Percutaneous vertebroplasty versus percutaneous kyphoplasty in treating Kummell disease of peripheral sclerosis type in stage Ⅲ
-
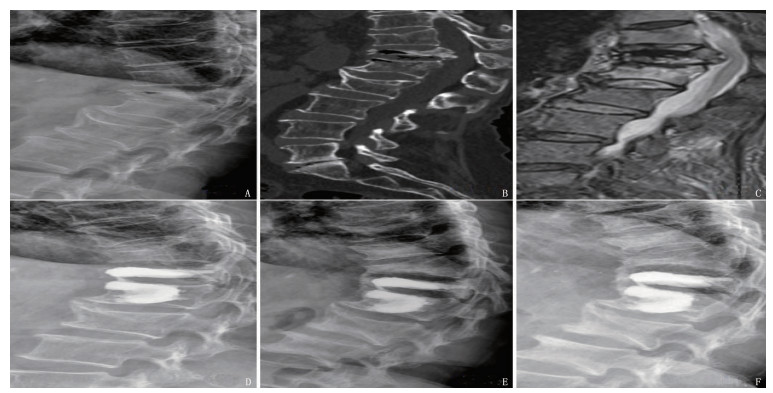
摘要:目的 比较经皮椎体成形术(PVP)与经皮椎体后凸成形术(PKP)治疗周壁硬化型Ⅲ期Kummell病的临床疗效。方法 回顾性分析77例周壁硬化型Ⅲ期Kummell病患者的临床资料,其中11例采用PVP治疗的患者设为PVP组, 66例采用PKP治疗的患者设为PKP组。比较2组手术时间,骨水泥注入量,术前、术后1 d及末次随访时的视觉模拟评分法(VAS)评分、Oswestry功能障碍指数(ODI), 以及椎体前缘高度和病变椎体局部Cobb角。结果 2组均顺利完成手术,且均获得随访, PVP组随访16.00(14.50, 18.00)个月, PKP组随访16.00(14.00, 18.00)个月。PVP组术中骨水泥注入量为3.00(2.00, 3.00) mL, PKP组为4.00(4.00, 5.00) mL, 差异有统计学意义(Z=-4.63, P < 0.01); PVP组手术时间为30.00(27.00, 33.00) min, PKP组为50.00(45.00, 57.00) min, 差异有统计学意义(Z=-4.91, P < 0.01)。术后1 d及末次随访时, 2组患者VAS评分及ODI均较术前降低,差异有统计学意义(P < 0.01)。术后1 d及末次随访时, 2组椎体高度均高于同组术前, Cobb角均低于术前,且PKP组椎体高度大于PVP组, Cobb角小于PVP组,差异均有统计学意义(P < 0.05或P < 0.01)。结论 PVP与PKP均可有效缓解周壁硬化型Ⅲ期Kummell病患者腰背部顽固性疼痛,但PKP可更好地恢复椎体高度,改善局部后凸畸形。Abstract:Objective To compare the clinical efficacy of percutaneous vertebroplasty (PVP) and percutaneous kyphoplasty (PKP) in the treatment of patients with Kummell disease of peripheral sclerosis type in stage Ⅲ.Methods The clinical materials of 77 patients with peripheral sclerosis type of Kummell disease in stage Ⅲ were retrospectively analyzed. Among them, 11 patients treated with PVP were selected as PVP group, and 66 patients treated with PKP were selected as PKP group. The operation time, the injected amount of bone cement, the Visual Analogue Scale (VAS) of pain and Oswestry dysfunction index (ODI) before operation, 1 day after operation and at the last follow-up, the height of the anterior edge of the vertebral body and the local Cobb angle of the diseased vertebral body were compared between the two groups.Results Patients in both groups completed the operation successfully and were followed up. The PVP group was followed up for 16.00 (14.50, 18.00) months, and the PKP group was followed up for 16.00 (14.00, 18.00) months. The intraoperative injected volume of bone cement was 3.00 (2.00, 3.00) mL in the PVP group and 4.00 (4.00, 5.00) mL in the PKP group, and there was a significant difference between two groups (Z=-4.63, P < 0.01); the operation time was 30.00 (27.00, 33.00) min in the PVP group and 50.00 (45.00, 57.00) min in the PKP group, and there was also a significant difference between two groups (Z=-4.91, P < 0.01). One day after operation and at the last follow-up, the VAS score and ODI in both groups were significantly lower than those before operation in the same group (P < 0.01). One day after operation and at the last follow-up, the vertebral body height in both groups were higher than that before operation in the same group, and the Cobb angle was significantly lower than that before operation; meanwhile, the vertebral body height of the PKP group was higher than that of the PVP group, and the Cobb angle was smaller than that of the PVP group; the differences above were statistically significant (P < 0.05 or P < 0.01).Conclusion Both PVP and PKP can effectively alleviate the intractable pain in the lower back of patients with peripheral sclerosis type of Kummell disease in stage Ⅲ, but PKP can better restore the height of vertebral body and improve local kyphosis.
