症状,但仍有部分患者存在颈部僵硬、头晕等残余症状[2]。残余头晕发生率为34%~61%, 患者自诉常有漂浮感、头晕、平衡不稳感等症状与焦虑、抑郁等负性情绪,严重影响正常生活与工作[3-4]。耳石症复位后残余头晕的治疗方法较多,现代医学以倍他司汀片等西药治疗为主,可在一定程度上改善脑部微循环,减轻头晕及前庭症状,但长期应用单一药物会引发药物副作用,整体疗效欠佳[5]。中医疗法安全、简便,近年来在治疗耳石症复位后残余头晕中显示出独特的优势。本研究对98例耳石症复位后残余头晕患者实施倍他司汀联合三联疗法(复合手法、经颅磁刺激及特定体位)治疗,现将结果报告如下。
1. 资料与方法
1.1 一般资料
前瞻性选择2022年1—12月就诊于本院的196例耳石症复位后残余头晕患者为研究对象,其中男104例,女92例; 年龄23~68岁,平均(44.16±4.25)岁; 体质量指数19.41~26.36 kg/m2, 平均(22.76±2.51) kg/m2; 病程1~5 d, 平均(3.29±0.75) d; 病变在左侧104例,右侧92例; 受累半规管为后半规管136例,水平半规管48例,前半规管12例。本研究获得院医学伦理委员会批准[院科伦审: (2021)伦审第(1022)号]。
纳入标准: ①符合《良性阵发性位置性眩晕诊断和治疗指南(2017)》[6]中耳石症西医诊断标准者; ②经手法复位后达到复位成功标准(即位置性眩晕和/或位置性眼震减轻,但未消失; 位置性眩晕消失,滚转试验阴性或Dix-Hallpike阴性)者; ③复位后有残余头晕症状者; ④既往无眩晕病史者; ⑤年龄18~75岁者; ⑥手法复位成功后5 d内发病者; ⑦既往无焦虑症、抑郁症、痴呆及颅脑损伤等疾病者; ⑧自愿签署知情同意书者。排除标准: ①伴有中枢神经系统病变、脑部炎症、眼科疾病或颈椎病等影响头晕的疾病者; ②存在控制不良的高血压,复合管、继发性耳石症,梅尼埃、前庭神经炎、前庭性偏头痛、中枢性位置性眩晕等疾病者; ③存在经颅磁刺激治疗禁忌证(包括有耳蜗植入物、植入心脏起搏器、颅内置入金属物等)者; ④近期接受前庭抑制剂、抗焦虑抑郁等药物治疗者; ⑤哺乳期或妊娠期女性; ⑥合并精神疾病、认知功能障碍者。
1.2 方法
将196例患者随机分为对照组和实验组,每组98例。对照组接受甲磺酸倍他司汀片治疗,即口服甲磺酸倍他司汀片[国药准字H20040130, 规格6 mg/片,卫材(中国)药业有限公司], 6 mg/次, 3次/d, 以7 d为1个疗程,共治疗2个疗程。实验组接受甲磺酸倍他司汀片(用法、用量与对照组一致)联合三联疗法。三联疗法: (1) 复合手法治疗。①开天门手法。点按印堂穴30下,由印堂至百会线为1线,旁开1.5寸和3寸为2线和3线,分别依次由下往上轻揉和点按5次,重复3次。用双侧拇指指腹分推100次前额,按顺时针、逆时针方向按揉50次太阳穴,用手指腹轻叩患者前额、头部约50下。太阳经梳理,双手手指指端交替梳推头额50下。②颈部手法。取俯卧位,操作者弹拨患者头半棘肌、枕下小肌群、斜方肌、肩胛提肌等颈部肌肉,放松3~5 min。采用低头摇正法纠正C3~C6小关节紊乱,利用仰头摇正法纠正寰枢关节、寰枕关节紊乱。取仰卧位,纵向快速牵伸患者颈部。上述操作1次/d, 以7 d为1个疗程,共治疗2个疗程。(2) 经颅磁刺激。仪器选用深圳市英智科技有限公司生产的S-30型号经颅磁刺激仪,操作前测定患者阈值。嘱患者取仰卧位,将圆形线圈中心置于患者晕听区(双耳尖上1.5 cm, 向前向后各引2.0 cm的水平线),刺激强度为80%静息运动阈值(RMT), 频率为1 Hz, 刺激3次,左右刺激时间各10 min, 每次刺激间隔时间为5 s, 1次/d, 以7 d为1个疗程,共治疗2个疗程。(3) 特定体位。根据患者耳石评估结果,确定患侧。提醒患者躺下或坐起时选择健侧,睡觉时健侧卧位,体位保持时间为7 d。
1.3 评价指标
1.3.1 各个量表评分
