Changes of interleukin-34 levels in serum and bronchoalveolar lavage fluid of patients with severe pneumonia and their prognostic value
-
摘要:目的
探讨重症肺炎患者血清和肺泡灌洗液中白细胞介素-34(IL-34)水平变化及其对预后的评估价值。
方法选取66例重症肺炎患者(重症肺炎组)、35例非重症肺炎患者(非重症肺炎组)、27名健康体检成人(对照组)作为研究对象, 并根据28 d生存情况将重症肺炎组患者进一步分为存活组38例和死亡组28例,分析各组对象的临床资料。绘制受试者工作特征(ROC)曲线,评估血清IL-34和肺泡灌洗液IL-34基因相对表达量对重症肺炎患者28 d内死亡的预测效能,并评估血清IL-34对重症肺炎的预测效能; 绘制Kaplan-Meier生存曲线,采用Logrank检验比较累积生存率; 采用Cox回归分析探讨重症肺炎患者28 d内死亡的危险因素。采用Pearson相关性分析法分析重症肺炎患者血清IL-34水平与肺泡灌洗液IL-34基因相对表达量的相关性。
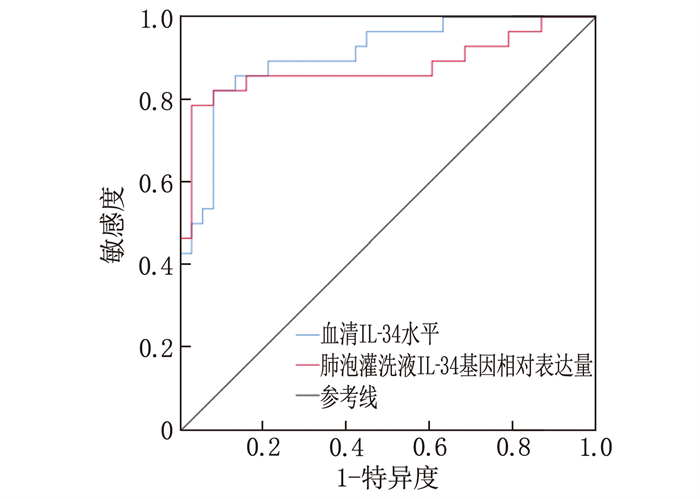
结果重症肺炎组血清IL-34水平高于非重症肺炎组,且非重症肺炎组血清IL-34水平高于对照组,差异有统计学意义(P < 0.05); 死亡组血清IL-34水平、肺泡灌洗液IL-34基因相对表达量均高于存活组,差异有统计学意义(P < 0.05)。ROC曲线分析结果显示,血清IL-34水平、肺泡灌洗液IL-34基因相对表达量预测重症肺炎患者28 d内死亡的曲线下面积分别为0.908、0.878; 血清IL-34水平预测重症肺炎的最佳截断值为129.9 pg/mL。多因素Cox回归分析结果显示,血清IL-34水平升高、肺泡灌洗液IL-34基因相对表达量增加是重症肺炎患者28 d内死亡的独立危险因素(P < 0.05)。Kaplan-Meier生存分析结果显示,以129.9 pg/mL为截断值,血清IL-34高水平的重症肺炎患者的累积生存率低于IL-34低水平患者,差异有统计学意义(Log-rank P < 0.001)。
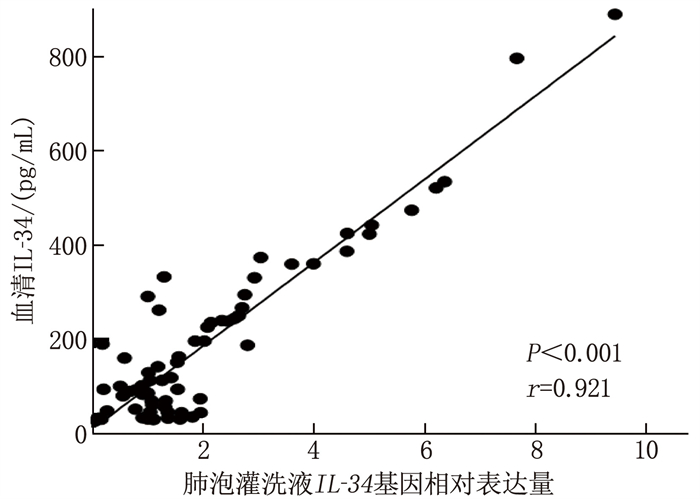
结论重症肺炎患者的血清IL-34水平显著升高,且肺泡灌洗液中IL-34基因相对表达量与血清IL-34水平呈正相关,两者均可作为预测重症肺炎患者28 d内死亡预后的指标。
Abstract:ObjectiveTo investigate the changes in interleukin-34 (IL-34)levels in serum and bronchoalveolar lavage fluid (BALF) of patients with severe pneumonia and their prognostic value.