-
血流感染是临床重症感染性疾病之一,具有较高的发病率和致死率,尽早检出致病菌同时精准用药可有效降低病死率[1-3]。血培养为诊断血流感染的金标准,但培养及检测时间长,且需得到纯培养菌落后才能进行鉴定及抗生素敏感试验。基质辅助激光解析电离飞行时间质谱(MALDI-TOF MS)已被报道[4]用于直接鉴定血培养标本中的病原菌,其为临床微生物检验提供了一种省时、有效的手段,因而备受微生物人员关注。本研究采用MALDI-TOF MS的检测体系对血流感染的病原菌进行检测和鉴定,为临床快速诊断及指导用药提供有力依据,现报告如下。
1. 资料与方法
1.1 一般资料
共纳入2017年4月—2019年4月西京医院检验科321例血流感染患者,收集血液标本并将其放入培养瓶中进行血培养,微生物室细菌培养结果均为阳性(其中需氧瓶181瓶,厌氧瓶100瓶,儿童瓶40瓶)。排除直接涂片革兰染色未见细菌和2种以上细菌的血液标本。
1.2 仪器与试剂
BACTEC FX400全自动血培养系统及其配套的需氧瓶、厌氧瓶、儿童瓶及分离胶促凝管均购自美国BD公司; 血琼脂平板和巧克力平板购自安图公司; 甲酸、乙腈、VITEK MS质谱仪、基质液、靶板、VITEK 2 COMPACT、GN卡、GP卡、ANC卡均购自法国梅里埃公司。质控菌株大肠埃希菌ATCC8739由本院微生物室保存。
1.3 方法
① 涂片染色镜检: 血培养瓶报警后,抽取培养物进行涂片镜检及转种,通过革兰染色镜检初步判定待检菌的种类,并排除样本假阳性干扰并做好镜检记录。
② 菌种常规鉴定: 从血培养系统中取出报警为阳性的血培养瓶,混匀后抽取阳性瓶中液体,分别涂布于血琼脂平板和巧克力平板,镜检结果若为真菌加转沙保弱平板,放置需氧或厌氧环境中培养菌种18~24 h。长出菌落后在平板上挑取单个纯菌落,用棉拭子配制0.5麦氏单位菌悬液,根据病原菌的生长特征和染色性,选择合适的板卡通过VITEK 2 COMPACT进行病原菌鉴定。
③ 分离胶促凝管样本预处理: 先混匀报警阳性的血培养瓶,用无菌注射器抽取2.5 mL血培养瓶中的液体转移至含有促凝剂的真空采血管内,室温下4 000 g离心10 min。离心后小心弃去上清液,分离胶边缘可见灰白色菌膜沉淀,用1 mL悬液转移至1.5 mL eppendof管中,加入200 μL 10%的SDS, 漩涡震荡1 min, 室温放置5 min后13 000转/min离心2 min, 小心弃上清液,沉淀中加入75%乙醇700 μL, 吹吸混匀,室温放置10 min, 13 000转/min离心2 min, 弃去上清液, 13 000转/min离心1 min, 小心弃去所有上清液。剩余沉淀在生物安全柜中室温放置5 min, 待乙醇完全挥发。
④ MALDI-TOF MS鉴定: 沉淀中加15 μL浓度为70%的甲酸,吹吸混匀,室温放置5~10 min, 加等量乙腈(15 μL), 吹吸混匀, 13 000转/min离心2 min。取1 μL的上清液滴于靶板,室温晾干。加基质,进样至MALDI-TOF MS系统中分析并记录结果。
⑤ 传统微生物培养鉴定结果: 采用VITEK 2 COMPACT对所有分离菌群鉴定种类,若菌种鉴定准确率为95%以上表示鉴定结果可靠。本实验以VITEK 2 COMPACT常规鉴定结果为标准,将MALDI-TOF MS直接鉴定的结果与其进行比较(MALDI-TOF MS鉴定结果准确率均为90%以上)。
2. 结果
180株革兰阴性菌临床分离株中, MALDI-TOF MS鉴定准确率为97.78%, 无鉴定错误出现。1例大肠埃希菌, 1例肺炎克雷伯菌, 1例阴沟肠杆菌, 1例嗜麦芽窄食单胞菌均未鉴定出。
141株革兰阳性菌临床分离株中, MALDI-TOF MS鉴定准确率为84.39%。1例金黄色葡萄球菌, 1例表皮葡萄球菌, 1例屎肠球菌, 2例粪肠球菌, 1例溶血葡萄球菌及1例蜡样芽孢杆菌存在鉴定错误,其中蜡样芽孢杆菌误鉴定为大肠埃希菌, 11.35%革兰阳性菌株未鉴定出结果。见表 1。