① 眩晕障碍量表(DHI)共25个项目3个维度(情感、躯体、功能),每项0、2或4分,最高分为100分,分值高提示眩晕障碍程度重。②前庭症状指数量表(VSI)共包含6种前庭症状,每种症状0~10分,满分60分,前庭症状严重程度与分值呈正相关。③视觉模拟评分法(VAS)总分0~10分,分别代表无痛至难以忍受的剧烈疼痛。④汉密尔顿焦虑量表(HAMA)共14个条目,每个条目0~4分,满分56分,焦虑严重程度与分值呈正相关。⑤活动平衡信心量表(ABC)用于测量个体在特定日常活动中的平衡信心程度,有16项任务,包括日常生活中的基本任务(如在屋子周围行走、在室内取物、上下楼梯、扫地等)与在社区中难度较大的任务(如在拥挤的商场里穿行、上下扶梯、在室外冰面行走等),分值0~100分,分值高表示活动平衡信心高。5个量表评估时间均为治疗前和治疗2个疗程结束后。
1.3.2 残余头晕持续时间与疗效
记录患者残余头晕持续时间,并参考《中药新药临床研究指导原则》[7]判定疗效,分为临床缓解、显效、进步、无效。治疗后DHI综合疗效指数≥95%, 疼痛消失为临床缓解; 治疗后DHI综合疗效指数为70%~ < 95%, 疼痛大部分缓解为显效; 治疗后DHI综合疗效指数为30%~ < 70%, 疼痛部分减轻为进步; 治疗后DHI综合疗效指数 < 30%, 疼痛无好转或病情加重为无效。
1.3.3 皮肤交感反应(SSR)检测
于治疗前、疗程结束后让患者在安静房间内自然平躺,利用肌电图/诱发电位仪(型号为M-800D, 珠海市迈康科技有限公司)测定患者SSR波幅、SSR潜伏期。
1.3.4 大脑流速
于治疗前、疗程结束后采用便携式彩色多普勒超声系统(型号为Clover 50, 深圳华声医疗技术股份有限公司)测定患者大脑椎动脉(VA)、基底动脉(BA)的血液平均流速(Vm)值。
1.4 统计学方法
采用SPSS 24.0软件进行统计学分析,计量资料以($\mathop x\limits^ - $±s)表示,比较采用t检验; 计数资料以[n(%)]表示,比较采用χ2检验。P < 0.05为差异有统计学意义。
2. 结果
2.1 2组患者一般资料比较
2组性别、年龄、体质量指数、病程、病变侧别、受累半规管等一般资料比较,差异无统计学意义(P>0.05)。见表 1。
表 1 2组一般资料比较($\mathop x\limits^ - $±s)一般资料 分类 对照组(n=98) 实验组(n=98) 性别 男 54 50 女 44 48 年龄/岁 44.72±4.16 43.85±4.35 体质量指数/(kg/m2) 23.16±2.48 22.81±2.34 病程/d 3.35±0.84 3.29±0.74 病变侧别 左侧 50 54 右侧 48 44 受累半规管 后半规管 70 66 水平半规管 26 22 前半规管 2 10 2.2 2组残余头晕持续时间与疗效比较
实验组残余头晕持续时间为(10.25±3.74) d, 短于对照组的(15.26±2.98) d, 差异有统计学意义(t=10.371, P < 0.001); 实验组治疗总有效率为93.88%, 高于对照组的79.59%, 差异有统计学意义(P < 0.05)。见表 2。
表 2 2组临床疗效比较[n(%)]组别 n 临床缓解 显效 进步 无效 总有效 对照组 98 6(6.12) 26(26.53) 46(46.94) 20(20.41) 78(79.59) 实验组 98 16(16.33) 28(28.57) 48(48.98) 6(6.12) 92(93.88)* 与对照组比较, *P<0.05。 2.3 2组DHI评分比较
实验组疗程结束后DHI的3个维度评分均低于对照组,差异有统计学意义(P < 0.05)。见表 3。
表 3 2组DHI评分比较($\mathop x\limits^ - $±s)分 组别 n 情感评分 躯体评分 功能评分 治疗前 疗程结束后 治疗前 疗程结束后 治疗前 疗程结束后 对照组 98 23.26±3.84 15.35±2.65* 21.05±2.65 16.11±2.85* 20.35±3.58 15.56±2.02* 实验组 98 23.16±4.11 10.46±2.38*# 20.74±2.46 10.32±2.41*# 20.42±4.28 10.49±3.32*# DHI: 眩晕障碍量表。与治疗前比较, *P < 0.05; 与对照组比较, #P < 0.05。 2.4 2组VAS、ABC、HAMA及VSI评分比较
