Correlation between left atrial diameter and renal function in patients with atrial fibrillation
-
摘要:目的
探讨心房颤动患者左心房内径(LAD)与肾功能的相关性。
方法选取364例心房颤动患者作为研究对象, 收集患者的临床资料, 包括性别、年龄、身高、体质量、吸烟史、饮酒史、心房颤动类型、高血压病史、冠心病病史、糖尿病病史、心力衰竭病史、用药史、高敏肌钙蛋白I、脑钠肽、C反应蛋白、肌酐、尿素氮、LAD、左室射血分数(LVEF)、左室舒张末期内径(LVDd)、左室后壁厚度(LVPWTd)和室间隔厚度(IVSTd); 计算估算肾小球滤过率(eGFR)和体质量指数。采用Spearman相关分析法探讨LAD与肌酐、尿素氮、eGFR的相关性; 将eGFR < 60 mL/(min·1.73 m2)设定为肾功能不全, 采用单因素Logistic回归分析探讨心房颤动患者肾功能不全的影响因素; 采用二元Logistic回归分析探讨房颤患者LAD与肾功能不全的关系。
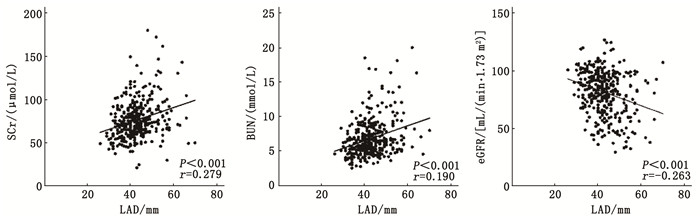
结果Spearman相关分析结果显示, 心房颤动患者中LAD与肌酐(r=0.279, P < 0.001)、尿素氮(r=0.190, P < 0.001)呈正相关, 与eGFR(r=-0.263, P < 0.001)呈负相关。单因素Logistic回归分析结果显示, 性别、糖尿病病史、高血压病史、冠心病病史、心力衰竭病史、房颤类型、钠-葡萄糖共转运蛋白2抑制剂用药史、利尿剂用药史、LAD、LVEF、LVDd、IVSTd均为房颤患者肾功能不全的影响因素(P < 0.05)。二元Logistic回归分析结果显示, 与LAD第1四分位(LAD ≤ 38 mm)相比, LAD第4四分位(LAD>47 mm)心房颤动患者发生肾功能不全的风险升高5.199倍(OR=5.199, 95 %CI: 1.210~22.337, P=0.027)。
结论心房颤动患者的LAD与肾功能显著相关, 且LAD是心房颤动患者肾功能不全的影响因素。
Abstract:ObjectiveTo explore the correlation between left atrial diameter (LAD) and renal function in patients with atrial fibrillation.
MethodsA total of 364 patients with atrial fibrillation were selected as study subjects. Clinical data of the patients were collected, including gender, age, height, body weight, smoking history, drinking history, atrial fibrillation type, history of hypertension, coronary heart disease, diabetes, heart failure, medication history, high-sensitivity troponin I, brain natriuretic peptide, C-reactive protein, creatinine, urea nitrogen, LAD, left ventricular ejection fraction (LVEF), left ventricular end-diastolic diameter (LVDd), left ventricular posterior wall thickness (LVPWTd), and interventricular septal thickness (IVSTd). Estimated glomerular filtration rate (eGFR) and body mass index were calculated. Spearman correlation analysis was used to explore the correlations of LAD with creatinine, urea nitrogen, and eGFR. With eGFR < 60 mL/(min·1.73 m2) setting as renal insufficiency, univariate Logistic regression analysis was used to explore the influencing factors of renal insufficiency in patients with atrial fibrillation. Binary Logistic regression analysis was used to explore the relationship between LAD and renal insufficiency in patients with atrial fibrillation.
ResultsSpearman correlation analysis showed that LAD was positively correlated with creatinine (r=0.279, P < 0.001) and urea nitrogen (r=0.190, P < 0.001) in patients with atrial fibrillation, and negatively correlated with eGFR (r=-0.263, P < 0.001). Univariate Logistic regression analysis showed that gender, history of diabetes, hypertension, coronary heart disease, heart failure, atrial fibrillation type, sodium-glucose cotransporter 2 inhibitor medication history, diuretic medication history, LAD, LVEF, LVDd, and IVSTd were all influencing factors of renal insufficiency in patients with atrial fibrillation (P < 0.05). Binary Logistic regression analysis showed that compared with the first quartile of LAD (LAD ≤ 38 mm), the risk of renal insufficiency in patients with atrial fibrillation in the fourth quartile of LAD (LAD>47 mm) increased by 5.199 times(OR=5.199; 95 %CI, 1.210 to 22.337; P=0.027).
