Risk factor and prediction model construction for postoperative gastroparesis syndrome after laparoscopic radical gastrectomy for gastric cancer
-
摘要:目的
分析接受腹腔镜胃癌根治术(LRG)治疗的胃癌患者发生术后胃瘫综合征(PGS)的危险因素,构建PGS的列线图预测模型并验证其预测效能。
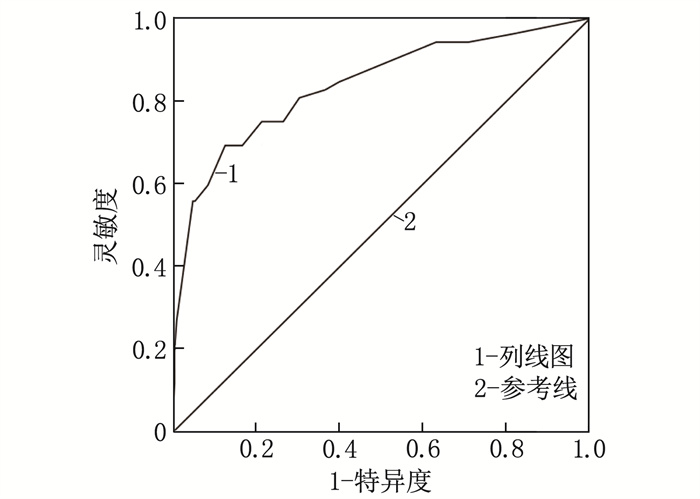
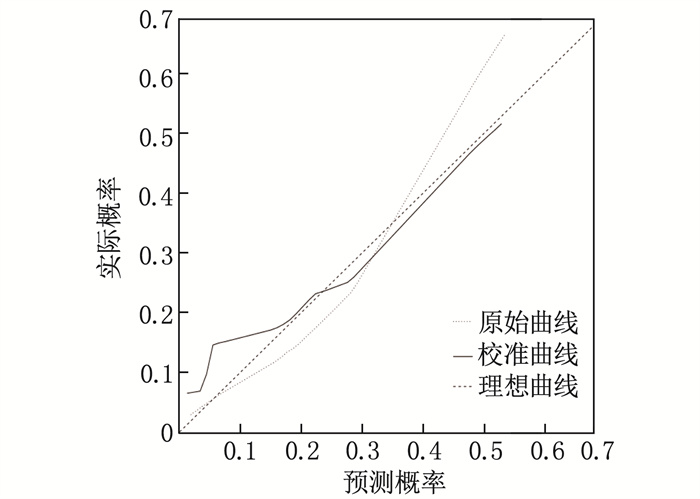
方法回顾性分析439例胃癌患者的临床资料,根据术后2个月内是否发生PGS将患者分成PGS组和对照组。采用Logistic回归分析筛选LRG患者发生PGS的危险因素,并基于筛选结果构建列线图预测模型。通过受试者工作特征(ROC)曲线评估列线图的区分度,通过校准曲线评估列线图的一致性。
结果439例患者中, 52例发生PGS, PGS发生率为11.85%。PGS组年龄≥60岁、伴有糖尿病、有腹部手术史、合并幽门梗阻、手术时间≥4 h及术中吻合方式为B-Ⅱ式的患者占比均高于对照组,差异有统计学意义(P < 0.05)。多因素Logistic回归分析结果显示,伴有糖尿病、有腹部手术史、合并幽门梗阻、手术时间≥4 h、术中吻合方式为B-Ⅱ式是LRG患者发生PGS的危险因素(P < 0.05)。内部验证结果显示, ROC曲线的曲线下面积为0.839(95%CI: 0.773~0.905), 校准曲线拟合良好, Hosmer-Lemeshow拟合优度检验结果为χ2=9.078, P=0.247。
结论伴有糖尿病、有腹部手术史、合并幽门梗阻、手术时间≥4 h、术中吻合方式为B-Ⅱ式是LRG患者发生PGS的危险因素, 基于这些因素构建的列线图能够有效预测LRG患者的PGS发生风险。
Abstract:ObjectiveTo analyze the risk factors for postoperative gastroparesis syndrome (PGS) in gastric cancer patients undergoing laparoscopic radical gastrectomy (LRG) and to construct and validate a nomogram prediction model for PGS.
