Construction of a nomogram model for risk of unstable ventilation pressure during nasal continuous positive airway pressure treatment for hyaline membrane disease in neonates
-
摘要:目的
分析新生儿肺透明膜病(HMD)患儿经鼻持续正压通气(NCPAP)治疗中通气压力不稳定的影响因素并构建列线图模型。
方法回顾性选取行NCPAP治疗的157例HMD患儿作为研究对象,根据治疗中有无发生通气压力不稳定分为不稳定组49例和稳定组108例。采用Logistic回归模型分析HMD患儿NCPAP治疗中通气压力不稳定的影响因素,利用R软件构建列线图模型,并通过受试者工作特征(ROC)曲线、校准曲线、Hosmer-Lemeshow拟合优度检验评估列线图模型的预测效能。
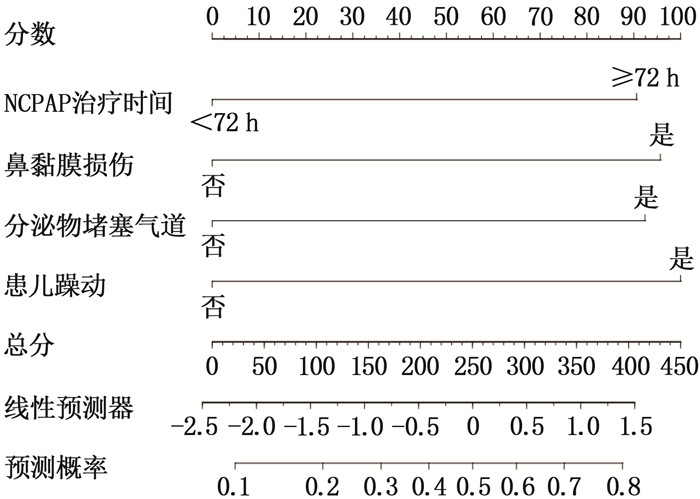
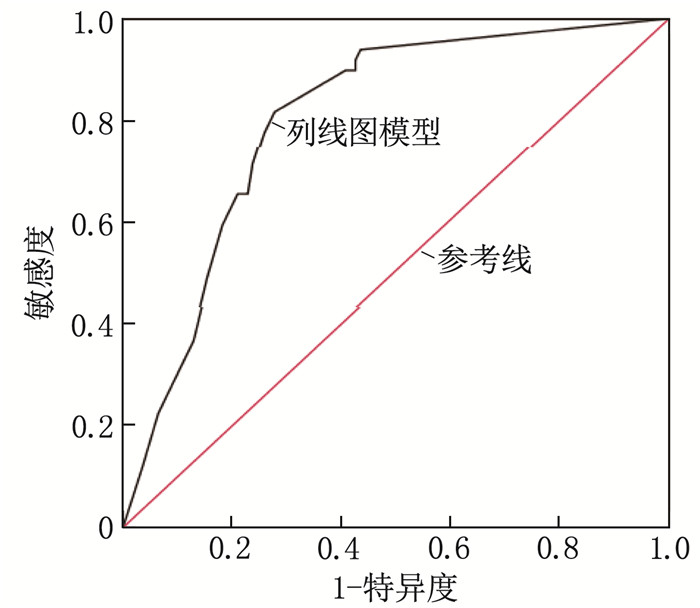
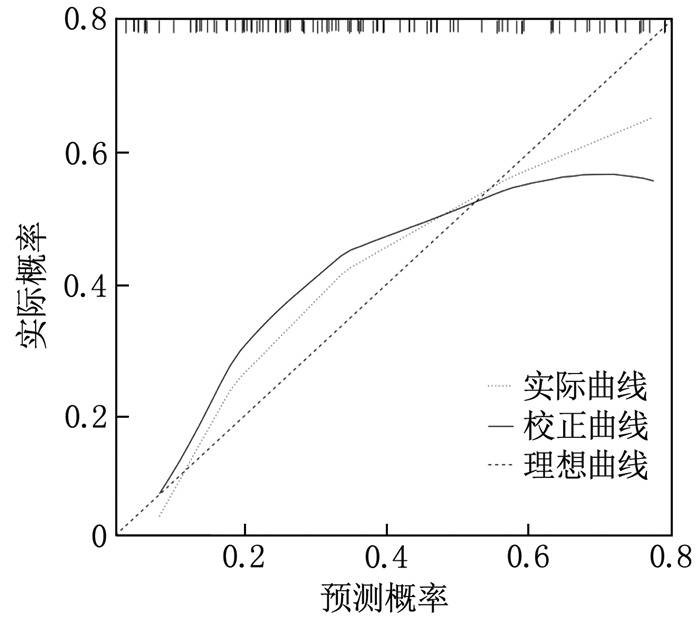
结果49例HMD患儿NCPAP治疗中发生通气压力不稳定,发生率为31.21%(49/157)。单因素分析显示, NCPAP治疗中通气压力不稳定与患儿的胎龄、性别、出生体质量、分娩方式、新生儿Apgar评分以及NCPAP治疗中导管扭曲、管内冷凝水过多无关(P>0.05); NCPAP治疗时间、鼻黏膜损伤、分泌物堵塞气道、躁动是HMD患儿NCPAP治疗中通气压力不稳定的影响因素(P < 0.05)。多因素Logistic回归分析显示, NCPAP治疗时间≥72 h、鼻黏膜损伤、分泌物堵塞气道、躁动为HMD患儿NCPAP治疗中通气压力不稳定的独立危险因素(P < 0.05), 基于4项独立危险因素构建列线图模型。ROC曲线显示,该列线图模型的区分度良好,曲线下面积为0.801(95%CI: 0.730~0.861); Hosmer-Lemeshow拟合优度检验结果显示χ2=3.550, P=0.470, 校准曲线斜率接近1, 提示该列线图预测模型的拟合效度良好。
结论基于NCPAP治疗时间、鼻黏膜损伤、分泌物堵塞气道、躁动构建的列线图模型, 对HMD患儿NCPAP治疗中是否发生通气压力不稳定具有较好的预测价值。
Abstract:ObjectiveTo analyze the influencing factors of unstable ventilation pressure during nasal continuous positive airway pressure (NCPAP) treatment in neonates with hyaline membrane disease (HMD) and construct a nomogram model.
MethodsA retrospective analysis was conducted in 157 HMD neonates who underwent NCPAP treatment. The patients were divided into unstable group (n=49) and stable group (n=108) based on the occurrence of unstable ventilation pressure during treatment. Logistic regression analysis was used to identify influencing factors of unstable ventilation pressure during NCPAP treatment in HMD neonates. A nomogram model was constructed using R software, and its predictive performance was evaluated using receiver operating characteristic (ROC) curves, calibration curves, and the Hosmer-Lemeshow goodness-of-fit test.
