Application value of point-of-care lung ultrasound scoring in selecting respiratory support treatment for neonatal infectious pneumonia
-
摘要:目的
探讨床旁即时肺部超声(POC-LUS)评分在新生儿感染性肺炎(NIP)患儿呼吸支持治疗方式选择中的应用价值。
方法选取89例NIP患儿作为研究对象,根据呼吸困难程度及血气分析结果分为对照组(无辅助通气)46例、无创组(无创辅助通气)28例、有创组(有创机械通气)15例。比较3组患儿的POC-LUS评分,并分析POC-LUS评分与动脉血氧分压[pa(O2)]、动脉血二氧化碳分压[pa(CO2)]的相关性。绘制受试者工作特征(ROC)曲线,评估POC-LUS评分对NIP患儿需要无创辅助通气或有创机械通气治疗的预测效能。
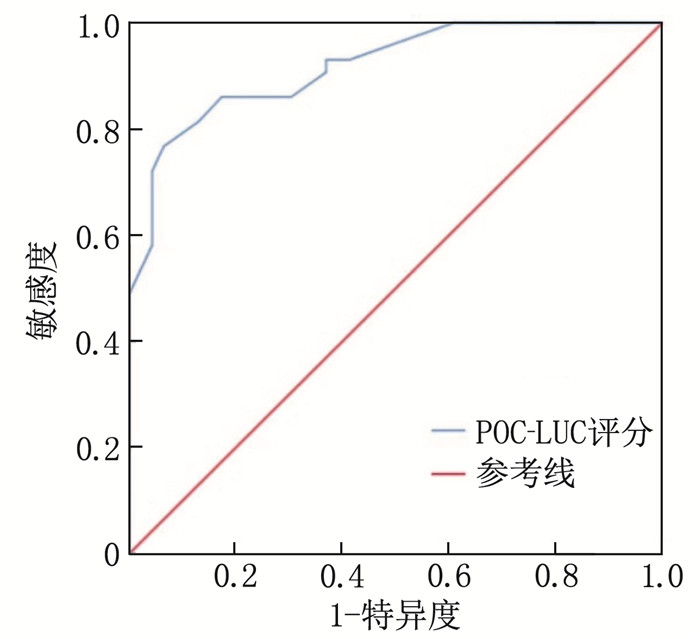
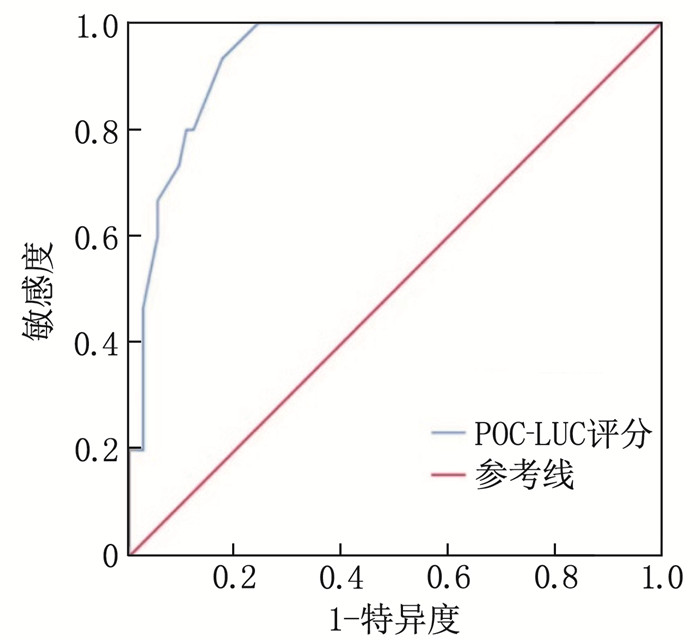
结果无创组、有创组的POC-LUS评分依次为(31.7±7.3)、(42.1±8.0)分,高于对照组的(21.5±7.3)分,且有创组评分高于无创组,差异有统计学意义(P < 0.05)。相关性分析结果显示, POC-LUS评分与pa(O2)呈显著负相关(r=-0.802, P < 0.05), 与pa(CO2)呈显著正相关(r=0.807, P < 0.05)。ROC曲线分析结果显示, POC-LUS评分预测患儿需要无创辅助通气、有创机械通气的曲线下面积(AUC)分别为0.918(95%CI: 0.862~0.973)、0.938(95%CI: 0.889~0.987), 敏感度分别为0.767、0.933, 特异度分别为0.935、0.824, 最佳截断值为29.5、31.5分。
结论POC-LUS评分可量化评估NIP患儿肺部病变严重程度,对临床医师选择辅助通气治疗方式具有指导作用。
Abstract:ObjectiveTo investigate the application value of point-of-care lung ultrasound (POC-LUS) scoring in selecting respiratory support treatment modalities for neonatal infectious pneumonia (NIP).