MethodsThe clinical data of 439 gastric cancer patients were retrospectively analyzed. Patients were divided into PGS group and control group based on whether PGS occurred within 2 months after surgery. Logistic regression analysis was used to screen for risk factors of PGS in LRG patients, and a nomogram prediction model was constructed based on the screening results. The discriminative ability of the nomogram was assessed by the receiver operating characteristic (ROC) curve, and its consistency was evaluated by the calibration curve.
ResultsAmong 439 patients, 52 developed PGS, with an incidence rate of 11.85%. The proportions of patients aged ≥60 years, complicating with diabetes, having a history of abdominal surgery, complicating with pyloric obstruction, having surgery duration ≥4 hours, and intraoperative anastomosis type of B-Ⅱ were higher in the PGS group than those in the control group (P < 0.05). The results of multivariate Logistic regression analysis showed that diabetes, a history of abdominal surgery, pyloric obstruction, surgery duration ≥4 hours, and intraoperative anastomosis type of B-Ⅱ were risk factors for PGS in LRG patients (P < 0.05). Internal validation results showed that the area under the ROC curve was 0.839 (95%CI, 0.773 to 0.905), the calibration curve fitted well, and the Hosmer-Lemeshow goodness-of-fit test result was good(χ2=9.078, P=0.247).
ConclusionDiabetes, a history of abdominal surgery, pyloric obstruction, surgery duration ≥4 hours, and intraoperative anastomosis type of B-Ⅱ are risk factors for PGS in LRG patients. The nomogram constructed based on these factors can effectively predict the risk of PGS in LRG patients.
-
精神分裂症是临床上较为常见的精神类疾病,该病起病较缓慢,病程较长,目前发病机制尚不明确[1-2]。研究[3]认为,精神分裂症的发生与神经营养因子具有一定的相关性,神经营养因子是神经元生存、发育、分化所需要的一种蛋白质分子,其表达异常会导致神经功能障碍,引发认知障碍,最终导致精神疾病的发生。目前,临床上对于精神分裂症的治疗主要以药物为主,但常用的精神类药物仅能控制患者临床症状,并不能达到完全治愈[4]。本研究分析齐拉西酮联合氯丙嗪对老年精神分裂症患者神经营养因子的影响,现报告如下。
1. 资料与方法
1.1 一般资料