ResultsUnstable ventilation pressure occurred in 49 HMD neonates during NCPAP treatment, with an incidence rate of 31.21% (49/157). Univariate analysis showed that unstable ventilation pressure during NCPAP treatment had no relation to gestational age, gender, birth weight, delivery mode, neonatal Apgar score, catheter distortion, or excessive condensation in the tube (P>0.05). However, NCPAP treatment duration, nasal mucosa damage, secretion blockage in the airway, and restlessness were identified as influencing factors for unstable ventilation pressure during NCPAP treatment in HMD neonates (P < 0.05). Multivariate Logistic regression analysis revealed that NCPAP treatment duration ≥72 h, nasal mucosa damage, secretion blockage in the airway, and restlessness were independent risk factors for unstable ventilation pressure during NCPAP treatment in HMD neonates (P < 0.05). A nomogram model was constructed based on these four independent risk factors. The ROC curve demonstrated good discrimination for the nomogram model, with an area under the curve of 0.801 (95%CI, 0.730 to 0.861). The Hosmer-Lemeshow goodness-of-fit test showed a chi-square value of 3.550 with a P-value of 0.470, and the calibration curve had a slope close to 1, indicating good fit validity for the nomogram prediction model.
ConclusionThe nomogram model constructed based on NCPAP treatment duration, nasal mucosa damage, secretion blockage in the airway, and restlessness has good predictive value for the occurrence of unstable ventilation pressure during NCPAP treatment in HMD neonates.
