Risk factor analysis and personalized prevention strategies for renal anemia in hemodialysis patients with end-stage kidney disease
-
摘要:目的
探讨终末期肾脏病(ESKD)血液透析患者肾性贫血的危险因素。
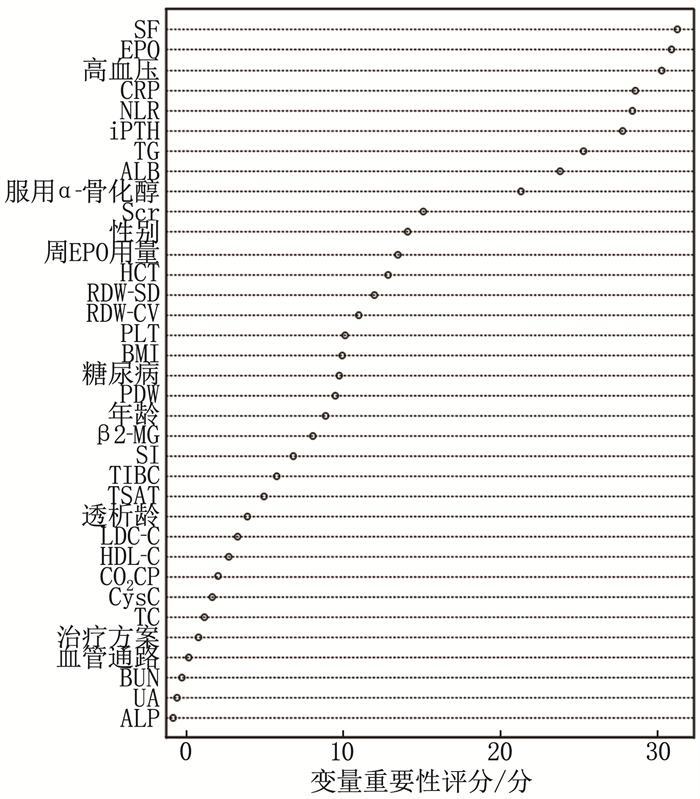
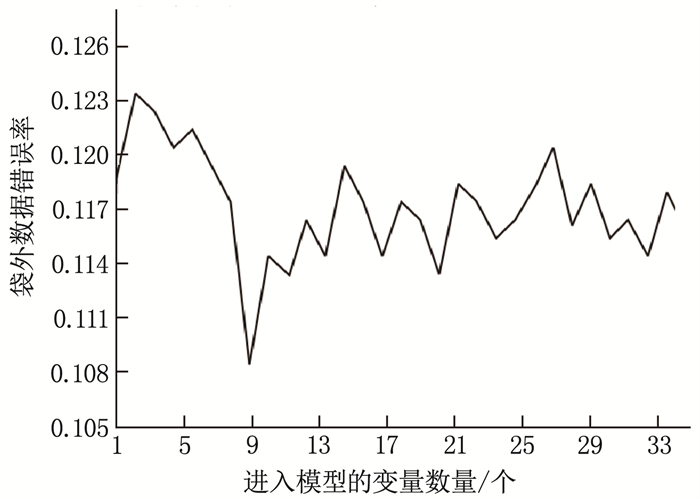
方法回顾性选取2021年12月—2022年12月于本院行血液透析治疗的148例ESKD患者作为研究对象, 根据血红蛋白(Hb)水平的不同及肾性贫血诊断标准将患者分为肾性贫血组(86例)和非贫血组(62例)。比较2组临床资料。采用随机森林算法及多因素Logistic回归分析筛选影响肾性贫血的因素,并建立多因素Logistic回归模型,同时采用十字交叉试验验证模型的稳定性。建立风险分层系统,并根据X-Tile软件获得的截断值对患者进行风险分层。采用受试者工作特征(ROC)曲线评价多因素Logistic回归模型和风险分层系统的区分度。
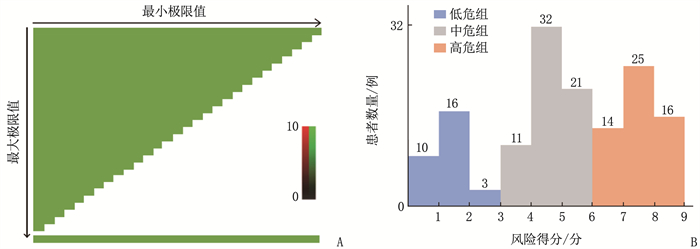
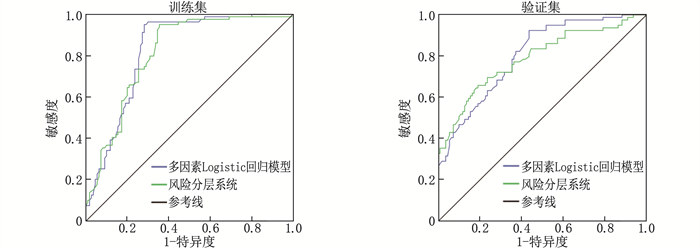
结果148例ESKD患者中,肾性贫血发生率为58.11%(86/148); 高血压、中性粒细胞与淋巴细胞比值(NLR)增加、C反应蛋白(CRP)升高、血清铁蛋白(SF)升高、全段甲状旁腺激素(iPTH)升高是影响患者肾性贫血发生的危险因素(P < 0.05), 服用α-骨化醇、促红细胞生成素(EPO)升高、甘油三酯(TG)升高、血清白蛋白(ALB)升高是保护因素(P < 0.05)。多因素Logistic回归模型的拟合优度检验结果显示Nagelkerke R2=0.593。根据X-Tile软件获得风险评分的截断值,将患者分为低危组(< 4分, 29例)、中危组(4~ < 7分, 64例)和高危组(≥7分, 55例), 肾性贫血发生率分别为24.14%、57.81%和76.36%。3组肾性贫血发生率比较,差异有统计学意义(P < 0.001)。训练集中多因素Logistic回归模型和风险分层系统的ROC曲线的曲线下面积分别为0.826、0.811, 验证集中分别为0.804和0.789。
结论ESKD血液透析患者肾性贫血的发生受高血压、NLR、CRP等诸多因素的影响。
Abstract:ObjectiveTo explore the risk factors for renal anemia in hemodialysis patients with end-stage kidney disease (ESKD).
MethodsA total of 48 ESKD patients undergoing hemodialysis in our hospital from December 2021 to December 2022 were selected as study objects. They were divided into renal anemia group (86 cases) and non-anemia group (62 cases) based on hemoglobin (Hb) levels and diagnostic criteria for renal anemia. Clinical data between the two groups were compared. Random forest algorithm and multivariate Logistic regression analysis were used to screen for factors influencing renal anemia, and