MethodsA total of 66 patients with severe pneumonia (severe pneumonia group), 35 patients with non-severe pneumonia (non-severe pneumonia group), and 27 healthy adults (control group) were enrolled. The severe pneumonia group was further divided into survival group of 38 patients and non-survival group of 28 patients based on 28-day survival. Clinical data of all subjects were analyzed. Receiver operating characteristic (ROC) curves were plotted to assess the predictive power of serum IL-34 and relative IL-34 gene expression in BALF for 28-day mortality in patients with severe pneumonia, as well as the predictive power of serum IL-34 for severe pneumonia. Kaplan-Meier survival curves were plotted, and the Log-rank test was used to compare cumulative survival rates. Cox regression analysis was conducted to explore risk factors for 28-day mortality in patients with severe pneumonia. Pearson correlation analysis was used to assess the correlation between serum IL-34 levels and relative IL-34 gene expression in BALF of patients with severe pneumonia.
ResultsSerum IL-34 levels were higher in the severe pneumonia group than those in the non-severe pneumonia group, and were higher in the non-severe pneumonia group than in the control group (P < 0.05). Serum IL-34 levels and relative IL-34 gene expression in BALF were higher in the non-survival group than in the survival group (P < 0.05). ROC curve analysis showed that the areas under the curve for predicting 28-day mortality in patients with severe pneumonia were 0.908 for serum IL-34 levels and 0.878 for relative IL-34 gene expression in BALF. The optimal cutoff value for serum IL-34 levels in predicting severe pneumonia was 129.9 pg/mL. Multivariate Cox regression analysis showed that increased serum IL-34 levels and increased relative IL-34 gene expression in BALF were independent risk factors for 28-day mortality in patients with severe pneumonia (P < 0.05). The Kaplan-Meier survival analysis results indicate that, with a cutoff value of 129.9 pg/mL, patients with severe pneumonia who had high serum levels of IL-34 exhibited a lower cumulative survival rate compared to those with low IL-34 level(Log-rank P < 0.001).
ConclusionSerum IL-34 levels are significantly increased in patients with severe pneumonia, and relative IL-34 gene expression in BALF is positively correlated with serum IL-34 levels. Both can be used as indicators for predicting the prognosis of 28-day mortality in patients with severe pneumonia.
-
Keywords:
- severe pneumonia /
- bronchoalveolar lavage fluid /
- interleukin-34 /
- prognosis
-
-
表 1 引物序列
引物名称 方向 引物序列(5′→3′) IL-34 正向 GCCACCCATCCTGGAAGTA 反向 GCCGCATACTGCAATGAGG GAPDH 正向 AGGGCTGCTTTTAACTCTGGT 反向 CCCCACTTGATTTTGGAGGGA 表 2 存活组与死亡组重症肺炎患者的临床资料比较(x±s)[n(%)][M(P25, P75)]