ConclusionLAD of patients with atrial fibrillation is significantly related to renal function, and LAD is an influencing factor of renal insufficiency in patients with atrial fibrillation.
-
-
表 1 4组房颤患者一般资料比较[n(%)][M(P25, P75)]
指标 分类 第1组(n=95) 第2组(n=99) 第3组(n=90) 第4组(n=80) χ2/H P 性别 男 42(44.21) 56(56.57) 55(61.11) 50(62.50) 7.681 0.053 女 53(55.79) 43(43.43) 35(38.89) 30(37.50) 年龄/岁 68.00(58.00, 77.00) 69.00(61.00, 77.00) 70.00(61.75, 77.25) 73.50(63.00, 81.00) 5.837 0.120 体质量指数/(kg/m2) 24.98(23.03, 26.67) 26.37(24.61, 28.55) 27.11(24.27, 28.75) 26.75(24.73, 29.90) 18.124 < 0.001 吸烟史 14(14.74) 25(25.25) 23(25.56) 20(25.00) 4.478 0.214 饮酒史 10(10.53) 20(20.20) 21(23.33) 14(17.50) 5.699 0.127 病史 糖尿病 17(17.89) 28(28.28) 30(33.33) 27(33.75) 7.394 0.060 高血压 48(50.53) 56(56.57) 58(64.44) 52(65.00) 5.341 0.148 冠心病 35(36.84) 46(46.46) 45(50.00) 43(53.75) 5.696 0.127 心力衰竭 6(6.32) 14(14.14) 18(20.00) 22(27.50) 15.390 0.002 用药史 胰岛素 5(5.26) 3(3.03) 5(5.56) 6(7.50) 1.821 0.610 SGLT2i 5(5.26) 4(4.04) 7(7.78) 4(5.00) 1.354 0.716 β受体阻滞剂 22(23.16) 23(23.23) 26(28.89) 25(31.25) 2.828 0.516 钙通道阻滞剂 21(22.11) 21(21.21) 28(31.11) 19(23.75) 3.028 0.387 ACEI/ARB/ARNI 32(33.68) 26(26.26) 30(33.33) 30(37.50) 2.759 0.430 利尿剂 9(9.47) 11(11.11) 9(10.00) 18(22.50) 8.503 0.037 房颤类型 持续性 16(16.84) 49(49.49) 51(56.67) 63(78.75) 69.759 < 0.001 阵发性 79(83.16) 50(50.51) 39(43.33) 17(21.25) hs-cTnI/(ng/mL) 0.001(0.001, 0.006) 0.003(0.001, 0.190) 0.008(0.001, 0.029) 0.010(0.001, 0.035) 23.481 < 0.001 脑钠肽/(ng/mL) 70.39(26.10, 155.97) 201.30(81.48, 396.30) 248.78(112.00, 571.78) 423.98(179.94, 1 118.80) 62.210 < 0.001 C反应蛋白/(mg/L) 0.50(0.50, 1.29) 0.95(0.50, 2.98) 0.63(0.50, 3.15) 1.17(0.50, 4.63) 9.440 0.024 eGFR/[mL/(min·1.73 m2)] 89.90(76.68, 98.84) 86.33(73.65, 7.31) 81.97(69.51, 93.46) 75.26(56.24, 92.61) 21.651 < 0.001 SCr/(μmol/L) 68.02(55.17, 78.44) 72.80(60.91, 85.53) 74.45(65.31, 86.98) 80.35(70.34, 99.75) 29.490 < 0.001 BUN/(mmol/L) 5.83(4.59, 7.11) 6.59(5.07, 7.88) 6.31(5.02, 7.65) 6.95(5.46, 8.91) 13.747 0.003 LVEF/% 60.00(58.00, 60.00) 58.00(55.00, 60.00) 58.00(55.00, 60.00) 55.50(43.50, 58.00) 83.370 < 0.001 LVDd/mm 45.00(43.00, 48.00) 47.00(44.00, 50.00) 48.00(46.00, 53.00) 50.00(48.00, 57.75) 72.768 < 0.001 左室后壁厚度/mm 8.60(8.00, 9.20) 9.00(8.50, 9.60) 9.30(8.70, 10.00) 9.75(9.00, 10.30) 39.431 < 0.001 室间隔厚度/mm 9.00(8.10, 10.00) 9.30(8.80, 10.00) 9.95(9.00, 11.00) 10.00(9.00, 11.00) 25.637 < 0.001 SGLT2i: 钠-葡萄糖协同转运蛋白2抑制剂; ACEI: 血管紧张素转化酶抑制剂; ARB: 血管紧张素Ⅱ受体阻断剂; ARNI: 血管紧张素受体-脑啡肽酶抑制剂; hs-cTnI: 高敏肌钙蛋白I; eGFR: 估算肾小球滤过率; SCr: 肌酐; BUN: 尿素氮; LVEF: 左室射血分数; LVDd: 左室舒张末期内径。 表 2 房颤患者肾功能不全的单因素Logistic回归分析
