Effect of multidisciplinary collaboration model in patients with systemic lupus erythematosus during pregnancy
-
摘要:目的
观察多学科协作模式在妊娠期系统性红斑狼疮(SLE)患者中的应用效果。
方法采用随机数字表法将60例妊娠期SLE患者分为常规护理组和强化护理组,每组30例。常规护理组采用常规护理,强化护理组采用多学科协作模式强化护理,观察并比较2组患者心理状态[焦虑自评量表(SAS)、抑郁自评量表(SDS)评分]、分娩成功率和SLE复发情况。
结果护理后, 2组患者SAS评分、SDS评分均低于护理前,且强化护理组SAS评分、SDS评分低于常规护理组,差异有统计学意义(P < 0.05)。2组均未出现SLE复发患者,但各有1例患者流产,其余患者均正常分娩。
结论将多学科协作模式应用于妊娠期SLE患者中,能够显著减轻患者抑郁、焦虑状态。
Abstract:ObjectiveTo observe the application effect of multidisciplinary collaboration model in patients with systemic lupus erythematosus(SLE) during pregnancy.
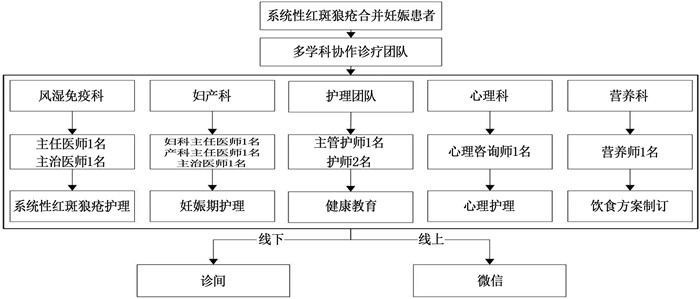
MethodsSixty patients with SLE in pregnancy were divided into routine nursing group(n=30) and intensive nursing group(n=30) by random number table method. Patients in the routine nursing group were treated with routine nursing, and patients in the intensive nursing group were treated with intensive nursing based on multidisciplinary collaboration model. The psychological status[Self-rating Anxiety Scale (SAS), self-rating Depression Scale (SDS) scores], delivery success rate and recurrence condition of SLE were observed and compared between the two groups.
ResultsAfter nursing, SAS score and SDS score of two groups were lower than before nursing, and SAS score and SDS score of intensive nursing group were lower than the routine nursing group, the differences were statistically significant (P < 0.05). There were no SLE recurrence patients in the two groups, but one patient in each group had abortion, and the other patients delivered normally.
ConclusionMultidisciplinary collaboration model can significantly reduce depression and anxiety in SLE patients during pregnancy.
-
Keywords:
- systemic lupus erythematosus /
- pregnancy /
- multidisciplinary collaboration model /
- Wechat /
- anxiety /
- depression
-
-
表 1 2组患者焦虑、抑郁水平比较[M(P25, P75)]
分 组别 n SAS评分 SDS评分 护理前 护理后 护理前 护理后 常规护理组 30 65.6(62.2, 67.5) 63.1(57.5, 65.3)* 62.5(57.2, 65.0) 60.0(54.7, 61.6)* 强化护理组 30 62.5(60.0, 67.5) 55.0(51.3, 58.1)*# 62.5(60.0, 67.5) 50.0(44.7, 52.5)*# SAS: 焦虑评分量表; SDS: 抑郁自评量表。与护理前比较, *P < 0.05; 与常规护理组比较, #P < 0.05。 表 2 2组患者实验室指标比较[M(P25, P75)]
指标 常规护理组(n=30) 强化护理组(n=30) 护理前 护理后 护理前 护理后 抗双链DNA抗体/(IU/mL) 29.5(23.5, 35.0) 23.0(15.0, 37.8) 24.5(16.0, 37.0) 21.5(13.0, 41.0) 补体C3/(g/L) 1.3(0.8, 2.0) 1.2(0.8, 1.8) 1.6(1.0, 2.5) 1.5(0.8, 3.1) 24 h尿蛋白/mg 52.0(23.8, 95.0) 43.0(24.8, 74.3) 36.0(24.5, 69.8) 29.0(20.8, 53.3) -
[1] HUSAKOVA M. microRNAs in the key events of systemic lupus erythematosuspathogenesis[J]. Biomed Pap Med FacUnivPalacky Olomouc Czech Repub, 2016, 160(3): 327-342. doi: 10.5507/bp.2016.004
[2] 张琪琪, 张贝, 武新峰, 等. 系统性红斑狼疮不良妊娠结局相关因素[J]. 中华临床免疫和变态反应杂志, 2022, 16(1): 24-29. https://www.cnki.com.cn/Article/CJFDTOTAL-OZHL202201005.htm [3] 张艳红, 赵国光, 李小莹, 等. 多学科协作在高龄骨科患者围术期全程管理中的应用[J]. 中国病案, 2020, 21(12): 44-46. doi: 10.3969/j.issn.1672-2566.2020.12.017 [4] DE JESUS G R, MENDOZA-PINTO C, DE JESUS N R, et al. Understanding and managing pregnancy in patients with lupus[J]. Autoimmune Dis, 2015, 2015: 943490.