-
产妇剖宫产后形成下肢静脉血栓的风险较高,若未及时接受有效防治措施,一旦出现血栓脱落,容易形成肺栓塞并增大死亡风险。静脉血栓形成因素主要包括血液滞缓、静脉壁受损以及血液高凝状态等,剖宫产术后产妇血液滞缓等危险因素均容易引发下肢静脉血栓。因此,为了促进产妇产后康复并改善母婴健康,尽早采取针对性的下肢静脉血栓预防措施具有重要应用价值[1-3]。本研究以剖宫产产妇为研究对象,分析其应用小剂量阿司匹林联合空气波压力治疗仪对抑制术后下肢静脉血栓形成率方面的作用,现报告如下。
1. 资料与方法
1.1 一般资料
选取2018年3月—2019年3月122例在本院进行剖宫产的产妇为研究对象,纳入标准: 入选产妇与其家属对本研究均知情并签署知情同意书; 均实施剖宫产分娩。排除标准: 产前已确诊下肢静脉血栓的产妇; 入组前接受过抗凝药物治疗的产妇; 全身免疫性疾病产妇; 凝血功能障碍产妇[4-6]。采用便利抽样法将入选产妇分为2组,其中实验组61例,年龄21~44岁,平均(28.9±5.6)岁; 初产妇36例、经产妇25例; 过期妊娠2例、早产11例、胎位异常3例、妊娠期高血压7例、巨大儿6例、骨盆异常9例; 术中出血量为(254.4±12.3) mL; 手术时间为(32.1±8.2) min。对照组61例,年龄19~44岁,平均(29.2±5.5)岁; 初产妇39例、经产妇22例; 过期妊娠2例、早产13例、胎位异常4例、妊娠期高血压9例、巨大儿5例、骨盆异常8例; 术中出血量为(256.1±12.7) mL; 手术时间为(33.4±8.0) min。本研究经伦理委员会批准。2组产妇剖宫产相关指标以及年龄等临床资料差异无统计学意义(P>0.05)。
1.2 方法
所有产妇均采用下肢静脉静脉血栓预防护理。体位护理: 术后6 h将产妇体位调整为半卧位,按时协助其翻身,防止肢体长时间受压,影响血液循环[7-9]; 下肢锻炼指导:术后指导产妇进行膝关节、踝关节伸展练习以及四肢收缩运动;饮食干预:指导产妇进食维生素以及蛋白质含量较高的食物,多食用茼蒿、洋葱、大蒜以及黑木耳等吡嗪类含量较高的食物,有利于促进血液流通并降低血栓形成率[10-12]。实验组产妇在接受常规护理的基础上联合应用空气波压力治疗仪以及小剂量阿司匹林治疗,阿司匹林服用剂量为75 mg/次, 1次/d, 术日联合应用空气波压力治疗仪治疗,为产妇实施双下肢空气驱动治疗,每次治疗30 min, 1次/d, 共计治疗5次[13-15]。
1.3 评价指标
统计并对比2组产妇下肢静脉血栓形成情况。对比2组产妇术后1周双下肢肿胀指数以及静息心指数,术后1周应用生物电阻抗分析法检测2组产妇静息心指数,静息心指数越高说明产妇心功能损伤越严重,双下肢肿胀指数越高说明产妇双下肢肿胀越严重。对比2组产妇产后不同时间视觉模拟评分法(VAS)评分,分别于术后第3天、术后1周以及术后2周指导产妇应用评分评估双下肢疼痛程度, 0分为无痛感, 10分为有剧烈痛感且超出产妇耐受度,产妇疼痛感越强烈则评分越高。
1.4 统计学分析
本研究数据资料采用SPSS 21.0统计软件包进行处理分析,计量资料采用(x±s)表示,计数资料采用率表示,分别以t、χ2检验比较2组差异,以P<0.05表示差异有统计学意义。
2. 结果
2.1 2组产妇下肢静脉血栓形成率比较
实验组产妇未出现下肢静脉血栓,对照组共8例产妇出现下肢静脉血栓,静脉血栓形成率为13.1%。对照组产妇下肢静脉血栓形成率高于实验组,差异有统计学意义(P<0.05), 见表 1。
表 1 2组产妇下肢静脉血栓形成率比较[n(%)]组别 左胫后静脉血栓 右下肢腓肠肌肌间静脉血栓 左下肢腓肠肌肌间静脉血栓 合计 实验组(n=61) 0 0 0 0* 对照组(n=61) 3(4.9) 3(4.9) 2(3.3) 8(13.1) 与对照组比较, *P<0.05。 2.2 2组产妇术后1周双下肢肿胀指数以及静息心指数比较
剖宫产术后1周,实验组产妇双下肢肿胀指数以及静息心指数均低于对照组,差异有统计学意义(P<0.05), 见表 2。