MethodsA total of 89 NIP patients were selected as the study subjects and divided into control group (no assisted ventilation) with 46 cases, noninvasive group (noninvasive assisted ventilation) with 28 cases, and invasive group (invasive mechanical ventilation) with 15 cases based on the degree of dyspnea and blood gas analysis results. The POC-LUS scores of the three groups were compared, and the correlations of POC-LUS scores with arterial oxygen partial pressure [pa(O2)] and arterial carbon dioxide partial pressure [pa(CO2)] were analyzed. Receiver operating characteristic (ROC) curves were plotted to assess the predictive efficacy of POC-LUS scores for the need for noninvasive assisted ventilation or invasive mechanical ventilation in NIP patients.
ResultsThe POC-LUS scores of the noninvasive group and the invasive group were (31.7±7.3) and (42.1±8.0), respectively, which were higher than (21.5±7.3) of the control group. Additionally, the score of the invasive group was higher than that of the noninvasive group (P < 0.05). Correlation analysis revealed a significant negative correlation between POC-LUS scores and pa(O2) (r=-0.802, P < 0.05), and a significant positive correlation with pa(CO2) (r=0.807, P < 0.05). ROC curve analysis showed that the area under the curve (AUC) of POC-LUS scores for predicting the need for noninvasive assisted ventilation and invasive mechanical ventilation were 0.918 (95%CI, 0.862 to 0.973) and 0.938 (95%CI, 0.889 to 0.987), respectively. The sensitivity was 0.767 and 0.933, and the specificity was 0.935 and 0.824, with optimal cutoff values of 29.5 and 31.5, respectively.
ConclusionPOC-LUS scoring can quantitatively assess the severity of lung lesions in NIP patients and serves as a guiding tool for clinicians in selecting assisted ventilation treatment modalities.
-
-
表 1 3组患儿一般资料比较(x±s)[n(%)]
一般资料 对照组(n=46) 无创组(n=28) 有创组(n=15) 性别 男 29(63.0) 19(67.9) 9(60.0) 女 17(37.0) 9(32.1) 6(40.0) 出生体质量/g 2 316.5±793.9 2 186.7±635.8 2 190.0±754.7 胎龄/d 215.5±18.6 222.6±14.4 217.0±13.0 脉率/(次/min) 138.9±9.7 144.4±9.1* 163.9±11.4*# 呼吸频率/(次/min) 48.7±7.7 53.0±6.9* 71.9±12.3*# pa(O2)/mmHg 78.9±17.7 47.0±5.7* 50.1±19.0* pa(CO2)/mmHg 27.9±13.1 29.5±6.3 59.9±13.3*# pH值 7.37±0.06 7.37±0.06 7.15±0.05*# pa(O2): 动脉血氧分压; pa(CO2): 动脉血二氧化碳分压。与对照组比较, * P < 0.05; 与无创组比较, #P < 0.05。 -