实验组疗程结束后VAS、HAMA、VSI评分低于对照组, ABC评分高于对照组,差异有统计学意义(P < 0.05)。见表 4。
表 4 2组VAS、ABC、HAMA及VSI评分比较($\mathop x\limits^ - $±s)分 组别 VAS评分 ABC评分 HAMA评分 VSI评分 治疗前 疗程结束后 治疗前 疗程结束后 治疗前 疗程结束后 治疗前 疗程结束后 对照组(n=98) 6.43±1.52 3.58±1.06* 40.56±7.98 70.25±8.45* 22.56±4.25 14.35±3.65* 30.15±3.59 17.46±4.26* 实验组(n=98) 6.33±1.45 1.78±0.89*# 41.28±7.98 87.46±10.05*# 22.74±4.03 8.46±1.64*# 30.58±4.25 12.03±3.58*# VAS: 视觉模拟评分法; ABC: 活动平衡信心量表; HAMA: 汉密尔顿焦虑量表; VSI: 前庭症状指数量表。
与治疗前比较, *P < 0.05; 与对照组比较, #P < 0.05。2.5 2组SSR检测结果比较
实验组疗程结束后SSR波幅值低于对照组, SSR潜伏期值高于对照组,差异有统计学意义(P < 0.05)。见表 5。
表 5 2组SSR检测结果比较($\mathop x\limits^ - $±s)组别 n SSR波幅值/mV SSR潜伏期值/ms 治疗前 疗程结束后 治疗前 疗程结束后 对照组 98 2.11±0.24 1.67±0.22* 1.49±0.15 1.64±0.27* 实验组 98 2.05±0.26 1.37±0.28*# 1.47±0.17 1.99±0.31*# SSR: 皮肤交感反应。与治疗前比较, *P < 0.05; 与对照组比较, #P < 0.05。 2.6 2组大脑流速比较
实验组疗程结束后VA、BA的Vm值高于对照组,差异有统计学意义(P < 0.05)。见表 6。
表 6 2组VA、BA的Vm值比较($\mathop x\limits^ - $±s)cm/s 组别 n VA BA 治疗前 疗程结束后 治疗前 疗程结束后 对照组 98 17.46±3.65 29.65±5.52* 21.46±4.98 28.46±5.63* 实验组 98 18.21±3.94 35.48±5.85*# 20.48±4.86 34.98±5.74*# VA: 大脑椎动脉; BA: 基底动脉; Vm: 血液平均流速。与治疗前比较, *P < 0.05; 与对照组比较, #P < 0.05。 3. 讨论
耳石症复位后残余头晕的发病原因复杂,目前主流学说认为与椭圆囊功能障碍、交感神经失调、耳石脱落至半规管损伤前庭功能等有关[8-9]。倍他司汀属于一种选择性H1受体激动剂,可抑制前庭受体细胞作用,增加内耳血流量与脑、周围迷路内组胺释放,增强前庭代偿功能,扩张内耳毛细血管,从而减轻甚至消除头晕症状[10-11]。WU P X等[12]在一项随机单盲对照试验中报道,倍他司汀可减轻耳石症复位后残余头晕患者头晕症状,提高平衡能力与日常生活活动能力。谢涛等[13]研究报道,倍他司汀可缩短耳石症患者管石复位成功后残余头晕的持续时间,降低头疼程度,减轻抑郁、焦虑程度。但仍有部分学者提出不一致的看法,ACAR B等[14]研究指出,倍他司汀、曲美他嗪、银杏叶提取物均无法有效减轻患者手法复位后残余头晕症状。因此,探讨一种高效、安全的联合治疗方案尤为关键。
中医学无耳石症复位后残余头晕的病名,根据其临床症状、体征归属于“眩晕”范畴。中医学对眩晕的认知历史悠久,早在《素问·至真要大论》中便记载“厥阴之胜,耳鸣头眩,愦愦欲吐,胃鬲如寒”[15-16]。本病病位在耳,反映在脑,且与肝、肾、脾密切相关。其病因病机分为内伤、外感2个方面,本虚标实,实者因风、火、痰、瘀扰乱而清窍失宁,虚者因气、血、精不足而髓海失养。本研究基于上述中西医理论机制,结合中医、现代康复、西医治疗,发现与对照组比较,实验组残余头晕持续时间短, DHI、VAS、HAMA、VSI评分低, ABC评分与VA、BA的Vm值高,表明三联疗法联合倍他司汀治疗耳石症复位后残余头晕疗效确切,可减轻眩晕、前庭症状,提高活动平衡信心,降低焦虑程度,改善大脑血流循环。