选取2017年1月—2019年1月本院收治的100例老年精神分裂症患者,随机分为对照组和联合组,每组50例。对照组男26例,女24例,平均年龄(73.5±2.6)岁,平均病程(10.5±1.6)个月; 联合组男25例,女25例,平均年龄(75.1±2.7)岁,平均病程(10.80±1.5)个月。2组患者一般资料比较,差异无统计学意义(P > 0.05),具有可比性。本研究所有患者均签署了知情同意书。纳入标准: ①患者均符合《国际疾病与相关健康问题统计分类第10版》中精神分裂症的诊断标准; ②患者年龄≥60岁。排除标准: ①合并脑部疾病的患者; ②存在先天性神经疾病的患者; ③合并心肺功能不全的患者; ④合并感染性、内分泌类疾病的患者; ⑤长期接受精神类药物治疗的患者; ⑥长期嗜酒、嗜药的患者。
1.2 方法
对照组患者采用氯丙嗪(国药集团新疆制药有限公司,国药准字H65020271)治疗,初始剂量为50 mg/d, 根据患者疾病控制情况,服用14 d后可增加剂量至600 mg/d。联合组采用氯丙嗪联合齐拉西酮治疗,齐拉西酮(重庆圣华曦药业股份有限公司,国药准字H20070078)初始剂量为40 mg/d, 2次/d, 根据患者疾病控制情况,服用7 d内可将剂量增加至160 mg/d; 氯丙嗪用法用量同对照组。2组患者均连续治疗12周,治疗过程中可酌情给予患者镇静催眠药物、β受体阻滞剂或者苯海索,但不使用其他抗神经类药物。
1.3 评价标准
① 采用阳性与阴性症状量表(PANSS)评价2组患者治疗前后精神症状,包括阳性、阴性、一般精神病理量表,共30个项目,采取百分制,分数越高说明精神症状越严重。采用简明精神状态量表(MMSE)评价2组患者治疗前后认知功能,包括即刻、延时记忆、注意力/计算力、定向力、语言及视空间能力等,总分为30分,分数越低说明患者认知功能障碍越严重。②采用Stroop测验、持续操作测验、数字符号编码测验、连线测验A评价2组患者治疗前后认知功能,分数越低说明患者认知功能越严重。③抽取2组患者治疗前1 d、治疗后1 d清晨空腹静脉血3 mL, 在离心半径5 cm、转速3 000转/min条件下离心处理10 min, 分离上层血清, -80 ℃保存待用。采用酶联免疫吸附试验法检测血清神经生长因子(NGF)、脑源性神经营养因子(BDNF)、神经元特异性烯醇化酶(NSE)、髓鞘碱性蛋白(MBP)、手型钙结合蛋白(S100B)水平。④ 2组患者治疗前后均行标准12导联同步心电图检测,重复测量3次患者的心搏QT、RR间期,并取3次测量的均值为最终值,采用Bazett公式计算校正的QT间期(QTc)。采用日立7170A型全自动生化分析仪检测2组患者治疗前后血钾、血镁水平。⑤根据PANSS评分评价治疗效果,分为痊愈、显效、有效、无效4个等级。痊愈: 临床症状均消失, PANSS评分减少 > 80%; 显效: 临床症状显著好转, PANSS评分减少 > 50%; 有效: 临床症状有所好转, PANSS评分减少 > 25%; 无效: 临床症状无改善,甚至有加重的趋势。总有效率=痊愈率+显效率+有效率。⑥统计2组患者嗜睡、恶心、呕吐、心动过速等不良反应发生情况。
1.4 统计学处理
采用SPSS 20.0统计软件进行数据分析处理。计量资料采用均数±标准差(x±s)描述,组间比较采用独立样本t检验,治疗前后比较采用重复测量方差分析; 计数资料采用频数和百分比表示,组间比较采用X2检验, P < 0.05为差异有统计学意义。
2. 结果
2.1 2组患者PANSS、MMSE评分比较
2组患者治疗前PANSS、MMSE评分比较,差异无统计学意义(P > 0.05); 2组患者治疗后MMSE评分高于治疗前, PANSS评分低于治疗前,且联合组患者MMSE评分高于对照组, PANSS评分低于对照组,差异均有统计学意义(P < 0.05)。见表 1。
表 1 2组患者PANSS、MMSE评分比较(x±s)分 组别 n PANSS MMSE 治疗前 治疗后 治疗前 治疗后 对照组 50 85.46±5.49 56.34±2.38* 15.30±1.10 20.14±2.04* 联合组 50 85.53±5.68 45.26±1.12*# 15.34±1.05 26.58±3.69*# PANSS: 阳性与阴性症状量表; MMSE: 简明精神状态量表。与治疗前比较, *P < 0.05; 与对照组比较, #P < 0.05。 2.2 2组患者认知功能比较
2组患者治疗前认知功能比较,差异无统计学意义(P > 0.05); 2组患者治疗后Stroop测验、持续操作测验、数字符号编码测验评分高于治疗前,连线测验A评分低于治疗前,且联合组患者Stroop测验、持续操作测验、数字符号编码测验评分高于对照组,连线测验A评分低于对照组,差异有统计学意义(P < 0.05)。见表 2。