变量 β SE OR 95%CI P 性别 -0.645 0.288 0.525 0.298~0.922 0.025 体质量指数 -0.061 0.041 0.941 0.869~1.019 0.135 吸烟史 -0.559 0.386 0.572 0.268~1.219 0.148 饮酒史 -0.751 0.454 0.472 0.194~1.150 0.099 高敏肌钙蛋白I -0.558 0.788 0.572 0.122~2.680 0.479 C反应蛋白 -0.001 0.002 0.999 0.995~1.004 0.761 房颤类型 0.658 0.293 1.931 1.088~3.426 0.025 糖尿病病史 1.037 0.293 2.820 1.588~5.006 < 0.001 高血压病史 0.846 0.320 2.329 1.243~4.365 0.008 冠心病病史 0.965 0.298 2.625 1.463~4.711 0.001 心力衰竭病史 0.678 0.340 1.970 1.012~3.834 0.046 SGLT2i用药史 1.343 0.481 3.830 1.492~9.832 0.005 ACEI/ARB/ARNI用药史 0.345 0.294 1.412 0.793~2.514 0.241 β受体阻滞剂用药史 0.435 0.305 1.545 0.850~2.811 0.154 利尿剂用药史 0.812 0.363 2.253 1.106~4.588 0.025 左心房内径 0.090 0.019 1.094 1.053~1.136 < 0.001 左室射血分数 -0.042 0.013 0.959 0.934~0.984 0.002 左室舒张末期内径 0.043 0.021 1.044 1.001~1.088 0.042 左室后壁厚度 0.211 0.136 1.234 0.946~1.611 0.121 室间隔厚度 0.202 0.091 1.224 1.024~1.463 0.027 表 3 房颤患者LAD与肾功能不全的二元Logistic回归分析
LAD分组 模型1 模型2 模型3 β SE OR(95%CI) P β SE OR(95%CI) P β SE OR(95%CI) P 第1四分位 — — — — — — — — — — — — 第2四分位 0.716 0.522 2.046(0.735~5.694) 0.170 1.019 0.587 2.771(0.876~8.759) 0.083 0.695 0.678 2.004(0.531~7.563) 0.305 第3四分位 1.005 0.512 2.732(1.001~7.459) 0.050 1.385 0.568 3.994(1.313~12.148) 0.015 1.038 0.641 2.822(0.803~9.921) 0.106 第4四分位 2.022 0.484 7.557(2.929~19.495) < 0.001 2.303 0.547 10.008(3.428~29.221) < 0.001 1.648 0.744 5.199(1.210~22.337) 0.027 第1四分位数: LAD≤38 mm; 第2四分位数: LAD>38~42 mm; 第3四分位数: LAD>42~47 mm; 第4四分位数: LAD>47 mm; 模型1: 不包含协变量; 模型2: 根据模型1,加入性别、BMI、糖尿病病史、高血压病史、冠心病病史、心力衰竭病史协变量进行调整; 模型3: 根据模型2,加入CRP、LVEF、LVDd、IVSTd、房颤类型协变量进行调整。 -
[1] BAMAN J R, PASSMAN R S. Atrial fibrillation[J]. JAMA, 2021, 325(21): 2218. doi: 10.1001/jama.2020.23700
[2] LIPPI G, SANCHIS-GOMAR F, CERVELLIN G. Global epidemiology of atrial fibrillation: an increasing epidemic and public health challenge[J]. Int J Stroke, 2021, 16(2): 217-221. doi: 10.1177/1747493019897870
[3] WIJESURENDRA R S, CASADEI B. Mechanisms of atrial fibrillation[J]. Heart, 2019, 105(24): 1860-1867. doi: 10.1136/heartjnl-2018-314267
[4] 中华医学会心电生理和起搏分会, 中国医师协会心律学专业委员会, 中国房颤中心联盟心房颤动防治专家工作委员会. 心房颤动: 目前的认识和治疗建议(2021)[J]. 中华心律失常学杂志, 2022, 26(1): 15-88. [5] KASHANI K, ROSNER M H, OSTERMANN M. Creatinine: from physiology to clinical application[J]. Eur J Intern Med, 2020, 72: 9-14. doi: 10.1016/j.ejim.2019.10.025
[6] WANG Y N, YANG Y, HE F. Insights into concomitant atrial fibrillation and chronic kidney disease[J]. Rev Cardiovasc Med, 2022, 23(3): 105. doi: 10.31083/j.rcm2303105
[7] PATEL R B, FONAROW G C, GREENE S J, et al. Kidney function and outcomes in patients hospitalized with heart failure[J]. J Am Coll Cardiol, 2021, 78(4): 330-343. doi: 10.1016/j.jacc.2021.05.002