a multivariate Logistic regression model was established. Cross-validation was also employed to verify the stability of the model. A risk stratification system was developed, and patients were stratified based on cut-off values obtained from X-Tile software. The areas under the receiver operating characteristic (ROC) curves were used to evaluate the discrimination ability of the multivariate Logistic regression model and the risk stratification system.
ResultsAmong 148 ESKD patients, the incidence of renal anemia was 58.11% (86/148). Hypertension, increased neutrophil-to-lymphocyte ratio (NLR), elevated C-reactive protein (CRP), increased serum ferritin (SF), and elevated intact parathyroid hormone (iPTH) were identified as risk factors for renal anemia (P < 0.05). Administration of α-calcidol, increased erythropoietin (EPO), elevated triglyceride (TG), and increased serum albumin (ALB) were protective factors (P < 0.05). The goodness-of-fit test for the multivariate Logistic regression model showed a Nagelkerke R2 of 0.593. Based on the cut-off values for risk scores obtained from X-Tile software, patients were stratified into low-risk group (< 4 points, 29 cases), medium-risk group (4 to < 7 points, 64 cases), and high-risk group (≥7 points, 55 cases), with renal anemia incidence rates of 24.14%, 57.81%, and 76.36%, respectively. The difference in renal anemia incidence rates among the three groups was statistically significant (P < 0.001). In the training set, the areas under the ROC curves for the multivariate Logistic regression model and the risk stratification system were 0.826 and 0.811, respectively, and were 0.804 and 0.789, respectively in the validation set.