表 2 2组产妇术后1周双下肢肿胀指数以及静息心指数比较(x±s)组别 肿胀指数 静息心指数 实验组(n=61) 3.0±2.2* 2.1±1.3* 对照组(n=61) 6.2±2.9 3.4±1.2 与对照组比较, *P<0.05。 2.3 2组产妇术后不同时间VAS评分比较
实验组产妇术后第3天、术后1周以及术后2周VAS评分均较对照组产妇低,差异有统计学意义(P<0.05), 见表 3。
表 3 2组产妇术后不同时间VAS评分比较(x±s)分 组别 术后第3天 术后1周 术后2周 实验组(n=61) 2.3±1.2* 2.1±1.1* 1.1±0.5* 对照组(n=61) 2.8±1.3 3.5±1.2 2.2±0.8 与对照组比较, *P<0.05。 3. 讨论
剖宫产术后下肢静脉血栓形成等并发症发生率较高,一旦血栓脱落进入产妇肺部,极大程度地危害产妇的生命安全。妊娠期产妇胎盘内生成大量雌激素,肝脏内有多种凝血因子形成,纤维蛋白含量显著增加,导致血液高凝状态形成。此外,受麻醉等因素影响,周围静脉血流明显减缓,容易导致下肢静脉血栓形成[16-17]。
阿司匹林可对血小板聚集产生抑制作用,显著降低环氧合酶合成量,下肢静脉血栓形成预防效果理想。空气波压力治疗仪可促进动脉灌注、静脉回流以及淋巴循环,防止凝血因子聚集,可使血管内膜黏附作用得到明显降低,同时促进肢体以及组织血液循环,因此预防双下肢水肿以及血栓形成的效果理想[18]。
本研究实验组产妇未出现下肢静脉血栓,对照组下肢静脉血栓形成率为13.1%; 剖宫产术后1周,实验组产妇双下肢肿胀指数以及静息心指数均显著低于对照组; 实验组术后第3天、术后1周以及术后2周VAS评分均较对照组产妇低。综上所述,剖宫产产妇应用小剂量阿司匹林与联合空气波压力治疗仪可明显降低下肢静脉血栓形成率,有助于促进产后康复。
-
表 1 HMD患儿NCPAP治疗中发生通气压力不稳定的单因素分析(x±s)[n(%)]
指标 分类 稳定组(n=108) 不稳定组(n=49) χ2/t P 胎龄/周 31.40±3.72 32.25±3.95 1.301 0.195 性别 男 57(52.78) 23(46.94) 0.460 0.498 女 51(47.22) 26(53.06) 出生体质量/g 3 170.22±336.50 3 085.50±320.06 1.484 0.140 分娩方式 自然分娩 61(56.48) 28(57.14) 0.006 0.938 剖宫产 47(43.52) 21(42.86) NCPAP治疗时间 < 72 h 80(74.07) 17(34.69) 22.139 < 0.001 ≥72 h 28(25.93) 32(65.31) 鼻黏膜损伤 是 26(24.07) 31(63.27) 22.388 < 0.001 否 82(75.93) 18(36.73) 分泌物堵塞气道 是 24(22.22) 28(57.14) 18.556 < 0.001 否 84(77.78) 21(42.86) 患儿躁动 是 30(27.78) 32(65.31) 19.867 < 0.001 否 78(72.22) 17(34.69) 新生儿Apgar评分/分 5.78±1.03 5.57±0.98 1.201 0.231 导管扭曲 是 17(15.74) 10(20.41) 0.516 0.473 否 91(84.26) 39(79.59) 管内冷凝水过多 是 9(8.33) 6(12.24) 0.597 0.440 否 99(91.67) 43(87.76) 表 2 HMD患儿NCPAP治疗中通气压力不稳定的多因素Logistic回归分析
指标 β SE Wald P OR 95%CI NCPAP治疗时间 0.872 0.425 4.212 0.040 2.393 1.040~5.505 鼻黏膜损伤 0.921 0.420 4.804 0.028 2.512 1.102~5.725 分泌物堵塞气道 0.890 0.419 4.518 0.034 2.434 1.072~5.529 躁动 0.963 0.418 5.294 0.021 2.619 1.153~5.948 常量 -2.409 0.389 38.430 < 0.001 0.090 — -