表 2 2组患者认知功能比较(x±s)分 项目 时点 对照组(n=50) 联合组(n=50) Stroop测验 治疗前 35.26±2.45 35.80±2.43 治疗后 45.37±3.48* 59.68±6.46*# 持续操作测验 治疗前 1.25±0.32 1.26±0.33 治疗后 3.00±0.40* 3.40±0.57*# 数字符号编码测验 治疗前 30.25±5.42 30.30±5.43 治疗后 51.24±6.48* 60.27±8.59*# 连线测验A 治疗前 70.24±8.49 70.25±8.52 治疗后 56.49±5.46* 41.27±3.45*# 与治疗前比较, *P < 0.05; 与对照组比较, #P < 0.05。 2.3 2组患者神经营养因子水平比较
2组患者治疗前神经营养因子水平比较,差异无统计学意义(P > 0.05); 2组患者治疗后NSE、S100B、MBP水平低于治疗前,NGF、BDNF水平高于治疗前,且联合组患者NSE、S100B、MBP水平低于对照组,NGF、BDNF水平高于对照组,差异有统计学意义(P < 0.05)。见表 3。
表 3 2组患者神经营养因子水平比较(x±s)指标 时点 对照组(n=50) 联合组(n=50) NSE/(μg/L) 治疗前 36.25±7.49) 36.26±7.52 治疗后 24.15±2.16* 20.16±1.09*# S100B/(μg/L) 治疗前 65.47±8.47 65.53±8.59 治疗后 49.68±5.14* 30.27±2.42*# MBP/(mg/L) 治疗前 24.59±3.48 25.61±3.52 治疗后 15.98±2.10* 10.27±1.06*# NGF/(pg/mL) 治疗前 31.29±1.45 31.32±1.43 治疗后 38.45±2.10* 46.27±3.49*# BDNF/(μg/L) 治疗前 3.30±0.52 3.32±0.51 治疗后 5.46±0.98* 7.58±1.10*# NSE: 神经元特异性烯醇化酶; S100B: 手型钙结合蛋白;
MBP: 髓鞘碱性蛋白; NGF: 神经生长因子;
BDNF: 脑源性神经营养因子。与治疗前比较, *P < 0.05;
与对照组比较, #P < 0.05。2.4 2组患者心电图、血钾、血镁水平比较
2组患者治疗前QTc、血钾、血镁水平比较,差异无统计学意义(P > 0.05); 2组患者治疗后QTc、血钾、血镁水平高于治疗前,但差异无统计学意义(P > 0.05); 2组患者治疗后的QTc、血钾、血镁比较,差异无统计学意义(P > 0.05)。见表 4。
表 4 2组患者心电图、血钾、血镁水平比较(x±s)组别 n QTc/ms 血钾/(mmol/L) 血镁/(mmol/L) 治疗前 治疗后 治疗前 治疗后) 治疗前 治疗后 对照组 50 425.36±16.35 428.67±16.99 3.92±0.24 3.94±0.26 1.02±0.16 1.04±0.17 联合组 50 425.65±16.23 429.68±17.25 3.93±0.26 3.95±0.25 1.03±0.15 1.05±0.16 QTc: 校正的QT间期。 2.5 2组患者疗效及不良反应比较
联合组患者总有效率高于对照组,差异有统计学意义(P < 0.05),见表 5。联合组总不良反应发生率低于对照组,但差异无统计学意义(P > 0.05), 见表 6。
表 5 2组患者疗效比较组别 n 治愈 显效 有效 无效 总有效率/% 对照组 50 20 9 12 9 82.00 联合组 50 26 13 10 1 95.00* 与对照组比较, *P < 0.05。 表 6 2组患者不良反应发生情况比较组别 n 嗜睡 恶心、呕吐 心动过速 不良反应发生率/% 对照组 50 2 0 1 6.00 联合组 50 2 1 1 8.00 3. 讨论
精神分裂症病情较为复杂,复发率较高,可导致患者日常生活能力、工作能力下降,给患者自身及家庭均带来了较大的负担[5]。氯丙嗪是临床上较为典型的精神类疾病的治疗药物,可拮抗与思维情绪相关的边缘系统的多巴胺受体,发挥安定、镇静的效果[6]。虽然氯丙嗪可治疗精神分裂症,但研究[7]发现单纯接受氯丙嗪治疗的效果并不理想。齐拉西酮属非典型抗精神类药物,可拮抗多巴胺D2受体、5-羟色胺1D受体、5-羟色胺2A受体,具有较高的亲和力,可激动5-羟色胺1D受体[8]。王章元等[9]研究表明,齐拉西酮联合奥氮平可用于老年精神分裂症的治疗,且对患者脂代谢的影响较小。陈莹等[10]研究认为,齐拉西酮胶囊可调控男性青少年首发精神催乳素(PRL)、空腹胰岛素(FINS)敏感性。本研究结果显示,相比单纯应用氯丙嗪治疗的患者,应用两药联合治疗的患者精神症状改善更为显著,提示氯丙嗪、齐拉西酮可能发挥协同作用,改善患者临床症状。