分析原因为: ①头为诸阳之会,其中督脉又是阳脉之海,若经络不畅,则气血运行阻滞,精微物质无法上荣头目,因而引发眩晕。天开门手法中的点按印堂穴可促进督脉气血运行、提神醒脑; 百会、印堂相配可畅达气机、调和阴阳; 天开门手法可开窍醒神、发汗解表; 运双侧太阳穴可止晕止痛。天开门手法针对头面部经络系统,结合点、线、面操作,疏导胆经、督脉、胃经、膀胱经与头部各穴位,可调节督脉气机运行,输送物质精微上荣于头,从而发挥阳气升达、醒神定眩的作用。现代医学研究[17]发现,天开门手法通过刺激头皮神经与表皮血管,可促进头部血液循环,增加大脑血供,消除局部血管紧张,调节交感神经紊乱,降低疼痛程度。②颈部有耳大神经、枕小神经、枕大神经等诸多神经分布,神经受挤压刺激后可引发颈项疼痛、头痛等症状。同时,肌肉长期处于劳累状态,易产生大量炎症介质,而炎症介质作用于颈部肌肉后会阻碍经络,不通则痛。颈部手法中通过弹拨患者头半棘肌、枕下小肌群、斜方肌、肩胛提肌等颈部肌肉,可松解组织粘连,解除肌肉痉挛,减轻肌肉疼痛程度[18]。同时,对各个颈部肌肉按压,可通过这些传输冲动汇集于中枢产生兴奋,兴奋通过传出神经传至效应器,从而改善局部血液循环、促进局部毛细血管扩张、促进致痛因子与炎症介质吸收。③研究[19]报道低频(≤5 Hz)经颅磁刺激可诱导长期突触抑制,减弱神经细胞兴奋性,而高频(>5 Hz)可诱导长期突触强化,提高神经细胞电活动。由于耳石症复位后残余头晕可能是因残余碎片持续兴奋性刺激内耳前庭器官内毛细胞所致,故本研究经颅磁刺激的频率设置为1 Hz。低频经颅磁刺激减轻疼痛的作用机制可能为: 减弱神经元兴奋性,抑制前庭神经核神经冲动传导至前庭外侧多突触1型神经元,进而降低头痛程度; 低频经颅磁刺激可调整M1区域兴奋性,延缓静息时长,经丘脑与脑皮层之间环路来阻滞丘脑疼痛感觉信息传导,影响神经突触兴奋性与联络性,增加γ-氨基丁酸等神经抑制性递质释放,从而减轻或消除疼痛感[20]。④睡觉时取健侧卧位,可避免因患侧肌肉组织受到压迫而导致的疼痛,增加血流量,从而缓解疼痛。
交感神经兴奋可促使汗腺分泌,影响皮肤电阻,造成SSR电位发生变化,故SSR可通过检测皮肤电阻改变来评估交感神经功能。HAGEMAN K N等[21]进行的动物实验发现,健康猫水平方向转头时交感神经活性不会发生明显变化,而倾斜或抬头时交感神经活性大大增加,表明耳石器会影响前庭交感反射。钱淑霞等[22]研究认为,耳石症复位后残余头晕的发生机制可能为耳石症伴前庭显微结构改变与耳石器障碍,导致双侧椭圆囊斑重力不均,从而导致残余头晕; 同时,该研究还发现残余头晕组SSR波幅明显增高,潜伏期缩短,证实耳石症复位后残余头晕患者伴有自主神经功能异常。本研究中,实验组疗程结束后SSR波幅值比对照组低, SSR潜伏期值比对照组高,可见三联疗法联合倍他司汀可改善SSR与交感神经功能,这也是减轻疼痛的作用机制之一。
综上所述,三联疗法联合倍他司汀治疗耳石症复位后残余头晕疗效确切,可减轻眩晕、前庭症状,提高患者活动平衡信心,降低焦虑程度,改善SSR与大脑血流循环。
-
表 1 学龄前急性上呼吸道感染高热惊厥患儿早期病情变化的单因素分析(x±s)[n(%)]
指标 分类 低危组(n=294) 中危组(n=65) 高危组(n=25) F/χ2 P 性别 男 172(58.5) 35(53.8) 14(56.0) 0.499 0.779 女 122(41.5) 30(46.2) 11(44.0) 年龄 ≤5岁 121(41.2) 33(50.8) 18(72.0) 13.644 0.009 >5岁 173(58.8) 32(49.2) 7(28.0) 既往发生过高热惊厥 是 85(28.9) 38(58.5) 18(72.0) 34.329 < 0.001 否 209(71.1) 27(41.5) 7(28.0) 家族高热惊厥史 有 122(41.5) 36(55.4) 13(52.0) 4.760 0.093 无 172(58.5) 29(44.6) 12(48.0) 家族癫痫史 有 124(42.2) 32(49.2) 13(52.0) 1.768 0.413 无 170(57.8) 33(50.8) 12(48.0) 