[1] 刘新学. 新生儿呼吸窘迫综合征临床特征及预后影响因素分析[J]. 内蒙古医学杂志, 2020, 52(9): 1078-1078. [2] 宁浩杰, 韦德湛, 罗慧, 等. 高频肺部超声结合分区域扫查早期鉴别新生儿肺透明膜病及湿肺的研究[J]. 现代生物医学进展, 2020, 20(21): 4177-4181. [3] SAKURAI R, LEE C, SHEN H, et al. A combination of the aerosolized PPAR-γ agonist pioglitazone and a synthetic surfactant protein B peptide mimic prevents hyperoxia-induced neonatal lung injury in rats[J]. Neonatology, 2018, 113(4): 296-304. doi: 10.1159/000486188
[4] 陈宝英, 梁惠冰, 周玲, 等. 儿童早期预警评分在儿童重症肺炎治疗中的应用效果[J]. 深圳中西医结合杂志, 2021, 31(4): 110-111. [5] 郭娇, 张洁琼. 优质护理模式在NCPAP治疗儿童重症肺炎合并呼吸衰竭中的应用效果观察[J]. 贵州医药, 2022, 46(11): 1834-1835. [6] 陆艺, 李双双, 余章斌, 等. 持续正压通气治疗早产儿失败的危险因素及结局的系统评价和Meta分析[J]. 中国循证儿科杂志, 2019, 14(6): 422-427. doi: 10.3969/j.issn.1673-5501.2019.06.005 [7] 王卫平, 孙锟, 常立文. 儿科学[M]. 9版. 北京: 人民卫生出版社, 2018: 107-111. [8] NELSON S M, ILIODROMITI S, MACKAY D F, et al. Apgar score and risk of cause-specific infant mortality-authors′reply[J]. Lancet, 2015, 385(9967): 506.
[9] 王成, 段玉松, 叶盎然, 等. PCV+SIMV模式与VTPC+SIMV模式治疗新生儿呼吸窘迫综合征的对比研究[J]. 西部医学, 2022, 34(4): 580-584. [10] SWEET D G, CARNIELLI V P, GREISEN G, et al. European consensus guidelines on the management of respiratory distress syndrome: 2022 update[J]. Neonatology, 2023, 120(1): 3-23. doi: 10.1159/000528914
[11] 赵宝君, 刘雪琴, 王平. 新生儿经鼻持续无创正压通气致鼻损伤的现状调查及影响因素分析[J]. 中华现代护理杂志, 2022, 28(14): 1944-1947. [12] 付晓宁, 杨爱国. NCPAP联合小剂量多巴胺用于小儿重症毛细支气管炎的临床效果观察[J]. 贵州医药, 2022, 46(6): 868-870. [13] 阎进晓, 邓巧妮. 鼻塞式持续气道正压通气(NCPAP)治疗小儿重症肺炎的疗效及安全性分析[J]. 贵州医药, 2021, 45(6): 883-884. [14] 章晓波, 吴琼, 王际铭. 新生儿肺透明膜病机械通气治疗的应用及预后评价[J]. 解放军预防医学杂志, 2019, 37(8): 77-78. [15] 钟艳玲. 新生儿肺透明膜病患儿NCPAP治疗中通气压力不稳定的因素分析[J]. 现代诊断与治疗, 2021, 32(19): 3116-3117. [16] 孔东雯, 王晓龙, 王世昌, 等. INSURE技术治疗早产儿呼吸窘迫综合征中临床效果及预后影响因素分析[J]. 中国初级卫生保健, 2020, 34(1): 66-68. [17] 丁晓燕. 