精神分裂症的发生与神经营养因子密切相关, NGF、BDNF属于神经生长因子家族成员,其可促进神经细胞再生,发挥神经保护的作用, NGF、BDNF水平低于正常时可损伤神经可塑性,影响信息传递功能[11]。研究[12-13]发现,当发生精神分裂症后,NGF、BDNF、GDNF水平显著降低,降低程度与患者精神症状严重程度显著相关。精神分裂症患者均伴有不同程度的脑损伤,其临床症状表现为神经髓鞘脱失、神经元破坏或者坏死以及血脑屏障破坏等。目前,临床上多采用NSE、S100B、MBP对脑损伤程度进行评估,当神经元被破坏后,上述因子会经损伤的神经元渗入至脑脊液,经过血脑屏障后进入血液,其水平可反映患者脑损伤程度[14-15]。本研究结果显示, 2组治疗前NGF、BDNF、GDNF、NSE、S100B、MBP均异常表达,提示患者均存在不同程度的神经损伤; 2组治疗后NGF、BDNF、GDNF、NSE、S100B、MBP异常表达均显著改善,且联合组患者改善效果更好,提示两药联合可修复受损神经,达到治愈的目的。
大多数精神分裂症患者处于兴奋应激状态,可能会导致机体电解质紊乱,延长QTc间期,诱发尖端扭转型室速。研究[16]表明,长期使用药物治疗的精神疾病患者伴有不同程度的QTc间期延长,影响电解质平衡。本研究结果显示, 2组患者治疗前后QTc间期、血钾、血镁水平无差异,说明两药联合治疗不会对患者QTc间期、机体电解质产生影响。
综上所述,齐拉西酮联合氯丙嗪可改善老年精神分裂症患者的临床症状,改善NGF、BDNF等神经营养因子的异常表达,修复受损神经元,且不影响患者机体电解质平衡。
-
表 1 LRG患者发生PGS的单因素分析($\overline x $±s)[n(%)]
项目 分类 PGS组(n=52) 对照组(n=387) χ2/t P 体质量指数/(kg/m2) 23.19±2.47 22.83±2.31 1.046 0.296 术中出血量/mL 205.47±37.21 198.89±34.26 1.287 0.199 性别 男 33(63.46) 225(58.14) 0.536 0.464 女 19(36.54) 162(41.86) 年龄 < 60岁 25(48.08) 242(62.53) 4.020 0.045 ≥60岁 27(51.92) 145(37.47) 吸烟史 有 19(36.54) 128(33.07) 0.247 0.619 无 33(63.46) 259(66.93) 饮酒史 有 21(40.38) 113(29.20) 2.705 0.100 无 31(59.62) 274(70.80) 基础疾病 高血压 18(34.62) 111(28.68) 0.778 0.378 糖尿病 17(32.69) 69(17.83) 6.429 0.011 高脂血症 15(28.85) 73(18.86) 2.850 0.091 腹部手术史 有 13(25.00) 45(11.63) 7.149 0.008 无 39(75.00) 342(88.37) 合并幽门梗阻 是 15(28.85) 52(13.44) 8.417 0.004 否 37(71.15) 335(86.56) 术前血红蛋白 < 110 g/L 20(38.46) 131(33.85) 0.432 0.511 ≥110 g/L 32(61.54) 256(66.15) 术前白蛋白 < 35 g/L 14(26.92) 91(23.51) 0.293 0.588 ≥35 g/L 38(73.08) 296(76.49) 术前C反应蛋白 < 10 mg/L 33(63.46) 279(72.09) 1.661 0.197 ≥10 mg/L 19(36.54) 108(27.91) TNM分期 Ⅰ~ⅡA期 15(28.85) 143(36.95) 1.307 0.253 ⅡB~Ⅲ期 37(71.15) 244(63.05) 肿瘤最大径 < 3 cm 14(26.92) 155(40.05) 3.337 0.068 ≥3 cm 38(73.08) 232(59.95) 病灶部位 胃窦 18(34.62) 149(38.50) 0.890 0.641 胃体 11(21.15) 93(24.03) 贲门 23(44.23) 145(37.47) 淋巴结转移 有 33(63.46) 201(51.94) 2.446 0.118 无 19(36.54) 186(48.06) 手术时间 < 4 h 20(38.46) 231(59.69) 8.437 0.004 ≥4 h 32(61.54) 156(40.31) 术中吻合方式 B-Ⅰ式 25(48.08) 269(69.51) 9.519 0.002 B-Ⅱ式 27(51.92) 118(30.49) 术后使用镇痛泵 是 28(53.85) 163(42.12) 2.565 0.109 否 24(46.15) 224(57.88) 表 2 变量赋值方式