ConclusionThe occurrence of renal anemia in hemodialysis patients with ESKD is influenced by various factors, including hypertension, NLR, CRP, etc.
-
-
表 1 2组患者临床资料比较(x±s)[n(%)]
指标 分类 非贫血组(n=62) 肾性贫血组(n=86) t/χ2 P 性别 男 30(48.39) 49(56.98) 1.068 0.301 女 32(51.61) 37(43.02) 年龄/岁 54.87±10.08 55.12±9.93 0.150 0.881 体质量指数/(kg/m2) 23.62±2.13 23.48±2.02 0.407 0.685 糖尿病 20(32.26) 30(34.88) 0.111 0.739 高血压 46(74.19) 76(88.37) 5.001 0.025 治疗方案 血液透析 40(64.52) 66(76.74) 2.673 0.263 血液透析+血液透析滤过 18(29.03) 16(18.60) 血液透析+血液透析滤过+血液灌流 4(6.45) 4(4.65) 血管通路 临时导管 4(6.45) 5(5.81) 0.194 0.907 长期导管 7(11.29) 8(9.30) 动静脉内瘘 51(82.26) 73(84.88) 透析龄/月 38.39±7.62 35.91±8.04 1.892 0.060 促红细胞生成素/(mIU/mL) 18.53±3.89 5.62±2.81 23.450 < 0.001 1周促红细胞生成素用量/(U/kg) 134.06±28.15 137.62±26.47 0.786 0.433 服用α-骨化醇 56(90.32) 48(55.81) 20.536 < 0.001 总胆固醇/(mmol/L) 3.88±1.12 3.59±1.05 1.612 0.109 甘油三酯/(mmol/L) 1.65±0.53 1.42±0.49 2.722 0.007 低密度脂蛋白胆固醇/(mmol/L) 2.40±0.92 2.18±0.73 1.621 0.107 高密度脂蛋白胆固醇/(mmol/L) 1.05±0.25 0.96±0.31 1.886 0.061 白蛋白/(g/L) 31.42±7.32 28.06±6.95 2.838 0.005 红细胞比容/% 0.36±0.11 0.32±0.14 1.871 0.063 红细胞分布宽度标准差 48.52±9.17 48.39±8.55 0.089 0.930 红细胞分布宽度变异系数 14.44±2.72 14.29±2.45 0.351 0.726 血小板/(×109/L) 183.96±77.02 180.65±72.38 0.267 0.790 血小板分布宽度/% 12.21±2.39 11.58±2.42 1.571 0.118 中性粒细胞与淋巴细胞比值/% 3.31±1.12 5.46±2.35 6.674 < 0.001 C反应蛋白/(mg/L) 11.64±2.39 15.08±3.72 6.389 < 0.001 血尿素氮/(mmol/L) 22.73±4.62 23.15±4.89 0.527 0.599 血肌酐/(mmol/L) 912.37±206.45 903.51±217.66 0.250 0.803 尿酸/(μmol/L) 418.92±89.72 406.53±90.28 0.826 0.410 β2-微球蛋白/(mg/L) 30.42±7.55 30.76±7.68 0.268 0.789 胱抑素C/(mg/L) 5.58±1.42 5.39±1.55 0.762 0.447 碱性磷酸酶/(U/L) 84.22±19.06 79.78±25.39 1.161 0.248 二氧化碳结合力/% 21.04±3.45 21.83±3.71 1.316 0.190 总铁结合力/% 45.39±19.07 41.15±22.18 1.216 0.226 血清铁/(μmol/L) 13.18±4.02 12.25±3.91 1.411 0.160 血清铁蛋白/(μg/L) 178.69±39.64 218.72±47.06 5.447 < 0.001 转铁蛋白饱和度/% 26.42±7.47 24.83±8.01 1.225 0.222 全段甲状旁腺激素/(pg/mL) 316.82±72.31 562.93±99.58 16.560 < 0.001 表 2 多因素Logistic回归分析筛选影响ESKD血液透析患者肾性贫血的因素