急诊绿色通道 是 188(63.9) 30(46.2) 6(24.0) 19.902 < 0.001 否 106(36.1) 35(53.8) 19(76.0) 接受氧疗 是 160(54.4) 31(47.7) 7(28.0) 6.910 0.032 否 134(45.6) 34(52.3) 18(72.0) 退热措施 物理退热 162(55.1) 34(52.3) 7(28.0) 6.802 0.033 药物退热 132(44.9) 31(47.7) 18(72.0) 伴有抽搐 是 39(13.3) 29(44.6) 13(52.0) 46.779 < 0.001 否 255(86.7) 36(55.4) 12(48.0) 伴有呼吸节律紊乱 是 44(15.0) 33(50.8) 18(72.0) 68.727 < 0.001 否 250(85.0) 32(49.2) 7(28.0) 伴有意识模糊 是 48(16.3) 28(43.1) 15(60.0) 42.916 < 0.001 否 256(87.1) 37(56.9) 10(40.0) 血压 低 125(42.5) 17(26.2) 7(28.0) 14.806 0.005 正常 103(35.0) 20(30.8) 8(32.0) 高 66(22.4) 28(43.1) 10(40.0) BR/(次/min) 16.1±2.2 18.3±3.0 22.3±4.1 655.270 < 0.001 HR/(次/min) 86.2±6.4 90.3±6.4 92.3±7.4 13.975 < 0.001 NLR/% 3.0±0.4 3.2±0.5 3.3±0.5 6.028 0.003 RDW/% 14.4±0.4 14.7±0.6 14.8±0.5 33.485 < 0.001 SaO2/% 87.4±6.5 82.3±7.3 80.5±7.4 24.567 < 0.001 HGB/(g/L) 108.7±15.1 101.8±15.2 98.3±12.1 9.881 < 0.001 PCT/(ng/mL) 8.5±2.0 9.7±2.3 12.7±3.1 10.358 < 0.001 CRP/(μg/L) 18.4±4.2 19.4±4.4 20.4±4.3 11.314 < 0.001 血钠/(mmol/L) 142.3±12.4 140.3±12.3 134.2±10.1 5.232 0.006 血钙/(mmol/L) 2.1±0.6 1.9±0.5 1.8±0.5 4.019 0.019 惊厥类型 复杂型 107(36.4) 20(30.8) 19(76.0) 17.083 0.002 单纯型 187(63.6) 45(69.2) 6(24.0) 惊厥后至高热时间 ≤12 h 125(42.5) 32(49.2) 18(72.0) 8.497 0.014 >12 h 169(57.5) 33(50.8) 7(28.0) 惊厥持续时间 < 1 min 124(42.2) 19(29.2) 4(16.0) 14.866 0.021 1~5 min 82(27.9) 20(30.8) 6(24.0) >5~10 min 53(18.0) 15(23.1) 7(28.0) >10 min 35(11.9) 11(16.9) 8(32.0) 首次惊厥后平均体温 ≤39.0 ℃ 60(20.4) 9(13.8) 3(12.0) 24.727 < 0.001 >39.0~40.0 ℃ 111(37.8) 22(33.8) 5(20.0) >40.0~41.0 ℃ 86(29.3) 24(36.9) 5(20.0) >41.0 ℃ 37(12.6) 10(15.4) 12(48.0) 再次惊厥次数 ≤1次 212(72.1) 37(56.9) 12(48.0) 12.670 0.013 >1~3次 47(16.0) 20(30.8) 8(32.0) >3次 35(11.9) 8(12.3) 5(20.0) 表 2 学龄前急性上呼吸道感染高热惊厥患儿早期病情变化的多元有序Logistic回归分析结果