表 1 321株临床分离株MALDI-TOF MS鉴定结果[n(%)]菌属 菌名 VITEK2 COMPAC方法 MALDI-TOF MS方法 鉴定株数/株 鉴定准确 鉴定错误/株 未鉴定出 革兰阴性菌(n=180) 大肠埃希菌 30 29(96.67) 0 1(3.33) 肺炎克雷伯菌 30 29(96.67) 0 1(3.33) 铜绿假单胞菌 20 20(100.00) 0 0 鲍曼不动杆菌 20 20(100.00) 0 0 阴沟肠杆菌 20 19(95.00) 0 1(5.00) 黏质沙雷菌 20 20(100.00) 0 0 产气肠杆菌 20 20(100.00) 0 0 嗜麦芽窄食单菌 20 19(95.00) 0 1(5.00) 革兰阳性菌(n=141) 金黄色葡萄球菌 30 27(90.00) 1(3.33) 3(10.00) 表皮葡萄球菌 30 25(83.33) 1(3.33) 4(13.33) 屎肠球菌 20 17(85.00) 1(5.00) 2(10.00) 粪肠球菌 20 16(80.00) 2(10.00) 2(10.00) 肺炎链球菌 20 19(95.00) 0 1(5.00) 溶血葡萄球菌 20 15(75.00) 1(5.00) 4(20.00) 蜡样芽孢杆菌 1 0 1(100.00) 0 3. 讨论
早期准确的病原学诊断是血流感染诊治的关建,传统的病原微生物主要依靠其形态学特征、生化反应及血清学反应进行鉴定,但这些鉴定方法一般需要72 h左右才能完成,容易使危重患者错过最佳治疗时机。应用分子生物学检测病原菌结果准确,但价格昂贵,不适合作为大批量标本的常规鉴定方法。MALDI-TOF MS技术是一种新型电离技术,能够快速、准确地鉴定培养得到的纯菌落,具有菌种涵盖范围广、准确度高、成本低、实用性强、鉴定速度快、安全性高、易于操作等优点,常规细菌鉴定24 h内即可得出鉴定结果[5-6]。采用MALDI-TOF MS对部分疑难或慢生长致病菌进行鉴定能够显著缩短鉴定时间[7]。分离胶促凝管联合MALDI-TOF MS方法可提高鉴定效率,但是也存在部分结果不符现象,如本研究将蜡样芽孢杆菌误鉴定为大肠埃希菌,说明在实际工作中不能将此方法彻底代替常规转种培养方法,采用2种方法配合使用,取长补短,不仅使MALDI-TOF MS检验快速准确,还能保留传统方法准确率较高的优势[8-10]。因此,采用MALDI-TOF MS方法对血培养细菌快速鉴定的同时进行直接药物敏感性实验,可尽快得出鉴定和药物敏感性结果,有助于缩短患者平均住院时间,降低病死率,减少住院费用[11-12]。
综上所述, MALDI-TOF MS方法直接检测血培养阳性待检菌具有快速、准确、方便、低成本的优势,能够为血流感染患者争取宝贵时间,满足临床早期诊断与干预需求。
-
表 1 2组手术前后VAS评分及ODI比较[P50(P25, P75)]
组别 n VAS评分/分 ODI/% 术前 术后1 d 末次随访 术前 术后1 d 末次随访 PVP组 11 7.00(7.00, 8.00) 2.00(2.00, 3.00)** 2.00(2.00, 3.00)** 74.00(72.00, 76.00) 24.00(22.00, 26.00)** 24.00(22.00, 24.00)** PKP组 66 7.00(7.00, 8.00) 3.00(2.00, 3.00)** 2.00(2.00, 3.00)** 74.00(72.00, 78.00) 24.00(24.00, 26.00)** 24.00(22.00, 24.00)** VAS: 视觉模拟评分法; ODI: Oswestry功能障碍指数。与术前比较, **P < 0.01。 表 2 2组手术前后椎体高度及Cobb角比较[P50(P25, P75)]
组别 n 椎体高度/cm Cobb角/° 术前 术后1 d 末次随访 术前 术后1 d 末次随访 PVP组 11 0.68(0.56, 0.74) 0.88(0.74, 0.99)** 0.83(0.71, 0.92)** 23.96(16.56, 28.31) 20.08(11.89, 24.43)** 21.22(12.75, 25.64)** PKP组 66 0.71(0.60, 0.83) 1.22(1.10, 1.39)**## 1.18(1.02, 1.32)**## 23.86(21.63, 28.58) 13.34(10.86, 14.66)**# 14.84(12.36, 17.46)**# 与术前比较, **P < 0.01; 与PVP组比较, #P < 0.05, ##P < 0.01。 -