因素 β SE Wald χ2 P OR(95%CI) 高血压 1.465 0.485 9.124 0.001 4.326(3.872~4.903) 服用α-骨化醇 -0.666 0.402 2.745 0.046 0.514(0.175~0.864) EPO升高 -0.891 0.637 1.956 0.027 0.410(0.134~0.764) TG升高 -0.955 0.612 2.435 0.023 0.385(0.102~0.667) ALB升高 -0.860 0.651 1.745 0.037 0.423(0.106~0.742) NLR增加 1.354 0.569 5.663 0.010 3.871(3.255~4.369) CRP升高 1.380 0.513 7.236 0.003 3.975(3.084~4.902) SF升高 1.519 0.438 12.027 < 0.001 4.569(3.705~5.362) iPTH升高 1.184 0.593 3.987 0.017 3.266(2.885~3.711) 表 3 不同肾性贫血概率模型对肾性贫血的预测效果
概率 准确度/% 敏感度/% 特异度/% 假阳性率/% 假阴性率/% 约登指数 0.95 77.82 87.12 77.31 65.02 2.49 64.43 0.90 80.14 87.04 80.69 59.27 2.50 67.73 0.85 85.09 86.59 85.52 55.02 3.12 72.11 0.80 93.77 86.42 92.85 41.28 3.27 79.27 0.75 93.29 86.21 92.06 36.43 3.47 78.27 0.70 92.81 83.63 93.17 32.79 4.22 76.80 0.65 93.08 80.24 93.85 30.36 4.39 74.09 0.60 92.37 78.23 93.43 29.57 5.21 71.66 0.55 93.56 75.06 93.39 28.12 5.69 68.45 0.50 94.01 70.18 94.08 37.43 6.31 64.26 0.45 93.72 67.93 94.26 24.11 6.45 62.19 0.40 93.28 66.86 96.32 22.38 6.82 63.18 0.35 93.15 60.95 97.28 20.09 7.15 58.23 0.30 90.79 57.13 98.17 18.73 7.29 55.30 0.25 87.62 54.39 99.24 13.46 8.05 53.63 0.20 87.13 47.12 99.83 7.02 8.78 46.95 0.15 86.05 32.45 99.69 4.28 9.42 32.14 0.10 85.44 19.76 100.00 < 0.01 10.13 19.76 0.05 86.07 < 0.01 100.00 < 0.01 10.59 < 0.01 表 4 十字交叉试验验证模型预测肾性贫血的稳定性
% 模型 准确度 敏感度 特异度 假阳性率 假阴性率 训练集 93.77 86.42 92.85 41.28 3.27 验证集 92.34 85.66 92.37 40.65 3.59 -
[1] JANKOWSKI J, FLOEGE J, FLISER D, et al. Cardiovascular disease in chronic kidney disease: pathophysiological insights and therapeutic options[J]. Circulation, 2021, 143(11): 1157-1172. doi: 10.1161/CIRCULATIONAHA.120.050686
[2] LIU P, QUINN R R, LAM N N, et al. Accounting for age in the definition of chronic kidney disease[J]. JAMA Intern Med, 2021, 181(10): 1359-1366. doi: 10.1001/jamainternmed.2021.4813
[3] GERRITS T, BROUWER I J, DIJKSTRA K L, et al. Endoglin is an important mediator in the final common pathway of chronic kidney disease to end-stage renal disease[J]. Int J Mol Sci, 2022, 24(1): 646. doi: 10.3390/ijms24010646
[4] WANG X F, SHI Q Y, MO Y Z, et al. Palliative care needs and symptom burden in younger and older patients with end-stage renal disease undergoing maintenance hemodialysis: a cross-sectional study[J]. Int J Nurs Sci, 2022, 9(4): 422-429.