自变量 B S. E. Wald χ2 OR P 95%CI 下限 上限 年龄 0.169 0.022 60.366 0.845 < 0.001 0.810 1.235 伴有抽搐 1.446 0.429 13.082 4.246 < 0.001 1.822 8.681 伴有呼吸节律紊乱 1.221 0.351 10.171 3.391 < 0.001 1.130 8.837 伴有意识模糊 1.217 0.624 9.121 3.377 0.006 1.113 8.499 BR 2.121 0.949 5.001 8.339 0.016 1.343 64.522 NLR 2.280 0.978 5.430 9.777 0.020 1.436 66.553 RDW 2.271 0.739 7.134 9.689 0.011 1.374 41.264 首次惊厥后平均体温 0.162 0.022 55.790 1.176 < 0.001 1.127 1.228 >40.0~41.0 ℃ -0.361 0.427 0.714 0.697 0.398 0.301 1.610 >39.0~40.0 ℃ -0.623 0.290 4.620 0.536 0.032 0.304 0.946 平行检验: χ2=40.152, P < 0.001; 拟合优度检验: χ2=82.538, P < 0.001。 表 3 学龄前急性上呼吸道感染高热惊厥患儿早期高危病情二元Logistic回归分析结果
自变量 B S. E. Wald χ2 OR P 95%CI 下限 上限 年龄(≤5岁=0, >5岁=1) -1.618 0.514 9.894 0.198 0.002 0.072 0.544 是否伴有抽搐(否=0, 是=1) 1.075 0.430 6.256 2.931 0.012 1.262 6.808 是否伴有呼吸节律紊乱(否=0, 是=1) 0.975 0.439 4.929 2.650 0.026 1.121 6.265 是否伴有意识模糊(否=0, 是=1) 1.143 0.432 7.005 3.137 0.008 1.345 7.313 BR(原值) 0.115 0.048 5.598 1.122 0.018 1.020 1.233 NLR(原值) 1.623 0.505 10.317 5.070 0.001 1.883 13.651 RDW(原值) 0.300 0.073 16.783 1.350 < 0.001 1.169 1.559 首次惊厥后平均体温(≤39.0 ℃=1; >39.0~40.0 ℃=2; >40.0~41.0 ℃=3; >41.0 ℃=4) 0.330 0.157 4.402 1.391 0.036 1.022 1.892 常数项 -9.952 2.400 17.190 < 0.001 < 0.001 — — 霍斯默-莱梅肖检验: χ2=0.270, P=0.332。 表 4 学龄前急性上呼吸道感染高热惊厥患儿早期高危病情影响因素的效能分析
检验变量 AUC S. E. P 95%CI 下限 上限 年龄(>5岁) 0.338 0.036 < 0.001 0.267 0.410 伴有抽搐 0.591 0.042 0.038 0.509 0.673 伴有呼吸节律紊乱 0.634 0.040 0.002 0.557 0.711 伴有意识模糊 0.639 0.040 0.002 0.561 0.717 BR 0.696 0.045 < 0.001 0.608 0.783 NLR 0.672 0.041 < 0.001 0.591 0.753 RDW 0.748 0.043 < 0.001 0.663 0.833 首次惊厥后平均体温 0.663 0.041 < 0.001 0.582 0.745 表 5 预测模型对测试集和训练集预测效能比较
数据集 预测概率AUC S. E. P 95%CI 测试集 0.780 0.034 < 0.001 0.888~0.966 训练集 0.927 0.020 < 0.001 0.714~0.846 表 6 学龄前急性上呼吸道感染高热惊厥患儿早期高危病情影响因素赋值表