布地奈德联合持续正压通气治疗新生儿呼吸窘迫综合征疗效研究[J]. 陕西医学杂志, 2022, 51(5): 599-603. [18] 杨国勇, 高春燕, 国燕, 等. 水胶体敷料预防正颌外科手术患者鼻翼压力性损伤的效果[J]. 中华现代护理杂志, 2019, 25(6): 733-736. [19] 梁欢, 王伏东, 蒋丽军, 等. 俯卧位通气在新生儿急性呼吸窘迫综合征治疗中的临床应用[J]. 实用临床医药杂志, 2022, 26(14): 114-118. doi: 10.7619/jcmp.20220211 -
期刊类型引用(16)
1. 张艳,陈小龙,刘静,张秀珍. 桃红四物汤合防己黄芪汤结合空气压力波治疗仪预防术后下肢深静脉血栓的效果观察. 四川中医. 2024(04): 127-130 .  百度学术
百度学术
2. 赖玲治,陈婷婷,白亚铃,李焕根. 气压治疗仪联合红外线照射预防重症患者下肢深静脉血栓. 中国医学物理学杂志. 2024(11): 1415-1420 .  百度学术
百度学术
3. 袁晓莉,张丽杰. 依诺肝素钠联合空气波压力治疗仪对高危产妇剖宫产术后下肢DVT的防治效果及对微循环、PAF、CD62P、CD63的影响. 临床医学研究与实践. 2023(25): 78-81 .  百度学术
百度学术
4. 张霞,王妙维,王任杰,李果,王傲,尹雨涵,魏全. 人体成分分析仪联合空气循环压力在防治乳腺癌相关淋巴水肿的临床应用. 湖南师范大学学报(医学版). 2023(04): 71-74 .  百度学术
百度学术
5. 曾桂金. 空气治疗仪对剖宫产后高龄产妇下肢静脉血栓形成率的影响分析. 基层医学论坛. 2022(06): 130-132 .  百度学术
百度学术
6. 严丽金,曾兆芬,罗淑芳,张东丽. 护理研究持续性阶段护理干预服务减低剖宫产产妇疼痛及提高产后母乳喂养的价值评估. 医学食疗与健康. 2022(09): 130-132 .  百度学术
百度学术
7. 郭杏英. 空气波压力治疗仪联合加压弹力袜对剖宫产术后下肢静脉血栓的预防. 实用医技杂志. 2022(06): 664-666 .  百度学术
百度学术
8. 史军艳,蒋晓娟. 空气波压力治疗仪联合多元化护理预防全子宫切除术后患者下肢深静脉血栓形成的临床效果. 医疗装备. 2022(20): 172-174 .  百度学术
百度学术
9. 郭敬敬,曹曰针,王柱. 小剂量阿司匹林预防剖宫产后下肢静脉血栓的效果. 中国继续医学教育. 2021(12): 160-164 .  百度学术
百度学术
10. 韦宝珍. 预防神经外科患者下肢静脉血栓形成的护理综述. 外科研究与新技术. 2021(01): 74-77 .  百度学术
百度学术
11. 孟媛媛. 空气波压力治疗仪联合穴位按摩对肝胆手术后下肢深静脉血栓及褥疮的预防作用研究. 临床医学. 2021(05): 85-87 .  百度学术
百度学术
12. 陈雪芳,吴敏瑜,苏文英. 气压治疗仪联合常规术后护理对剖宫产后凝血指标的调节作用. 名医. 2021(01): 127-128 .  百度学术
百度学术
13. 艾艳霞,樊菊莲,苏丽. 阿司匹林及气压仪预防高龄剖宫产产妇术后下肢深静脉血栓形成. 血栓与止血学. 2021(06): 1021-1022 .  百度学术
百度学术
14. 潘玉琴,陶婷,吴晔. 空气压力波治疗仪联合体感诱发电位监测预防脊柱骨折术后下肢深静脉血栓形成的应用效果. 中国医学物理学杂志. 2021(12): 1554-1559 .  百度学术
百度学术
15. 曾瑜嫚. 剖宫产产妇术后采用空气波压力治疗仪降低双下肢深静脉血栓形成的重要性. 医学食疗与健康. 2021(11): 208-209 .  百度学术
百度学术
16. 郭蕊. 空气波压力治疗仪配合早期护理干预对剖宫产术后下肢深静脉血栓的预防效果. 医疗装备. 2020(14): 160-161 .  百度学术
百度学术
其他类型引用(0)




 下载:
下载:
 苏公网安备 32100302010246号
苏公网安备 32100302010246号