[5] 徐丽玲, 郭乾育, 蔡小燕, 等. 糖皮质激素治疗系统性红斑狼疮患者的现况调查[J]. 中华内科杂志, 2017, 56(4): 290-294. doi: 10.3760/cma.j.issn.0578-1426.2017.04.010 [6] 张翠琴. 基于互联网的健康教育对妊娠糖尿病孕妇的自护能力及妊娠结局的影响[J]. 糖尿病新世界, 2021, 24(12): 162-165. https://www.cnki.com.cn/Article/CJFDTOTAL-TNBX202112040.htm [7] HOCHBERG M C. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus[J]. Arthritis Rheum, 1997, 40(9): 1725.
[8] 杨艳, 刘恩令, 李君, 等. 系统性红斑狼疮妊娠时机对妊娠结局影响的Meta分析[J]. 现代妇产科进展, 2017, 26(11): 851-854. https://www.cnki.com.cn/Article/CJFDTOTAL-XDFC201711013.htm [9] 黎静, 罗漫灵, 钟梅. 妊娠合并系统性红斑狼疮的围孕期管理[J]. 中国实用妇科与产科杂志, 2016, 32(10): 934-939. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGSF201610005.htm [10] 林华娟. 高危妊娠的筛查和管理及其与不良妊娠结局的关系分析[J]. 中国全科医学, 2021, 24(S1): 86-87. https://www.cnki.com.cn/Article/CJFDTOTAL-QKYX2021S1032.htm [11] 陈如梦, 傅荣, 徐任菊. 糖皮质激素维持治疗患者自我感受的质性研究[J]. 中华护理杂志, 2019, 54(9): 1364-1369. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHHL201909020.htm [12] ZUCCHI D, TANI C, MONACCI F, et al. Pregnancy and undifferentiated connective tissue disease: outcome and risk of flare in 100 pregnancies[J]. Rheumatology (Oxford), 2020, 59(6): 1335-1339.
[13] 刘菊梅, 罗健英. 妊娠合并系统性红斑狼疮不良妊娠结局预测因素的研究[J]. 中国妇幼保健, 2019, 34(20): 4837-4839. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB201920079.htm [14] 孙振晓, 刘化学, 焦林瑛, 等. 医院焦虑抑郁量表的信度及效度研究[J]. 中华临床医师杂志: 电子版, 2017, 11(2): 198-201. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLYD201702005.htm [15] 杨夏, 李焕平. 白芍总苷治疗系统性红斑狼疮患者的临床疗效及对免疫功能的影响[J]. 世界中医药, 2019, 14(5): 1270-1273. https://www.cnki.com.cn/Article/CJFDTOTAL-SJZA201905048.htm [16] 陈群, 严远飞, 陈数, 等. 系统性红斑狼疮合并心脏损害的相关危险因素分析[J]. 实用临床医药杂志, 2022, 26(1): 109-115. doi: 10.7619/jcmp.20212670 [17] CHEN Y J, CHANG J C, LAI E L, et al. Maternal and perinatal outcomes of pregnancies in systemic lupus erythematosus: a nationwide population-based study[J]. Semin Arthritis Rheum, 2020, 50(3): 451-457.
[18] 狄文, 吴珈悦. 妊娠合并自身免疫性疾病的孕期健康管理[J]. 实用妇产科杂志, 2021, 37(8): 561-563. https://www.cnki.com.cn/Article/CJFDTOTAL-SFCZ202108001.htm [19] 郑均燕. 系统性红斑狼疮合并妊娠患者妊娠结局的影响因素研究[J]. 临床护理杂志, 2020, 19(5): 48-50. https://www.cnki.com.cn/Article/CJFDTOTAL-LCHL202005017.htm [20] DONG Y H, WANG P, DAI Z P, et al. Increased self-care activities and glycemic control rate in relation to health education via Wechat among diabetes patients: a randomized clinical trial[J]. Medicine, 2018, 97(50): e13632.




 下载:
下载:
 苏公网安备 32100302010246号
苏公网安备 32100302010246号