变量 赋值方式 年龄 < 60岁=1, ≥60岁=2 伴有糖尿病 否=0, 是=1 腹部手术史 无=0, 有=1 合并幽门梗阻 否=0, 是=1 手术时间 < 4 h=1, ≥4 h=2 术中吻合方式 BⅠ式=1, B-Ⅱ式=2 表 3 LRG患者发生PGS的多因素Logistic回归分析
变量/参照 B SE Wald χ2 P OR 95%CI 伴有糖尿病 1.062 0.343 9.601 0.002 2.894 1.478~5.666 有腹部手术史 1.684 0.446 14.229 < 0.001 5.385 2.245~12.916 合并幽门梗阻 1.795 0.415 18.686 < 0.001 6.022 2.668~13.593 手术时间≥4 h 1.601 0.359 19.905 < 0.001 4.957 2.454~10.015 术中吻合方式为B-Ⅱ式 1.596 0.399 15.975 < 0.001 4.934 2.256~10.794 常数项 -4.346 0.447 94.545 < 0.001 0.013 — -
[1] LI G Z, DOHERTY G M, WANG J P. Surgical management of gastric cancer: a review[J]. JAMA Surg, 2022, 157(5): 446-454. doi: 10.1001/jamasurg.2022.0182
[2] HUANG C M, LIU H, HU Y F, et al. Laparoscopic vs open distal gastrectomy for locally advanced gastric cancer: five-year outcomes from the CLASS-01 randomized clinical trial[J]. JAMA Surg, 2022, 157(1): 9-17. doi: 10.1001/jamasurg.2021.5104
[3] 张博, 赵刚, 钟先鸿. 胃癌术后胃瘫综合征患者中医证素分布规律与胃瘫症状严重程度(分级)相关性的研究[J]. 世界中西医结合杂志, 2023, 18(7): 1386-1390. [4] 赵伟鹏, 姜欣, 黄金昶. 胃周穴位温针灸治疗肿瘤术后胃瘫综合征临床观察[J]. 中华中医药杂志, 2021, 36(7): 4379-4382. [5] WANG Z, SHI Y X, ZHANG L L, et al. Nomogram for predicting swallowing recovery in patients after dysphagic stroke[J]. JPEN J Parenter Enteral Nutr, 2022, 46(2): 433-442. doi: 10.1002/jpen.2115
[6] 严小丽, 黄革, 阎萍, 等. 超声评分系统联合临床特征列线图预测凶险性前置胎盘患者产后出血[J]. 中国医学影像技术, 2024, 40(3): 401-406. [7] CAMILLERI M, PARKMAN H P, SHAFI M A, et al. Clinical guideline: management of gastroparesis[J]. Am J Gastroenterol, 2013, 108(1): 18-37. doi: 10.1038/ajg.2012.373