影响因素 赋值 年龄 >5岁=0分,≤5岁=33分 伴有抽搐 是=0分,否=22分 伴有呼吸节奏紊乱 是=0分,否=20分 伴有意识模糊 是=0分,否=23分 BR 8次/min =0分, 10次/min =5分, 12次/min =9分, 14次/min =14分, 16次/min =19分, 18次/min =24分, 20次/min =28分, 22次/min =33分, 24次/min =38分, 26次/min =42分, 28次/min =47分, 30次/min =52分, 32次/min =57分 NLR 2.0%=0分, 2.5%=17分, 3.0%=33分, 3.5%=50分, 4.0%=67分, 4.5%=83分, 5.0%=100分 RDW 8%=0分, 10%=12分, 12%=25分, 14%=37分, 16%=49分, 18%=62分, 20%=74分, 22%=86分, 24%=99分 首次惊厥后平均体温 ≤39.0 ℃=0分; >39.0~40.0 ℃=7分; >40.0~41.0 ℃=14分; >41.0 ℃=20分 总分对应的风险概率 85分=0.1%, 132分=1%, 166=5%, 182分=10%, 198分=20%, 209分=30%, 218分=40%, 227分=50%, 235分=60%, 244分=70%, 255分=80%, 272分=90%, 287分=95% -
[1] 曹丽洁, 帅金凤, 刘建华, 等. 2014—2017年石家庄地区住院儿童急性呼吸道感染病毒病原学分析[J]. 中华实验和临床病毒学杂志, 2019, 33(4): 400-404. doi: 10.3760/cma.j.issn.1003-9279.2019.04.014 [2] 董娜, 王爱琼. 炎症反应、热性惊厥与继发性癫痫相关性研究进展[J]. 临床儿科杂志, 2015, 33(10): 896-899. doi: 10.3969/j.issn.1000-3606.2015.10.014 [3] 李娟, 王丹, 王艳, 等. 小儿高热惊厥的危险因素及护理对策[J]. 实用临床医药杂志, 2017, 21(18): 107-109. doi: 10.7619/jcmp.201718034 [4] DREIER J W, LI J, SUN Y L, et al. Evaluation of long-term risk of epilepsy, psychiatric disorders, and mortality among children with recurrent febrile seizures: a national cohort study in Denmark[J]. JAMA Pediatr, 2019, 173(12): 1164-1170. doi: 10.1001/jamapediatrics.2019.3343
[5] 蹇英, 朱雪凤, 王惠芬, 等. 改良早期预警评分在儿童急诊分诊中的应用[J]. 中国急救复苏与灾害医学杂志, 2018, 13(1): 97-98. https://www.cnki.com.cn/Article/CJFDTOTAL-SZZX202210039.htm [6] 王卫平. 儿科学(第9版/本科临床/配增值)[M]. 北京: 人民卫生出版社, 2018: 1-10. [7] 中华医学会儿科学分会神经学组. 热性惊厥诊断治疗与管理专家共识(2017实用版)[J]. 中华实用儿科临床杂志, 2017, 32(18): 1379-1382. [8] 王瑞平. 随机对照临床试验设计中的样本量估算方法[J]. 上海医药, 2023, 44(1): 48-52. https://www.cnki.com.cn/Article/CJFDTOTAL-SYIY202301013.htm [9] DUNCAN H, HUTCHISON J, PARSHURAM C S. The Pediatric Early Warning System score: a severity of illness score to predict urgent medical need in hospitalized children[J]. J Crit Care, 2006, 21(3): 271-278. doi: 10.1016/j.jcrc.2006.06.007