[8] BARASHI R, HORNIK-LURIE T, GABAY H, et al. Renal function and outcome of patients with non-valvular atrial fibrillation[J]. Eur Heart J Acute Cardiovasc Care, 2021, 10(10): 1180-1186. doi: 10.1093/ehjacc/zuab075
[9] 米琴, 郭雪娅. 心房颤动与慢性肾脏病相关性研究[J]. 中华老年心脑血管病杂志, 2019, 21(2): 204-206. doi: 10.3969/j.issn.1009-0126.2019.02.025 [10] RIMMELE D L, BOROF K, JENSEN M, et al. Association between carotid atherosclerosis and atrial fibrillation, cardiac, and renal function[J]. Eur J Vasc Endovasc Surg, 2022, 63(4): 641-647. doi: 10.1016/j.ejvs.2022.01.010
[11] HU Y F, CHEN Y J, LIN Y J, et al. Inflammation and the pathogenesis of atrial fibrillation[J]. Nat Rev Cardiol, 2015, 12(4): 230-243. doi: 10.1038/nrcardio.2015.2
[12] TAPOI L, URECHE C, SASCAU R, et al. Atrial fibrillation and chronic kidney disease conundrum: an update[J]. J Nephrol, 2019, 32(6): 909-917. doi: 10.1007/s40620-019-00630-1
[13] KOZBERG M G, PEROSA V, GUROL M E, et al. A practical approach to the management of cerebral amyloid angiopathy[J]. Int J Stroke, 2021, 16(4): 356-369. doi: 10.1177/1747493020974464
[14] FLORIA M, TANASE D M. Atrial fibrillation type and renal dysfunction: new challenges in thromboembolic risk assessment[J]. Heart, 2019, 105(17): 1295-1297. doi: 10.1136/heartjnl-2019-315212
[15] PARK S, LEE S, KIM Y, et al. Atrial fibrillation and kidney function: a bidirectional Mendelian randomization study[J]. Eur Heart J, 2021, 42(29): 2816-2823. doi: 10.1093/eurheartj/ehab291
[16] VAN DER BURGH A C, GEURTS S, IKRAM M A, et al. Bidirectional association between kidney function and atrial fibrillation: a population-based cohort study[J]. J Am Heart Assoc, 2022, 11(10): e025303. doi: 10.1161/JAHA.122.025303
[17] GENG T T, WANG Y, LU Q, et al. Associations of new-onset atrial fibrillation with risks of cardiovascular disease, chronic kidney disease, and mortality among patients with type 2 diabetes[J]. Diabetes Care, 2022, 45(10): 2422-2429. doi: 10.2337/dc22-0717
[18] 张爱丽, 侯旗旗, 韩全乐, 等. 中国北方人群心房颤动与新发慢性肾脏病发病风险的相关性研究[J]. 中国全科医学, 2023, 26(36): 4521-4526. doi: 10.12114/j.issn.1007-9572.2023.0006 [19] DING W Y, GUPTA D, WONG C F, et al. Pathophysiology of atrial fibrillation and chronic kidney disease[J]. Cardiovasc Res, 2021, 117(4): 1046-1059. doi: 10.1093/cvr/cvaa258
[20] LÓPEZ-GALVEZ R, RIVERA-CARAVACA J M, ROLDÁN V, et al. Imaging in atrial fibrillation: a way to assess atrial fibrosis and remodeling to assist decision-making[J]. Am Heart J, 2023, 258: 1-16. doi: 10.1016/j.ahj.2022.12.007
[21] THOMAS L, ABHAYARATNA W P. Left atrial reverse remodeling: mechanisms, evaluation, and clinical significance[J]. JACC Cardiovasc Imaging, 2017, 10(1): 65-77. doi: 10.1016/j.jcmg.2016.11.003