[5] GONG Y, XIE L Y, YU S Q. Long-term In-center nocturnal hemodialysis improves renal Anemia and malnutrition and life quality of older patients with chronic renal failure[J]. Clin Interv Aging, 2022, 17: 915-923. doi: 10.2147/CIA.S358472
[6] TSAI M H, SU F Y, CHANG H Y, et al. The effect of statin on Anemia in patients with chronic kidney disease and end-stage kidney disease: a systematic review and meta-analysis[J]. J Pers Med, 2022, 12(7): 1175. doi: 10.3390/jpm12071175
[7] KU E, DEL VECCHIO L, ECKARDT K U, et al. Novel anemia therapies in chronic kidney disease: conclusions from a Kidney Disease: improving Global Outcomes (KDIGO) Controversies Conference[J]. Kidney Int, 2023, 104(4): 655-680. doi: 10.1016/j.kint.2023.05.009
[8] 孙雪峰. 《中国肾性贫血诊疗的临床实践指南》解读[J]. 中国实用内科杂志, 2021, 41(9): 785-788. [9] UMBOH O, MOIES E S, PALAR S. The effect of Anemia and hypoalbuminemia on six-months hospitalization risk in end stage chronic kidney disease patients undergoing hemodialysis: a retrospective cohort study[J]. Acta Med Indones, 2023, 55(2): 136-141.
[10] AGORO R, WHITE K E. Anemia and fibroblast growth factor 23 elevation in chronic kidney disease: homeostatic interactions and emerging therapeutics[J]. Curr Opin Nephrol Hypertens, 2022, 31(4): 320-325. doi: 10.1097/MNH.0000000000000797
[11] GUTIÉRREZ O M. Treatment of iron deficiency Anemia in CKD and end-stage kidney disease[J]. Kidney Int Rep, 2021, 6(9): 2261-2269. doi: 10.1016/j.ekir.2021.05.020
[12] RASHIDI A, GARIMELLA P S, AL-ASAAD A, et al. Anemia management in the cancer patient with CKD and end-stage kidney disease[J]. Adv Chronic Kidney Dis, 2022, 29(2): 180-187. e1. doi: 10.1053/j.ackd.2022.03.005
[13] 王静, 温向琼, 康婷, 等. 维持性血液透析患者肾性贫血与中性粒细胞/淋巴细胞比值的相关性[J]. 西部医学, 2023, 35(2): 242-246. doi: 10.3969/j.issn.1672-3511.2023.02.017 [14] 李霞, 陈育青. 影响维持性血液透析患者促红细胞生成素抵抗的因素分析[J]. 重庆医学, 2022, 51(9): 1554-1557. doi: 10.3969/j.issn.1671-8348.2022.09.024 [15] 刘海飞, 赵晓倩, 李兆婷, 等. 老年维持性血液透析病人肾性贫血现状调查及影响因素分析[J]. 实用老年医学, 2022, 36(4): 345-349. [16] 韩蓓, 韩俊岭, 曹靖昊, 等. 全段成纤维细胞生长因子23与维持性血液透析患者肾性贫血的相关性研究[J]. 实用临床医药杂志, 2021, 25(21): 114-118. doi: 10.7619/jcmp.20213812 [17] 吕晴, 陈卫东, 刘磊. 维持性血液透析患者肾性贫血的多因素分析及相关性研究[J]. 中华全科医学, 2021, 19(5): 871-874. [18] 朱燕. 长期维持性血液透析患者发生肾性贫血的危险因素分析[J]. 现代医学与健康研究电子杂志, 2022, 6(14): 24-26.




 下载:
下载:
 苏公网安备 32100302010246号
苏公网安备 32100302010246号