[10] 郭伟中. 小儿热性惊厥复发的相关因素分析[J]. 医学综述, 2016, 22(15): 3070-3072. https://www.cnki.com.cn/Article/CJFDTOTAL-YXZS201615046.htm [11] 李娟, 刘秀云, 殷菊, 等. 儿童重症腺病毒肺炎急性期临床特点分析[J]. 北京医学, 2019, 41(11): 1013-1016. https://www.cnki.com.cn/Article/CJFDTOTAL-BJYX201911017.htm [12] 李晓娜. 针对性急救护理在高热惊厥患儿急诊护理中的应用效果探讨[J]. 中国冶金工业医学杂志, 2020, 37(2): 242-243. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGYJ202002113.htm [13] 刘科贝. 高热惊厥小儿的临床特征及预后分析[J]. 实用临床医药杂志, 2019, 23(16): 16-19. doi: 10.7619/jcmp.201916005 [14] 李爱月, 张巧丽, 赵燕芳, 等. 616例小儿热性惊厥首次发作的临床特点及危险因素分析[J]. 中国小儿急救医学, 2020, 27(4): 298-301. [15] 陈芳芳. 沟通技巧在门诊学龄前儿童患者中的应用[J]. 浙江中医药大学学报, 2007, 31(2): 219-220. https://www.cnki.com.cn/Article/CJFDTOTAL-BHON200702048.htm [16] 白利洁, 许丽霞, 郭明丽, 等. 热性惊厥患儿临床特点及复发因素分析[J]. 河北医药, 2015, 37(14): 2130-2133. https://www.cnki.com.cn/Article/CJFDTOTAL-HBYZ201514015.htm [17] 卢一斌, 刘占利, 马效东. NLR和RDW在小儿高热惊厥中的表达及其与T淋巴细胞水平的相关性研究[J]. 重庆医学, 2019, 48(17): 2953-2955, 2959. https://www.cnki.com.cn/Article/CJFDTOTAL-CQYX201917017.htm [18] 张丽丹, 黄慧敏, 程玉才, 等. 4种小儿危重死亡评分对危重患儿死亡风险的预测价值[J]. 中华危重病急救医学, 2018, 30(1): 51-56. [19] 陈嘉蕾, 刘平, 胡文广, 等. 热性惊厥持续状态复发的危险因素分析[J]. 临床神经病学杂志, 2021, 34(1): 10-13. https://www.cnki.com.cn/Article/CJFDTOTAL-LCSJ202101004.htm -
期刊类型引用(5)
1. 毕勇志,马芬,宋琳琳. 血清HBP、CRP、PCT在早期毛细血管渗漏综合征患者中的表达分析. 罕少疾病杂志. 2024(02): 111-112+120 .  百度学术
百度学术
2. 陈雯,钱风华,孙旗,丁纯蕾,杨家豪,姜旭升,沈梦雯. 四逆升降散干预“肝-脾轴”改善脓毒症急性肺损伤预后的临床研究. 中国中医急症. 2024(11): 1929-1933 .  百度学术
百度学术
3. 林柏柏,赵雷,丁纯蕾,钱义明,张琼,谭美春,陆云霞,沈梦雯. 四逆升降散对脓毒症毛细血管渗漏综合征患者凝血功能的影响. 中国中医急症. 2024(11): 1934-1937 .  百度学术
百度学术
4. 闫雨蒙,徐霄龙,李博,郭玉红,刘清泉. 2000—2022年中医药治疗脓毒症研究文献的知识图谱可视化分析. 中医杂志. 2023(16): 1700-1706 .  百度学术
百度学术
5. 谷翠红,王阳,林丽,王丽红,张志华. 抗胸腺细胞球蛋白联合环孢素A治疗儿童重型再生障碍性贫血诱发毛细血管渗透综合征1例. 临床荟萃. 2023(09): 819-822 .  百度学术
百度学术
其他类型引用(1)




 下载:
下载:
 苏公网安备 32100302010246号
苏公网安备 32100302010246号