项目 分类 存活组(n=38) 死亡组(n=28) t/χ2/Z P 年龄/岁 64.8±16.8 70.5±14.3 -1.449 0.153 性别 男 31(81.6) 20(71.4) 0.946 0.331 女 7(18.4) 8(28.6) 机械通气 有 27(71.1) 22(78.6) 0.477 0.490 无 11(28.9) 6(21.4) 肺炎类型 社区获得性肺炎 22(57.9) 18(64.3) 0.276 0.599 医院获得性肺炎 16(42.1) 10(35.7) 合并症 慢性阻塞性肺疾病 1(2.6) 2(7.1) 0.749 0.387 高血压病 18(47.4) 19(67.9) 2.747 0.097 糖尿病 8(21.1) 11(39.3) 2.614 0.106 慢性心功能不全 7(18.4) 9(32.1) 1.653 0.199 慢性肝病 8(21.1) 10(35.7) 1.747 0.186 慢性肾病 10(26.3) 14(50.0) 3.908 0.048 脑卒中 7(18.4) 7(25.0) 0.418 0.518 癫痫 4(10.5) 2(7.1) 0.228 0.633 实验室指标 白细胞/(×109/L) 10.6±4.0 11.1±5.8 -0.441 0.661 中性粒细胞/(×109/L) 8.7±3.8 9.2±5.2 -0.506 0.614 淋巴细胞/(×109/L) 1.0±0.6 1.0±0.5 -0.398 0.692 单核细胞/(×109/L) 0.8±0.4 0.8±0.6 -0.073 0.942 血清尿素氮/(mmol/L) 9.2±5.0 13.3±11.3 -1.820 0.077 C反应蛋白/(mg/L) 90.4(31.6, 170.0) 83.1(32.2, 149.5) -0.050 0.960 降钙素原/(ng/mL) 0.6(0.2, 1.6) 1.8(0.4, 3.3) -1.640 0.112 血清IL-34/(pg/mL) 72.0(35.4, 115.0) 281.2(204.4, 424.8) -6.061 < 0.001 肺泡灌洗液IL-34基因相对表达量 1.1(0.8, 1.4) 2.7(2.0, 4.9) -5.509 < 0.001 PSI评分/分 129.2±37.2 155.1±32.8 -2.940 0.005 IL-34: 白细胞介素-34; PSI: 肺炎严重指数。 表 3 重症肺炎组、非重症肺炎组与对照组的临床资料比较(x±s)[n(%)][M(P25, P75)]
项目 重症肺炎组(n=66) 非重症肺炎组(n=35) 对照组(n=27) χ2/F P 年龄/岁 67.2±15.9 69.2±17.1 65.6±11.4 0.413 0.662 性别 男 51(77.3) 23(65.7) 17(63.0) 2.588 0.274 女 15(22.7) 12(34.3) 10(37.0) 白细胞/(×109/L) 10.8±4.8 9.9±2.8 6.2±1.4 14.506 < 0.001 中性粒细胞/(×109/L) 8.9±4.4 2.8±2.2 3.4±1.0 47.236 < 0.001 淋巴细胞/(×109/L) 1.0±0.6 0.8±0.7 2.1±0.6 36.831 < 0.001 单核细胞/(×109/L) 0.8±0.5 0.4±0.2 0.4±0.1 15.453 < 0.001 血清尿素氮/(mmol/L) 10.9±8.5 5.9±2.4 6.3±1.3 9.480 < 0.001 血清IL-34/(pg/mL) 124.6(55.2, 273.3) 109.9(48.0, 147.9) 75.3(29.9, 110.3) 9.277 < 0.001 表 4 重症肺炎患者28 d内死亡的单因素和多因素Cox回归分析
因素 单因素分析 多因素分析 OR Wald χ2 P OR Wald χ2 P 年龄 1.029 4.097 0.043 1.012 0.375 0.540 降钙素原 1.008 1.256 0.262 — — — C反应蛋白 1.000 0.014 0.907 — — — 血清IL-34 1.014 40.189 < 0.001 1.007 4.152 0.042 肺泡灌洗液IL-34基因相对表达量 6.315 40.712 < 0.001 5.142 20.594 < 0.001 PSI评分 1.011 6.514 0.011 1.007 0.919 0.338 -
[1] 中华医学会呼吸病学分会. 中国成人社区获得性肺炎诊断和治疗指南(2016年版)[J]. 中华结核和呼吸杂志, 2016, 39(4): 253-279. doi: 10.3760/cma.j.issn.1001-0939.2016.04.005 [2] 中华医学会呼吸病学分会感染学组. 中国成人医院获得性肺炎与呼吸机相关性肺炎诊断和治疗指南(2018年版)[J]. 中华结核和呼吸杂志, 2018, 41(4): 255-280. doi: 10.3760/cma.j.issn.1001-0939.2018.04.006 [3] WANG Y M, SZRETTER K J, VERMI W, et al. IL-34 is a tissue-restricted ligand of CSF1R required for the development of Langerhans cells and microglia[J]. Nat Immunol, 2012, 13(8): 753-760. doi: 10.1038/ni.2360
[4] BAGHDADI M, ENDO H, TAKANO A, et al. High co-expression of IL-34 and M-CSF correlates with tumor progression and poor survival in lung cancers[J]. Sci Rep, 2018, 8(1): 418. doi: 10.1038/s41598-017-18796-8