[8] 杨玉兵, 张海洋, 史娟, 等. 胃癌患者行腹腔镜胃癌根治术后发生胃瘫综合征的危险因素分析[J]. 癌症进展, 2023, 21(15): 1699-1701. [9] 陈烈欢, 程龙庆, 彭翔, 等. 腹腔镜远端胃癌根治术后胃瘫综合征的危险因素及对患者预后影响分析[J]. 实用中西医结合临床, 2019, 19(12): 51-53. [10] 杜耀, 张江南, 李卫平, 等. 远端胃癌根治性切除术后PGS发生的危险因素及风险预测模型的建立和评价[J]. 山东医药, 2018, 58(28): 74-77. doi: 10.3969/j.issn.1002-266X.2018.28.020 [11] 朱兴业, 张亮, 郭腾龙, 等. 预测右半结肠癌术后胃瘫危险因素列线图模型的建立[J]. 中国现代普通外科进展, 2022, 25(9): 734-737, 746. [12] 陈贝. 根治性远端胃大部切除术对胃癌患者的临床效果及术后胃瘫综合征的高危因素分析[J]. 实用癌症杂志, 2023, 38(9): 1498-1501. doi: 10.3969/j.issn.1001-5930.2023.09.027 [13] 王娜, 周勇, 李卡. 肠道菌群与腹部手术后胃肠功能障碍的相关性研究进展[J]. 中国普外基础与临床杂志, 2022, 29(2): 248-254. [14] 梁延洋, 张春旭, 楚理家. 腹腔镜远端胃癌根治Billroth Ⅰ式吻合术后胃瘫综合征相关因素分析[J]. 河南外科学杂志, 2023, 29(6): 93-95. [15] 王雄飞, 刘春庆, 邵建平, 等. 腹腔镜胃癌根治术后胃瘫综合征的危险因素分析[J]. 武汉大学学报: 医学版, 2022, 43(3): 423-426. [16] 陈颖, 胡丹红, 郑子越. 胰十二指肠术后胃瘫的临床特征及危险因素分析[J]. 海南医学, 2023, 34(19): 2788-2791. doi: 10.3969/j.issn.1003-6350.2023.19.010 [17] 谈利. 胃癌根治术后胃排空延迟的相关危险因素分析[J]. 河南外科学杂志, 2023, 29(1): 73-75. [18] 中国研究型医院学会, 丁世康, 叶辉, 等. 中国肿瘤患者术后胃瘫诊治中西医结合专家共识(2022版)[J]. 中国中西医结合消化杂志, 2023, 31(3): 188-191. doi: 10.3969/j.issn.1671-038X.2023.03.07 [19] 高伟, 李涛, 席锐, 等. 不同吻合方式对经典胰十二肠切除术后胃排空障碍的临床疗效观察[J]. 局解手术学杂志, 2020, 29(6): 501-504. -
期刊类型引用(10)
1. 周彩凤,崔万花. 信迪利单抗联合TP化疗方案治疗对晚期非小细胞肺癌患者肿瘤标志物和免疫平衡的影响. 中国医学创新. 2024(28): 121-124 .  百度学术
百度学术
2. 樊宁. 血管内皮生长因子和肿瘤标志物对肺癌分期的诊断价值分析. 临床研究. 2023(06): 10-13 .  百度学术
百度学术
3. 雷小平,孙雅菊. 参芪扶正注射液在晚期非小细胞肺癌患者治疗中的效果. 中国医药导刊. 2023(04): 425-429 .  百度学术
百度学术
4. 吴西,张家艳,殷俊,杨春茂. 免疫治疗联合含铂双药治疗肺腺癌疗效及对患者短期生存的影响. 北华大学学报(自然科学版). 2023(05): 617-621 .  百度学术
百度学术
5. 杜晓丹,徐维国,朱静,李琳,吴君华. 嘌呤能型2受体家族X7嘌呤受体高表达与可切除非小细胞肺癌患者临床病理特征及预后的相关性研究. 实用临床医药杂志. 2022(10): 77-82 .  本站查看
本站查看
6. 柳芳美,凡国华,徐金静,王庆,杨俊俊,闵凌峰,张梦,吴书清. 中性粒细胞与淋巴细胞比值在非小细胞肺癌合并阻塞性睡眠呼吸暂停低通气综合征患者中的临床意义. 实用临床医药杂志. 2022(15): 45-49 .  本站查看
本站查看
7. 冯雨,崔东,张会民,刘渊源,李瑞杰,栾加强,徐明星,钱如林. 外周血循环肿瘤细胞联合血清肿瘤标志物检测在非小细胞肺癌患者中的临床意义. 实用医院临床杂志. 2022(06): 31-33 .  百度学术
百度学术
8. 周明锴. 四项血清指标联合检测在鉴别诊断NSCLC中的价值分析. 实验与检验医学. 2021(03): 655-657+687 .  百度学术
百度学术
9. 杨明,邢坤,袁五营,杜佳辉,白杨. 非小细胞肺癌组织错配切除修复蛋白1、核苷酸还原酶M1和乳腺癌易感基因1的表达与预后的关系. 实用医院临床杂志. 2021(05): 43-47 .  百度学术
百度学术
10. 杨旭,朱德兵,王巍炜,唐明伟,钱俊. 5种肿瘤标志物在非小细胞肺癌中的诊断价值. 临床医学研究与实践. 2021(34): 28-32 .  百度学术
百度学术
其他类型引用(2)




 下载:
下载:

 苏公网安备 32100302010246号
苏公网安备 32100302010246号