[1] 陈昊, 杨惠林. 骨质疏松性椎体压缩骨折诊治的思考[J]. 中华创伤骨科杂志, 2019, 21(4): 366-368. doi: 10.3760/cma.j.issn.1671-7600.2019.04.017 [2] LIM J, CHOI S W, YOUM J Y, et al. Posttraumatic delayed vertebral collapse: kummell's disease[J]. J Korean Neurosurg Soc, 2018, 61(1): 1-9. doi: 10.3340/jkns.2017.0505.010
[3] KIM J E, CHOI S S, LEE M K, et al. Failed percutaneous vertebroplasty due to insufficient correction of intravertebral instability in kummell's disease: a case report[J]. Pain Pract, 2017, 17(8): 1109-1114. doi: 10.1111/papr.12561
[4] YUDOYONO F, RUSPANAH I, BARAQBAH H. Three-level thoracolumbar vertebroplasty with screw-rod-wire construct in Kummels disease patient with neurological deficit after low impact injury[J]. Nsmc, 2020, 3(3): 118-121. doi: 10.36444/nsmc.v3i3.124
[5] LI K C, LI A F Y, HSIEH C H, et al. Another option to treat Kümmell's disease with cord compression[J]. Eur Spine J, 2007, 16(9): 1479-1487. doi: 10.1007/s00586-006-0094-z
[6] KIM H S, LEE S K, KIM S W, et al. Chronic Spinal Epidural Hematoma Related to Kummell's Disease[J]. J Korean Neurosurg Soc, 2011, 49(4): 231-233. doi: 10.3340/jkns.2011.49.4.231
[7] HUANG Y J, PENG M X, HE S Q, et al. Clinical efficacy of percutaneous kyphoplasty at the hyperextension position for the treatment of osteoporotic kümmell disease[J]. Clin Spine Surg A Spine Publ, 2016, 29(4): 161-166. doi: 10.1097/BSD.0000000000000259
[8] HUANG Y S, HAO D J, WANG X D, et al. Long-segment or bone cement-augmented short-segment fixation for kummell disease with neurologic deficits A comparative cohort study[J]. World Neurosurg, 2018, 116: e1079-e1086. doi: 10.1016/j.wneu.2018.05.171
[9] 李伟, 楼宇梁, 全仁夫. 脊柱后路PSO截骨长节段固定治疗Kummells病伴脊柱后凸的临床疗效[J]. 中华老年骨科与康复电子杂志, 2019, 5(1): 33-38. doi: 10.3877/cma.j.issn.2096-0263.2019.01.007 [10] PARK J W, PARK J H, JEON H J, et al. Kümmell's disease treated with percutaneous vertebroplasty: minimum 1 year follow-up[J]. Korean J Neurotrauma, 2017, 13(2): 119-123. doi: 10.13004/kjnt.2017.13.2.119