[1] 邵肖梅, 叶鸿瑁, 丘小汕. 实用新生儿学[M]. 5版. 北京: 人民卫生出版社, 2019: 582-588. [2] 赵浩天, 刘奕, 李会英, 等. 床旁即时超声对急重症疑难病患者诊断与评估研究进展[J]. 疑难病杂志, 2021, 20(10): 1072-1076. https://www.cnki.com.cn/Article/CJFDTOTAL-YNBZ202110024.htm [3] ISMAIL R, EL RAGGAL N M, HEGAZY L A, et al. Lung ultrasound role in diagnosis of neonatal respiratory disorders: a prospective cross-sectional study[J]. Children, 2023, 10(1): 173. doi: 10.3390/children10010173
[4] 胡安辉, 简敏, 宗渝敏, 等. 肺部超声评分及血清PCT对新生儿感染性肺炎病情程度的评估价值[J]. 中华医院感染学杂志, 2021, 31(12): 1802-1805. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY202112009.htm [5] 《中华儿科杂志》编辑委员会, 中华医学会儿科学分会新生儿学组. 新生儿机械通气常规[J]. 中华儿科杂志, 2015, 53(5): 327-330. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHEK200405013.htm [6] 江秋霞, 黄嵘森, 沈龙源, 等. 肺部超声新评分法评估新生儿呼吸窘迫综合征机械通气撤机时机的应用价值[J]. 临床超声医学杂志, 2021, 23(4): 280-283. https://www.cnki.com.cn/Article/CJFDTOTAL-LCCY202104011.htm [7] 曹金侠, 朱红权, 张晓荣, 等. 新生儿肺部疾病低剂量多层螺旋CT表现与X射线对比研究[J]. 中国医学装备, 2020, 17(3): 50-53. https://www.cnki.com.cn/Article/CJFDTOTAL-YXZB202003014.htm [8] 万磊, 杨灵杰, 孟庆欣, 等. 超声诊断重症肺炎的临床价值[J]. 东南国防医药, 2022, 24(3): 253-256. https://www.cnki.com.cn/Article/CJFDTOTAL-DNGY202203006.htm [9] 张晓勤, 李春玲, 潘灵爱, 等. 经胸肺部超声彗尾征及血管外肺水指数在脓毒症患者预后评估中的价值[J]. 中华危重病急救医学, 2021, 33(8): 985-989. [10] 郑红雨, 孙振涛, 杨贯宇, 等. 肺超声评价不同吸入氧浓度对儿童肺不张的影响[J]. 中华实用诊断与治疗杂志, 2021, 35(2): 185-188. https://www.cnki.com.cn/Article/CJFDTOTAL-HNZD202102019.htm [11] 廖姮, 牛延德, 朱晓娟, 等. 肺部超声诊断儿童社区获得性肺炎动态的价值研究[J]. 中国临床医学影像杂志, 2022, 33(4): 240-242, 248. https://www.cnki.com.cn/Article/CJFDTOTAL-LYYX202204003.htm [12] 刘立静, 马洪欣, 杜睿, 等. 肺部超声新评分法在新生儿呼吸窘迫综合征病情评价及治疗中的应用效果[J]. 实用临床医药杂志, 2022, 26(21): 111-114. doi: 10.7619/jcmp.20221820 [13] 何海, 廖宏伟, 李莉, 等. 改良肺部超声评分与呼吸窘迫综合征新生儿氧合状态及呼吸支持模式的相关性[J]. 临床超声医学杂志, 2022, 24(12): 953-955. https://www.cnki.com.cn/Article/CJFDTOTAL-LCCY202212017.htm [14] 苏姣, 周海艳, 李传芬. 肺部超声评分和CRP对儿童肺炎病情严重程度的预测意义[J]. 中华肺部疾病杂志: 电子版, 2021, 14(5): 605-607. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFBD202105014.htm [15] 米皎, 伍金林, 章峰敏, 等. 肺部超声在羊水胎粪污染新生儿呼吸支持治疗中的指导价值[J]. 临床和实验医学杂志, 2023, 22(5): 536-539. https://www.cnki.com.cn/Article/CJFDTOTAL-SYLC202305024.htm [16] CHEN J G, HE C, YIN J T, et al. Quantitative analysis and automated lung ultrasound scoring for evaluating COVID-19 pneumonia with neural networks[J]. IEEE Trans Ultrason Ferroelectr Freq Control, 2021, 68(7): 2507-2515. doi: 10.1109/TUFFC.2021.3070696
[17] 肖燕, 闫媛媛, 娄君鸽. 肺超声评分对评估新生儿感染性肺炎病情严重程度的应用价值分析[J]. 中华全科医学, 2020, 18(10): 1711-1714. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY202010028.htm [18] 尹旭, 王倩. 肺部超声与X线在新生儿呼吸窘迫综合征中的诊断价值对比研究[J]. 检验医学与临床, 2018, 15(8): 1077-1079. https://www.cnki.com.cn/Article/CJFDTOTAL-JYYL201808008.htm




 下载:
下载:
 苏公网安备 32100302010246号
苏公网安备 32100302010246号