[5] KUZUMI A, YOSHIZAKI A, TOYAMA S, et al. Serum interleukin-34 levels in patients with systemic sclerosis: clinical association with interstitial lung disease[J]. J Dermatol, 2018, 45(10): 1216-1220. doi: 10.1111/1346-8138.14538
[6] 林玉霞, 陈名智. ROX指数、淋巴细胞指标、血糖对重症肺炎经鼻高流量氧疗后再次气管插管的预测效能及意义[J]. 实用临床医药杂志, 2024, 28(6): 30-36. doi: 10.7619/jcmp.20233382 [7] 康林, 祝莹, 高芸, 等. 血清降钙素、脑钠肽、心肌肌钙蛋白Ⅰ与老年肺炎病情严重程度的关系[J]. 实用临床医药杂志, 2023, 27(17): 93-96. doi: 10.7619/jcmp.20231133 [8] TORRES A, CHALMERS J D, DELA CRUZ C S, et al. Challenges in severe community-acquired pneumonia: a point-of-view review[J]. Intensive Care Med, 2019, 45(2): 159-171. doi: 10.1007/s00134-019-05519-y
[9] 周曙俊, 周军, 王大明. 单核细胞人白细胞抗原DR监测在重症肺炎患者预后评估中的价值[J]. 江苏大学学报: 医学版, 2013, 23(1): 30-33. [10] LIN H S, LEE E, HESTIR K, et al. Discovery of a cytokine and its receptor by functional screening of the extracellular proteome[J]. Science, 2008, 320(5877): 807-811. doi: 10.1126/science.1154370
[11] FREUCHET A, SALAMA A, REMY S, et al. IL-34 and CSF-1, deciphering similarities and differences at steady state and in diseases[J]. J Leukoc Biol, 2021, 110(4): 771-796. doi: 10.1002/JLB.3RU1120-773R
[12] XU B L, LIN X, GONG Y, et al. Interleukin-34: an important modifier in the pathogenesis of influenza pneumonia[J]. Crit Care, 2021, 25(1): 274. doi: 10.1186/s13054-021-03708-0
[13] YU G Z, BING Y T, ZHU S Y, et al. Activation of the interleukin-34 inflammatory pathway in response to influenza A virus infection[J]. Am J Med Sci, 2015, 349(2): 145-150. doi: 10.1097/MAJ.0000000000000373
[14] 肖慧, 徐维国, 范小兵, 等. 血清IL-34、SP-D、CXCL17在甲型流感病毒性肺炎患者中表达及临床意义[J]. 中华肺部疾病杂志(电子版), 2023, 16(3): 349-351. doi: 10.3877/cma.j.issn.1674-6902.2023.03.010 [15] 肖朗, 胡清亮, 冯秀莉, 等. 肺结核合并肺部细菌感染S100A9与IL-34和IFN-γ水平及其诊断价值[J]. 中华医院感染学杂志, 2023, 33(4): 494-497. [16] KHAN F, OWENS M B, RESTREPO M, et al. Tools for outcome prediction in patients with community acquired pneumonia[J]. Expert Rev Clin Pharmacol, 2017, 10(2): 201-211. doi: 10.1080/17512433.2017.1268051
[17] CHRIST-CRAIN M, SCHUETZ P, MVLLER B. Biomarkers in the management of pneumonia[J]. Expert Rev Respir Med, 2008, 2(5): 565-572. doi: 10.1586/17476348.2.5.565
[18] NIEDERMAN M S, TORRES A. Severe community-acquired pneumonia[J]. Eur Respir Rev, 2022, 31(166): 220123. doi: 10.1183/16000617.0123-2022
[19] MARTI C, GARIN N, GROSGURIN O, et al. Prediction of severe community-acquired pneumonia: a systematic review and meta-analysis[J]. Crit Care, 2012, 16(4): R141. doi: 10.1186/cc11447
[20] LANKS C W, MUSANI A I, HSIA D W. Community-acquired pneumonia and hospital-acquired pneumonia[J]. Med Clin North Am, 2019, 103(3): 487-501. doi: 10.1016/j.mcna.2018.12.008




 下载:
下载:

 苏公网安备 32100302010246号
苏公网安备 32100302010246号