[11] 唐永超, 莫国业, 张顺聪, 等. 经皮椎体强化术治疗无神经症状Kümmell病的中长期疗效[J]. 中国脊柱脊髓杂志, 2018, 28(1): 38-43. doi: 10.3969/j.issn.1004-406X.2018.01.06 [12] 刘义杰, 杨森, 李雪峰, 等. 经皮椎体后凸成形术治疗无神经症状性Ⅲ期Kümmell病[J]. 中华创伤骨科杂志, 2019, 21(10): 888-893. doi: 10.3760/cma.j.issn.1671-7600.2019.10.012 [13] CHEN L, DONG R B, GU Y, et al. Comparison between balloon kyphoplasty and short segmental fixation combined with vertebroplasty in the treatment of kümmell's disease[J]. Pain Physician, 2015, 18(4): 373-381.
[14] JACOBSON R E, PALEA O, GRANVILLE M. Progression of vertebral compression fractures after previous vertebral augmentation: technical reasons for recurrent fractures in a previously treated vertebra[J]. Cureus, 2017, 9(10): e1776. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5732011/
[15] YANG H L, LIU H, WANG S H, et al. Review of percutaneous kyphoplasty in China[J]. Spine (Phila Pa 1976), 2016, 41(Suppl 19): B52-B58. http://www.ncbi.nlm.nih.gov/pubmed/27656784
[16] WANG B, WANG Y H, ZHANG H P, et al. A novel bone cement screw system combined with vertebroplasty for the treatment of Kummell disease with bone deficiency at the vertebral anterior border: a minimum 3-year follow-up study[J]. Clin Neurol Neurosurg, 2021, 201: 106434.
-
期刊类型引用(7)
1. 刘业琼,王蕾,曹励欧,徐炜新. 中段尿样本病原菌快速检测方法的建立与评估. 分子诊断与治疗杂志. 2025(03): 441-444 .  百度学术
百度学术
2. 袁佳春,许明佳,许艳丹,李伟,叶玉龙. 上海金山区宾馆淋浴水和公共浴室水中嗜肺军团菌MALDI-TOF MS快速检测及聚类分析. 中国卫生检验杂志. 2023(04): 426-428 .  百度学术
百度学术
3. 张小云,刘本,连建春,姜玉章,唐朝贵,王霞. 质谱鉴定联合直接快速药敏试验在细菌血流感染中的应用. 医学信息. 2023(03): 98-103 .  百度学术
百度学术
4. 蒲玉熙,次仁央金,嘎松卓嘎,赵颖,刘治娟. 高原地区两种微生物鉴定系统对临床常见病原菌鉴定的一致性分析. 中国实用医药. 2023(07): 97-99 .  百度学术
百度学术
5. 吴奇福. ALDI-TOF MS技术在微生物检验中的应用效果及效能ROC曲线. 中国医药指南. 2023(16): 121-124 .  百度学术
百度学术
6. 任燕飞,张敏,杨涛,李荣凯,梁新. 下呼吸道感染病原体检测方法及相关病原体研究. 中国现代医生. 2022(25): 114-117 .  百度学术
百度学术
7. 张鞠玲,康琳,鲍春梅,王欢,贾天野,陈素明,庞君丽,李伯安. MALDI-TOF MS技术直接鉴定无菌体液病原菌的效果评价. 国际检验医学杂志. 2022(24): 3016-3021 .  百度学术
百度学术
其他类型引用(1)




 下载:
下载:
 苏公网安备 32100302010246号
苏公网安备 32100302010246号