[22] MILLS H, ESPERSEN K, JURLANDER R, et al. Prevention of sudden cardiac death in hypertrophic cardiomyopathy: risk assessment using left atrial diameter predicted from left atrial volume[J]. Clin Cardiol, 2020, 43(6): 581-586. doi: 10.1002/clc.23351
[23] THOMAS L, MURARU D, POPESCU B A, et al. Evaluation of left atrial size and function: relevance for clinical practice[J]. J Am Soc Echocardiogr, 2020, 33(8): 934-952. doi: 10.1016/j.echo.2020.03.021
[24] BEYER C, TOKARSKA L, STÜHLINGER M, et al. Structural cardiac remodeling in atrial fibrillation[J]. JACC Cardiovasc Imaging, 2021, 14(11): 2199-2208. doi: 10.1016/j.jcmg.2021.04.027
[25] GOETTE A, LENDECKEL U. Atrial cardiomyopathy: pathophysiology and clinical consequences[J]. Cells, 2021, 10(10): 2605. doi: 10.3390/cells10102605
[26] NGUYEN H T T, DO C V, DANG D T V, et al. Progressive alterations of left atrial and ventricular volume and strain across chronic kidney disease stages: a speckle tracking echocardiography study[J]. Front Cardiovasc Med, 2023, 10: 1197427. doi: 10.3389/fcvm.2023.1197427
[27] CHEN S C, CHANG J M, TSAI Y C, et al. Left atrial diameter and albumin with renal outcomes in chronic kidney disease[J]. Int J Med Sci, 2013, 10(5): 575-584. doi: 10.7150/ijms.5845
[28] HUANG T H, CHIU H, WU P Y, et al. The association of echocardiographic parameters on renal outcomes in chronic kidney disease[J]. Ren Fail, 2021, 43(1): 433-444. doi: 10.1080/0886022X.2021.1885444
[29] HU L L, XIONG Q M, CHEN Z Q, et al. Factors associated with a large decline in renal function or progression to renal insufficiency in hospitalized atrial fibrillation patients with early-stage CKD[J]. Int Heart J, 2020, 61(2): 239-248. doi: 10.1536/ihj.19-205
-
期刊类型引用(10)
1. 唐丽欣,郭雨栋,李士学,唐秀芬. 利那洛肽联合复方聚乙二醇电解质散肠道准备改良方案的随机对照研究. 中华消化内镜杂志. 2025(02): 120-124 .  百度学术
百度学术
2. 张超群,刘梦丽,姬娟娟,杜学芳,宋雅璇,王玉玉,张彩凤. 不同清肠药物对肠道准备情况及肠道群菌的影响. 医药论坛杂志. 2025(05): 548-552 .  百度学术
百度学术
3. 钟佳燕,姜丽英,严兰婷,朱燕勤. 通便散脐部贴敷配合聚乙二醇电解质在结肠镜检查前肠道准备中的应用. 新中医. 2024(10): 151-154 .  百度学术
百度学术
4. 郭存果,傅思华. 利那洛肽联合复方聚乙二醇电解质应用于老年慢性便秘患者肠道准备的效果评价. 中国医药导报. 2024(14): 95-97 .  百度学术
百度学术
5. 李松琳,许佳阳. 老年人结肠镜术前肠道准备用药研究进展. 吉林医药学院学报. 2023(03): 208-210 .  百度学术
百度学术
6. 任霜霜,陆启峰,杨如雪,孙璐宇. 利那洛肽联合聚乙二醇对比番泻叶联合聚乙二醇在便秘病人肠道准备中的应用. 安徽医药. 2023(12): 2525-2528 .  百度学术
百度学术
7. 惠逸帆,赵硕琪,凌亭生,李柳,张烨,顾立梅,廖星,程海波. 结直肠腺瘤中西医结合防治指南. 中国中药杂志. 2023(23): 6269-6277 .  百度学术
百度学术
8. 陈振东. 中医药用于消化内镜检查前肠道准备的研究进展. 甘肃高师学报. 2022(02): 39-42 .  百度学术
百度学术
9. 刘芳. 胃肠镜视野清晰度增强仪在结肠镜检查中的应用. 医疗装备. 2022(10): 172-173 .  百度学术
百度学术
10. 林国敏,周文强. 盐酸达克罗宁胶浆对结肠镜检查中肠镜视野及去泡效果的影响. 深圳中西医结合杂志. 2022(22): 119-121 .  百度学术
百度学术
其他类型引用(5)




 下载:
下载:
 苏公网安备 32100302010246号
苏公网安备 32100302010246号
